eISSN: 2469-2794


Review Article Volume 5 Issue 3
Department of Science and Technology Nottingham Trent University, UK
Correspondence: Andrew OHagan, Department of Science and Technology, Nottingham Trent University, Nottingham, UK, Tel 44115-8483153
Received: September 13, 2017 | Published: September 15, 2017
Citation: Hagan AO, Smith C (2017) A New Beginning: An Overview of New Psychoactive Substances. Forensic Res Criminol Int J 5(3): 00159. DOI: 10.15406/frcij.2017.05.00159
New psychoactive substances are the newest danger trending on the drug market. Though they are defined as substances designed to replicate the effects of traditional illegal drugs such as cocaine, ecstasy, amphetamines and cannabis, it has been suggested that these mimics are extensively more potent than their counterparts. Beyond the limits of current legislation, clandestine chemists have set out to manufacture these substances for profit, whilst benefitting users in areas of affordability, availability and purity. Since the rediscovery of mephedrone in 2003 and more so in recent years, the manufacture and sale of these substances has soared. Due to the rate at which these ever-increasing analogues are being manufactured, and the endless number of combinations available for production, it is unlikely the trade will be reduced in the near future. This review provides an overview of these new substances addressing; what they are, when they were produced, where they are available, how they are manufactured, who is taking them and why users are resorting to these substances over traditional substances. It is clear throughout this review that the lack of information surrounding these substances is leading to increased risks to users, untrained healthcare and forensic professionals and ineffective legislation. Welcome to, a new beginning.
Keywords: New psychoactive substances; Legal highs; Head shops; Clandestine chemistry; Law enforcement
The emerging and adapting world of New Psychoactive Substances (NPS) is creating devastating effects on users worldwide. This trade is becoming so advanced that it has the potential to continuously evade the law, inflicting danger, addiction and in some cases death on users. New psychoactive substances have been in continuous production by clandestine chemists since as early as 1929, when mephedrone was first produced.1 However, the increase of NPS to a recorded number of more than 560 substances notified to the European Union Early Warning system (EUEWS) in 2015, has raised major concern.2 By altering chemical structures of the active ingredients found in traditional drugs, chemists can create new analogues, which can be legally traded provided they are not sold for human consumption. These substances are widely available and commonly accessed from sources such as High Street and Non-High Street retailers including head shops (HS) where they are sold as ‘bath salts’, ‘research chemicals’, ‘plant food’ and ‘incense’. Other sources include friends, family members and colleagues.3,4 Along with this personal level of distribution, the availability of these substances on the internet by the number of online shops, has dramatically increased in the European Union (EU) from 170 in 2010 to 693 in 2012.5 This increase of internet usage has diversified and expanded global boundaries, creating a new, anonymous and impersonal platform of availability to potential users.6 The main factors which make NPS so popular are their affordability, availability, high purity and ‘portrayed’ legality. All of these factors make it extremely beneficial for drug users to convert from traditional drug use to NPS, along with new users being introduced to drugs, due to their vulnerability, curiosity and potential avoidance of prosecution.
The Psychoactive Substances Act 2016 (PSA), has been recently introduced in an attempt to control the production and supply of these substances, subjecting an offending individual to a maximum of seven years’ imprisonment.7 Though this bill was intended to decrease the number of HS and websites selling NPS, and as a result decrease the number of individuals using these substances, other professionals criticise the bill. They state that it has the potential to drive NPS underground into a more complex, hidden territory, creating more issues than those currently being faced.8 The majority of these issues relate to the increase in the number of deaths, the ongoing production and uncertainty of new substances, and the lack of knowledge and training in healthcare professionals. This review delves into the depths of the topics mentioned, and discusses the overall nature, availability, manufacture and issues of these substances, as well as considering potential users, their effects and the recent legislation attempting to control their use.
What are legal highs?
New psychoactive substances, colloquially known as ‘legal highs’, are synthetic substances engineered to replicate the effects of illegal drugs like cocaine, ecstasy, amphetamines and cannabis.3,9 These ‘legal highs’ are designed with the intention to avoid legislation, by changing compounds within illegal substances to reproduce new ones, that yield similar effects to their illegal counterparts. As a result of this clandestine chemistry, these new substances are not controlled under the Misuse of Drugs Act 1971 (MDA). Before the PSA, it was not against the law to produce, distribute or supply NPS if they were labelled ‘not for human consumption’. Therefore, until 2016, they were available to purchase in HS that specialise in these NPS and drug paraphernalia.4 Within these HS NPS are commonly retailed as unsuspected substances and are packaged in attractive packets, with piercing identities such as, Spice, China White and Benzo Fury to name a few (Figure 1).3,4 Based on the type of substance, they are purchased in a variety of forms including pills, liquids, powders, capsules, and smoking blends and can be ingested orally, snorted, smoked, or injected.3 (Figure 2). Because new psychoactive substances are derivatives of other controlled substances, there is almost an infinitive number of combinations that can be manufactured to deem a substance ‘legal’ as a result, making them extremely difficult to control.

Figure 1 Different names and brightly coloured packaging of ‘legal highs’.10

Figure 2 The variety of forms of NPS.11
Classification:ike many drugs controlled under the MDA, the classification of NPS allows them to be sub-divided into categories that aid in the identification of their chemical structure, pharmacological mechanisms or psychological effects.12 The main categories are; stimulants, depressants, psychedelics, and synthetic cannabinoids (Table 1). These can vary based on how substances are classified.9-18
|
Classification |
Information |
Effects |
|
Stimulants |
Operate on the nervous system. Increase the risk of heart disease, and disrupt circadian rhythms.9 Are synthetic cathinone’s, which contain chemicals related to cathinone that naturally occur in the khat plant. They are either swallowed, snorted or injected.13 |
Effects include, mood enhancement, increased blood pressure, body temperature and energy, a sense of euphoria, suppression of appetite and psychedelic effects such as hallucinations, paranoia and anxiety. |
|
Depressants |
Depressants slow down the nervous system and produce inhibitory effects on the brain. |
The effects cause the user to feel relaxed, care-free and occasionally sedated.9 |
|
Psychedelics |
Manufactured to mimic the effects of an illegal drug known as LSD. Users become aware of subconscious thoughts and feelings, and exert challenges in coping with concepts such as, fantasies, life circumstances and fears.14 Can make users hallucinate and experiences vary in relation to their surrounding.9,14 |
The main effects are, increased blood pressure, body temperature and breathing rate, problems with circadian rhythms, spiritual and sensory experiences, excessive sweating, feelings of relaxation, paranoia and nausea.15 |
|
Synthetic cannabinoids |
Smoking blends primarily designed to mimic the psychoactive component known as delta-9-tetrahydrocannabinol (THC) present in the illegal substance, cannabis.16,17 They earned their name by their effhect on the cannabinoid receptors in the brain. The most well-known series is the JWH series.18 |
The main effects are relaxation, elevated mood, rapid heart rate, altered perception and symptoms of psychosis. They are reported to be significantly stronger and more dangerous than their illegal counterpart and can also induce nausea, aggression, seizures and respiratory failure.16,18 |
Table 1 Classification, effects and examples of NPS
Where did they come from?
Production lines: An example of the rise of NPS was in 1979 when the sophistication of substance production reached new heights.19 In Orange County of California, two overdose deaths were reported. Both victims had a consistent history of heroin abuse, but when toxicological analysis was conducted, the results showed no trace of drugs.19 Following these deaths, in 1980 a total of fifteen deaths were recorded and similarly, no trace of drug use was apparent. As a result of this suspicion, law enforcement officials seized street samples sold as heroin, and found the substance was absent of any known drug. It was identified as alpha-methylfentanyl, a potent narcotic that had not undergone scientific evaluation. Though the substance produced very similar effects to fentanyl, it was classified as a new substance and was not lawfully controlled.19
Additionally, in the Cambodian Rainforest, concealed illegal factories are utilised for turning sassafras oil, extracted from the roots of the Mreah Prew Phnom Tree, into a precursor chemical known as methylenedioxymethamphetamine, commonly known as the illegal substance, ecstasy.20 The authorities from Cambodia and Australia decided to take action on these ecstasy laboratories and in 2008, 30 tons of sassafras oil were destroyed. It was estimated that this amount of sassafras oil could have been used to produce 245 million doses of ecstasy, equating to a street value in the US of $7 billion.1 As a result of this destruction, the dealers and street sellers who already had demands from club users, had to invest money into finding alternatives to traditional ecstasy. Consequently, chemical substances such as piperazines, which imitate the effects of ecstasy were produced.1 These new substances proved popular with users as not only were they cheap, accessible and higher in purity, they were legal.1
Mephedrone: Mephedrone, also known as ‘M-cat’, ‘Meth’ and ‘Moonshine’ was first synthesised in China in 1929, but laid dormant until it was rediscovered in 2003.1 It is a phenethylamine and cathinone derivative, which cross-links its psychoactive effects with ecstasy, cocaine and amphetamines and is primarily sold as a white powder or capsules (Figure 3).1,21 Because of its manufacture and lack of clinical analysis, it was not controlled by the MDA or the Medicines Act 1968. The use and interest in mephedrone took a rapid increase due to its 99% purity and affordable nature at only £10 a gram. This increase was also suspected to be linked with the decreasing purity of traditional stimulants like cocaine and ecstasy.4,22 By 2008, mephedrone was linked to numerous fatalities. These deaths alerted law enforcement agencies and by 2010, mephedrone was made illegal in the UK.4 In a study conducted by the University of London in 2012, mephedrone victims were characteristically under the age of 35 (78%), male (75%), white (96%) and in full time employment or students (73%).22 It was fast tracked through parliament and classified as a Class B drug, making it illegal to produce, supply or possess; possession alone subjecting an individual to a maximum of five years’ imprisonment.4,23,24
Figure 3 Mephedrone - white powder form.24
Within two years prior to the ban, mephedrone had become the fourth most popular drug behind cannabis, cocaine and ecstasy.1 The surge in mephedrone use and the increased publicity regarding NPS, meant it had gained a position in the market. The production and retail of new substances has rapidly expanded, and online stores and HS selling NPS in Europe have thrived. In January 2010, 170 online stores were recorded and by 2014 this value had escalated to almost 1,000.1 Furthermore, though mephedrone is now banned, it will have consequently been driven underground, regaining a new market in illicit drug trades, increasing its value and demand.
The global increase: According to the European Monitoring Centre for Drugs and Drug Addition (EMCDDA), in the last five years, 368 NPS have been recorded, with 98 new substances alone accounting for 2015. This results in the number of NPS notified to the EUEWS for the first time to be >560, with synthetic cannabinoids being the dominating group.2 (Figure 4). Furthermore, the increasing growth of new drugs on the market has created an increase in the number of seizures according to the EUEWS. The EUEWS was introduced to identify, record and monitor NPS that emerge. In the UK annual report of 2014/15, 1,345 of the samples seen were not controlled, and of these numbers 4 NPS have been identified, equating to 35 new identified samples through this system.25 On a European scale, there were ~50,000 seizures in 2014 in relation to new substances across Europe, with the majority being synthetic cannabinoids (30,000) followed by synthetic cathinones (8,000) and other groups such as fentanyls and benzodiazepines.2 (Figure 5). On a global scale, information collected by the United Nations Office on Drugs and Crime (UNODC) in 2012 based on the global spread of NPS, received 240 responses from 80 countries.26 Of all the countries, 70 reported that NPS had emerged on the market, with their appearance in Europe accounting for 31 of the countries. The results were followed by other countries including Asia (19 countries), America (11 countries), Africa (seven countries) and Oceania (two countries).26 (Figure 6).
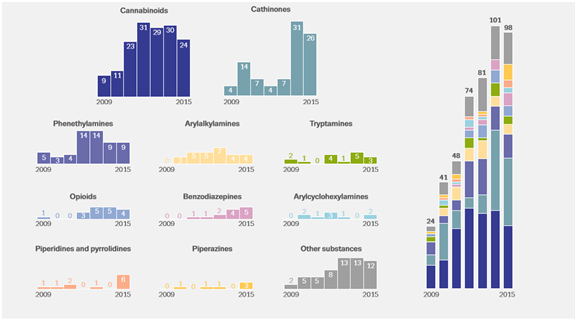
Figure 4 Number and categories of NPS notified to the EU Early Warning System for the first time, 2009-15.2

Figure 5 Number of seizures of NPS reported to the EU Early Warning System trends and by category in 2014. Reproduced from the EMCDDA European Drug Report, 2016.2
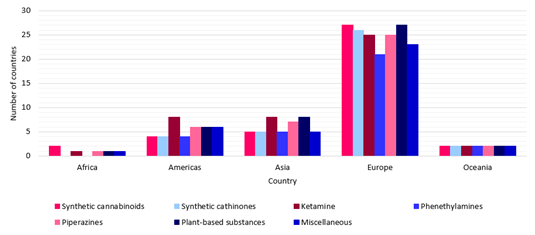
Figure 6 Regional emergence by NPS group. Modified from the United Nations Office on Drugs and Crime 2013,.26
How are they manufactured?
Clandestine chemists are the source of manufacture for NPS both illegal and legal.27 Since the late 1970s, illicit laboratories have been utilised to synthesise designer drugs that imitate the pharmacological effects of controlled substances, by altering the chemical structure enough to escape legislation controls.27 These laboratories are mainly based in Far Eastern countries such as China and Indonesia, along with other countries including Israel and Holland. China, was originally a country which exported the ‘research chemicals’ to the manufacturers. However, recently, after witnessing the profitable nature of NPS, they have claimed the business and increased the production of toxic substances to maximise their income. Furthermore, organised crime groups desire a piece of this business due to the recent depletion in traditional drug use by NPS. This produces a continuous shift towards these substances so traditional criminals can establish their own market in this trade.1 Because of their lack of definition, chemical constituents utilised to manufacture such compounds, require very small alterations that completely legalise them. As a result, an endless variety of these analogues can be designed, produced and distributed efficiently to users.27
Focusing specifically on the manufacture of synthetic cannabinoids, the main active compound mimicked is named THC.27 The first ‘classical cannabinoid’ analogue of THC that was synthesised in Israel in 1988 was ‘HU-210’ (Figure 7) and following this, a whole range of cannabinoid families that are structurally dissimilar to THC were produced, including both non-classical and aminoalkylindoles.26 Aminoalkylindoles are divided into other categories, and constitute of the JWH-compounds named after Professor John William Huffman, JWH-018 being the most common. These JWH-compounds are the most widespread and well-known synthetic cannabinoids, and their potency has been measured as three times more than the original active substance.27,26 Dr. Zee is an Israeli chemist that holds the status of ‘the godfather’ of legal highs. Like other chemists, he controls the chemical structure of substances and manufactures them weekly. Meanwhile, he is testing his substances to establish what effect (if any) they have on the human body and brain. He states, ‘I make molecule after molecule then try them without prejudice. You have to keep an open mind.’ And ‘That said, I have a great deal of knowledge that allows me to disqualify potential dangers’.28
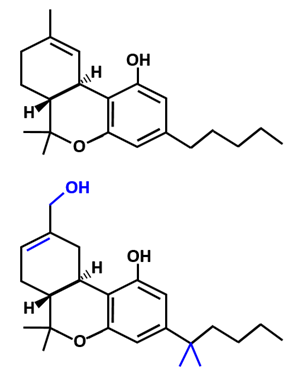
Figure 7 Chemical structure of classical cannabinoids delta-9-tetrahydrocannabinol (top), and of the synthetic cannabinoid HU-210 (bottom). The differences between the synthetic cannabinoid and the controlled substances tetrahydrocannabinol are highlighted in blue. Modified from United Nations Office on Drugs and Crime 2013.26
How are they distributed and where are they available?
Due to the accessibility of chemicals and the simplicity and diversity of manufacture, the distribution of NPS is endemic. Chinese laboratories and to a lesser extent, India, supply large quantities of final products and intermediate chemicals required for the manufacture of NPS.29 In a UNODC questionnaire on NPS in 2012, the trafficking of these substances was found to be by air (30 countries) or by mail (24 countries).26 When they reach their destination, commonly countries in the EU or America, they are either repackaged and redistributed by retailers using online or offline services, or are delivered to the UK directly.30 The availability of these products once they reach their final destination is vast, but mainly falls into three categories.29,30
Internet
The internet has become a global marketplace for the selling of NPS. The emergence and growth of this community is becoming concerning for control agencies, with the EU number of online shops selling NPS increasing from 170 in 2010 to 693 in 2012.5 NPS are sold on both the ‘clear net’ which deals with non-controlled substances and the ‘dark net’ which deals with controlled substances. Both platforms are accessed by different customers and thus, diversifies and expands boundaries of drug supply, creating more opportunities for the availability and distribution of these products.6,30 Eradicating personal interactions between the user and drug dealer provides comfort to the majority of young people interested in purchasing, as the electronic interactions offer a safer alternative.29 The National Crime Agency (NCA) has estimated that in the UK there are between 100 and 150 websites on the ‘clear net’ that sell non-controlled NPS.30 After introductions of control measures such as legislation, in an effort to regulate their supply, the transfer of sales onto the ‘dark net’ has erupted and creates a further platform for the increase in sale and availability.6,30
For example, in the Global Drug Survey 2015 (GDS), the proportion of respondents who bought certain types of drugs on the ‘dark net’ between November and December 2014 was recorded. Though the majority of the drugs purchased on the ‘dark net’, as expected, were traditional illegal drugs, illegal NPS substances still contributed to a portion of the market (Figure 8).31 The ‘dark net’ supplies a further ‘security blanket’ as it allows customers to purchase illegal substances with anonymity and personal safety, by hiding identities through anonymisation services.6,29 A common example is ‘The Onion Router’, which conceals computer IP addresses of those accessing the site, and leaves them relatively untraceable.29,31 The encrypted payment methods, better known in the drug community as ‘cryptocurrencies’, used by these services include, bank transfers, e-money and virtual currencies including, bitcoin and litecoin.6,30 Arguably, offenders claim they show no interest in moving to the ‘dark net’ to advertise their products, as their risk of being caught on the ‘clear net’ is slim.6
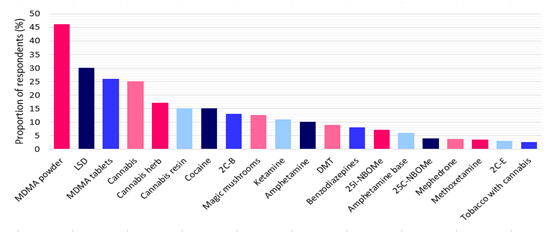
Figure 8 Drugs purchased on the ‘dark net’, by types of drug, 2014. Modified from the New psychoactive substances review report of the expert panel. Home Office 2014.31
The development of the ‘clear net’ community has opened access for websites, chatrooms, blogs, forums and instant messaging. This increase in communication, has meant that potential customers are able to access information on; places to buy, prices, how to activate substances, how to manufacture substances, as well as feedback on other user’s experiences with specific products.6 Despite these factors making the drug market a more approachable platform, positivity may stem from this as forums providing advice, ratings on sellers and products, has the potential to reduce negative reactions to ‘faulty’ batches.6 This accessible information appears attractive to younger generations, and in a survey conducted by the European Commission in 2008 amongst 15-24 year olds in the EU, the internet (61%) was shown to be the most popular source for information, followed by friends (35%), health professionals (24%), relatives (27%) and drug counsellors (25%).32 Additionally, the number of EU 15-24 year olds who looked to the internet for information around NPS increased from 30% to 64% between 2001 and 2011.5
The availability of NPS online is vast, however it has a high level of variability and frequently fluctuates as a response to evolving legislation and customer demand.29. Continuous monitoring of drug-related websites has proven difficult because of this factor. An example of this variation is from the online sale of mephedrone which showed a dramatic growth from 2008 to 2010 in Europe. It was recorded in March 2008 that there were <10 online vendors selling mephedrone but following this, new sites were appearing weekly and the number of UK students purchasing mephedrone from the internet, prior to the introduction of UK control legislation in April 2010, was 10.7%. When mephedrone was eventually banned in 2010 the online availability of mephedrone plummeted from 33% to 1% and the rise of street dealers began.29.
High-street retailers: High-street retailers relate primarily to Head Shops. Head Shops are stores that specialise in drug paraphernalia. Prior to May 2016, they were widespread on the streets and were able to evade the law by stating products were ‘not for human consumption’, even though in most cases discussions around consumption are common. The number of HS in the UK is unknown. However, by searching the internet and retrieving information from trading standard offices, the Angelus foundation estimated that there are >250 in the UK alone (Figure 9).30,33 In addition, the Home Office have also recorded that 450 HS and online sellers in the UK selling NPS say they contribute to the majority of their income.34 However, sources including the NCA national strategic assessments state, the introduction of the PSA, will cause the sale of NPS in stores to dramatically shift to online distribution, because of the fear of prosecution from street sale.35,36,37

Figure 9 Head shop selling NPS in Brighton Carl Court.37
Non-retail vendors: Non-retail vendors are classified as ‘street dealers’ who obtain their products from the internet or high-street retailers and sell them for their own profit in clubs, schools, at music festivals and on the street.29 An example of an individual dealer named Denny indicates, that though the trade is popular on the internet and in HS, traditional dealers can still operate effectively. Denny opened his business in 2012 and claims he has 300 customers buying his products every week. His method of sale intrigues customers as his products are available 24/7 with an offer of ‘delivery service’, much like ordering fast food.4 Occasionally, customers may prefer this method of sale, as the potential of being scammed is much slimmer than when purchasing online.4
In the 2015/16 Crime Survey for England and Wales (CSEW), respondents were asked questions relating to NPS use. One of these questions related to how they obtained the drugs in their last instance of drug use. Based on the responses, it was found that over a third of the individuals obtained the drug from either their friend, neighbour or colleague (35%), followed secondly by a shop (25%), a known dealer (9%) and other means of access, with the internet only equating to 8% (Figure 10).38 Alternatively, it was found by the GDS in 2016 that online was the most popular source (50.5%) followed by friends (29.2%), shops (23.7%) and dealers (15.2%) (Figure 11).39 This suggests that globally NPS are primarily sourced online. Overall, it is clear that all methods of distribution for NPS are effective in their purpose, but the variability of the most popular system is highly dependent on external factors including, market pressures, demographic characteristics and demand.
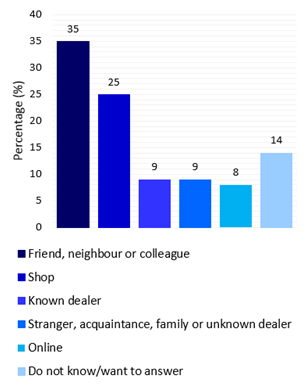
Figure 10 Source of NPS used on the last occasion, by adults aged 16-59. Modified from the 2015/16 Crime Survey for England and Wales.38
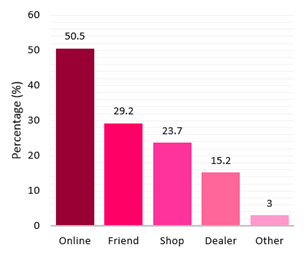
Figure 11 Source of NPS. Modified from the Global Drug Survey 2016.39
Who, why and what are the effects?
NPS are attractive to users due to their availability, low cost and legal nature, but questions are raised in relation to, who consumes them? Why? And most importantly, what effects are they having on individuals?.34 It was found in 2013/14 by the CSEW, that 83% of users of an NPS known as ‘Salvia’ had used an illicit substance in the previous year, with 73% taking cannabis, 37% taking ecstasy and 33% taking cocaine.40 This finding was also supported by the CSEW in 2015/16 where 84.9% of NPS users had used another substance in the previous year.38 These results suggest that the majority of NPS users are already existing drug users. However, it has been discovered that naïve, new drug users that are absorbed into the drug trade by the false statements and misinterpretations of NPS, are also using these substances despite their lack of engagement in illicit drug-taking.40 Additionally, it has been found by the CSEW in 2015/16 that the use of NPS in the previous year was concentrated to young, vulnerable individuals aged 16-24, overall equating to 2.6% of the young adult population. This value is three times higher than the value among the wider age group. Furthermore, it has been found that approximately twice the number of males were more likely to have used NPS than females (Figure 12).38 The higher use of NPS in young adult populations (16-24 year olds) as opposed to the wider age group (16-59 year olds), could be as a result of lifestyle factors such as increased levels of alcoholism and exposure to ‘club cultures’. For example, it was also proven by the CSEW that individuals who had increased visits to nightclubs, pubs or bars in the previous year were more likely to have used NPS, and likewise with individuals who had consumed alcohol more than once in the previous month (Table 2).38
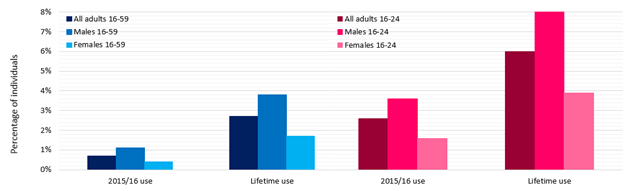
Figure 12 Prevalence of NPS use in 2015/16 and the adult’s lifetime, by sex and age. Modified from the 2015/16 Crime Survey for England and Wales.38
|
Variables |
Age |
|
|
Adults 16-59 |
Adults 16-24 |
|
|
No visits to a nightclub or disco in the last month |
0.40% |
1.60% |
|
Visited a nightclub or disco in the last month 1-3 times in the last month 4+ times in the last month |
2.70% |
4.60% |
|
2.30% |
4.20% |
|
|
4.30% |
5.60% |
|
|
Did not consume alcohol in the last month |
0.40% |
1.00% |
|
Consumed alcohol once or more in the last month Less than a day a week in the last month 1-2 days a week in the last month 3+ days a week in the last month |
1.00% |
3.80% |
|
0.70% |
2.20% |
|
|
1.00% |
3.70% |
|
|
1.10% |
6.90% |
|
Table 2 Percentage of NPS use in 2015/16 by frequency of visits to a nightclub or disco and alcohol consumption in the last month, 16-59 and 16-24 year olds, 2015/16 CSEW. Modified from the 2015/16 Crime Survey for England and Wales.38
There are a range of possibilities why individuals consume these substances and it is commonly alleged that because they are termed ‘legal’, the misconception of legality portrays ‘safety’, consequently, encouraging their popularity and reducing the perception of risk.41 Despite this idea of ‘safety’, it has been found in an online survey conducted by Corazza et al..21, on 446 students aged 13-30, that NPS are purchased due to their enjoyable effects (55.7%), easy availability (45.7%), enhanced sociability (35%) and affordability (28.6%), opposed to a view of ‘safety’ in comparison to more traditional drugs.42 For example, 74.2% of the students do not consider NPS to be safer than their illegal counterparts (Figure 13).42 In a survey conducted by the GDS (2016) on 101,313 participants in >50 countries, 6,015 being from the UK, aspects of value-for-money and online availability, were the two most popular motivators for NPS use.43 In another generic drug user survey conducted by Boys (2001) on 364 young poly-drug users, the most significant reasons for drug use were found to be, to relax (96.7%), to become intoxicated (96.4%), to stay awake at night while socialising (95.9%), to enhance activity (88.5%) and to alleviate depressed mood (86.8%).44
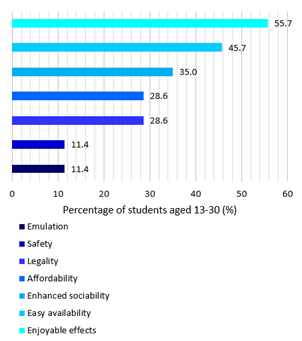
Figure 13 Reasons for taking NPS. Modified from Corazza et al..42
Awareness and risk association of NPS are factors that have the potential to produce a large impact on the population. Most individuals fail to understand aspects relating to the nature and probable dangers of NPS, possibly because of a lack of factual advertisement. It is known that; they are not approved for human consumption, they are unknown to health and other professionals so it is unlikely individuals will receive the correct treatment, they have rarely been studied in scientific literature so the majority of the compounds and effects on the body are unknown, and they are regularly advertised as ‘legal’ and ‘safe’. It is common amongst consumers that the legality of the substances is misinterpreted by their easy availability, and users are unaware that substances they are consuming have an illicit status.45 For example, in a self-report survey conducted in 2012 on 2,346 undergraduate students in the United States, approximately 1/3 of the sample inaccurately believed that synthetic cannabinoids such as Salvia divorum (34.7%), K2/Spice (36.5%), and Pot-pourri (32.1%) were legal in the state. Additionally, over half (50.3%) inaccurately believed that synthetic cathinones were legal in the state.45 This delusion is claimed to be due to factors such as the media, which can be a generic issue worldwide. The media commonly narrow their focus to newer substances, which are often legal due to their lack of classification, re-emphasising the products as ‘legal highs’. Because focus is deviated from substances that are undergoing illegalisation, it is common that all ‘legal highs’ are perceived as legal when this is not always the case.45 As a result, these substances are affecting individuals due to these erroneous beliefs and usage decisions based on inaccurate declarations.
Though death rates involving NPS are small, they have increased rapidly throughout recent years from 10 in 2009 to 68 in 2012. Overall, there have been 76 deaths related to NPS in England and Wales between 2004 and 2013, with the average age at death being 28.46,47 The average age for drug misuse deaths is 38 years, so emphasis from other research that NPS use is concentrated in younger population is supported. Though several short-term effects of NPS are known such as, agitation, paranoia, psychosis, hypertension, elevated temperature and seizures, many long-term harms are unknown and though re-occurring death rates demonstrate obvious indicators of their danger, users continue to play ‘Russian-roulette’ with their lives.47 For example, a 26-year-old named Richard, took a now banned legal high known as the N-bomb, which is manufactured to imitate the illegal substance, Lysergic acid diethylamide (LSD).
After suffering from a bad reaction, doctors confirmed that a mixture of the N-bomb and alcohol induced a series of fits, leaving Richard severely brain damaged and dependent on 24-hour care. This effect on individuals proves that users are completely unsure of what they are taking, how much they should take and what effect it will have on their body, especially in conjunction with other substances.46,47 It was reported by researchers at St George’s University, that post-mortem test results from across the UK did not include all the examinations, so it is possible that not all coroners upload their data on causes of death. Therefore, the number of deaths that are linked to NPS is likely to be higher than those recorded.46
The law – psychoactive substances act, 2016
The PSA came into force on the 26th of May 2016. Psychoactive substances are defined as substances that produce a psychoactive effect within an individual. The act has made it an offence to produce, supply or offer to supply any of these products. However, substances which are exempt from this legislation include nicotine, alcohol, caffeine and medicinal products. Penalties relating to this offence can subject an individual to a maximum of 7 years’ imprisonment if they are caught offending (Table 3).7,48 Possession of a substance under this act is not an offence unless it is within a custodial institution such as, prisons, young offender’s centres, removal centres or service custody premises. The exemption of possession being an offence, prevents a vast amount of young people being criminalised without solving the primary issue relating to NPS. Other existing legislation including the MDA and the Human Medicines Regulation 2012 are unaffected by this act. However, the Intoxicating Substances Supply Act 1985 has now been removed.48
|
Offence |
Summary (Magistrates Court) |
Indictment (Crown Court) |
|
Possession |
Not an Offence |
Not an offence |
|
Possession in a custodial institution |
Up to 12 months and/or a fine |
Up to 2 years and/or a fine |
|
Possession with intent to supply |
Up to 12 months and/or a fine |
Up to 7 years and/or a fine |
|
Supply/offer to supply |
Up to 12 months and/or a fine |
Up to 7 years and/or a fine |
|
Production |
Up to 12 months and/or a fine |
Up to 7 years and/or a fine |
|
Importation/exportation |
Up to 12 months and/or a fine |
Up to 7 years and/or a fine |
|
Failure to comply with a prohibition/premises notice |
Up to 12 months and/or a fine |
Up to 2 years and/or a fine |
Table 3 Penalties under the Psychoactive Substances Act 2016. Modified from DrugWatch, 2016.48
The bill was actioned with the aim of working against the producers and sellers of NPS, aiming to reduce the numbers of shops and websites that supply these products. The government stated that subjecting producers and dealers to a possible 7-year sentence will emphasise the dangers of NPS and the number of people consuming them will decrease. However, several critics including Professor David Nutt, a British psychiatrist and neuropsychopharmacologist, who specialises in the research of drugs, argued that the ban will increase the death rates related to NPS, and the decrease of HS and websites supplying these substances will drive the sales of NPS underground.8,34 Additionally, our growing knowledge relating to the dosage and potency of these substances, has the potential to reach a standstill because of their movement into more explicit and hidden territory.
It has been suggested by Harry Sharpiro, the chief executive of drugs information from the DrugWise Charity, that the only people who will benefit from the ban are traditional drug dealers and organised crime groups, who will add the sale of NPS to their assortment. With this profit in mind, the street dealers will aim to convert NPS users to more traditional drugs such as heroin and cocaine, due to their significantly higher cost and higher level of additivity.8 The effects of this ban have also been expected to reflect those in Ireland when the ban was executed in 2010. Based on the Ireland National Drug-Related Death Index, since the ban the deaths involving NPS have increased from six in 2010 to 28 in 2013. Additionally, HS have benefitted researchers and professionals, as they have made it possible to track and monitor the substances sold to users, as well as the owners providing a level of quality control and responsibility towards their customers, unlike the average street dealer.8
It has also been found from a survey conducted by the National Youth Charity YMCA on >1,000 16-24 year olds, that regardless of the new legislation, 64% would still be likely to use these substances. Denise Hatton, the chief executive of the YMCA stated that in her experience, young individuals will not be impacted by the ban, and it will not achieve the necessary outcomes required to address the main concepts of the NPS issue. Furthermore, it has been emphasised by the YMCA that though the number of young people administering these substances is likely to decrease, they will continue to be unnecessarily harmed by NPS, and further education and community support is essential for a positive effect on young individuals to be attained.49
Issues
Though there have been huge attempts to inform the public and potential customers about the dangers of NPS, many still believe they are safe to consume. Predominant issues mainly highlighted are those regarding legislation, the uncertainty of available products and several medical implications.
Legislation: Issues relating to the broad range of substances that fall under the recent legislation is that they are almost impossible to categorically define, meaning harmful and harmless substances are not specified and all exemptions to the bill are not fully listed. Consequently, substances that could be of benefit to the community, such as herbal medicines or benign compounds, will be faced with the possibility of prosecution.50 Moreover, psych activity of a substance has no measurable deduction and therefore cannot be proven in court. Due to the legislation being based on the psychoactive effect of the substance on an individual, the only possible way of determining the effect is by the analysis of human experience, which cannot be legally documented for court.50
As proven before the bill came into action, the British government cannot legislate against NPS parallel to the rate at which they are being manufactured and as a result, many substances have been produced that evaded and continue to evade the law. Now that the Act has become part of British legislation, chemists have had to devise a different system in which NPS can still be produced without the fear of prosecution.28 Dr. Zee, has succeeded in doing this by creating a modernised drug-related ‘coffee machine’, which he has named the ‘Methspresso’. This machine allows Dr Zee to produce and supply recreational drugs within the boundaries of the new legislation. He intends to manufacture non-psychoactive compounds that his customers can convert into psychoactive compounds at home, by heating up the substances in hydrochloric acid for six hours and legally obtain what was available to purchase in HS and over the internet prior to the ban.28 This again, produces another issue for the government to act against. Overall, it is clear that the government is failing to control NPS use and are displacing drug use as opposed to reducing it.51
Uncertainty of the products: Another range of issues deriving from the manufacture and sale of NPS, is the overall uncertainty of the products. The Laboratory of Environmental Hygiene and Forensic Toxicology (LIAFT) has proven, by analysing three case reports taken from the archive of processed cases, that NPS contain high variability in the quantity of an active ingredient, the number of active ingredients, and the ingredients themselves within various products.52 For example, on analysis of 32 separate ready-for-sale herbal materials sent to LIAFT, an extreme level of variability was found in the products, with the concentrations of a common synthetic cannabinoid known as JWH-018 ranging from 0.8% to >30%.52 This result was linked with an unmonitored inaccurate procedure used when preparing these final products. This inaccuracy, leads to issues relating to dosage for example, it is common that websites and packaging do not contain information relating to safety, ingestion and recommended dosages (77% of 22 products purchased from five different websites selling NPS). Consequently, any dosage instructions would create inconsistent and unpredictable health effects in the user (51-53). This lack of dosage information is concerning, as a varying supply of substances can be purchased in a range of amounts from 1 gram to 1 kilogram of product.51
Furthermore, on analysis of 16 packages submitted to LIATF, it was also found that though numerous packets contained ingredients lists and several of these were consistent with the elements within the products, illicit substances where found within products that were not claimed on several labels. As a result, this produces a huge degree of risk relating to the users, as there is a possibility they are consuming products containing illicit substances unknowingly.52 For example, in a previously mentioned study conducted on 446 students to explore experience and the perception of risk association, 15.7% of respondents reported they did not know what drug they had taken and as a result, could not predict the effects of the substance, or report it to health professionals.42 Additionally, in a study conducted by Ayres et al.51 containing 22 analysed products, 23% were found to not contain the active ingredient that was claimed on the packet, and 9% of the products did not have a list of active ingredients at all.51 Moreover, the analysis of 24 products purchased from 18 UK-based websites claiming to be legal, discovered that 62.5% of these products contained controlled substances.53
Medical/Health care: It is an issue that NPS users are not attending drug treatment services, as a result of denial in branding themselves as drug users. Consequently, they are presenting themselves at non-specialist services such as accident and emergency departments, where the staff are commonly untrained, inexperienced and lack confidence in dealing with intoxication of this kind (Figure 14).54 The rarity of published, reliable literature and thorough analysis of substances means that practicing clinicians and other healthcare professionals have great difficulty in confidently identifying and diagnosing conditions associated with NPS.55 Consequently, these professionals are often ill equipped to care for these individuals, resulting in incorrect treatments and procedures not specific to their condition.53 Despite this limited understanding of NPS, individuals working in these emergency settings have had to develop their knowledge and skills relating to acute care management and protocols, so they are able to respond more proactively to the increasing number of patients with NPS-related symptoms.56
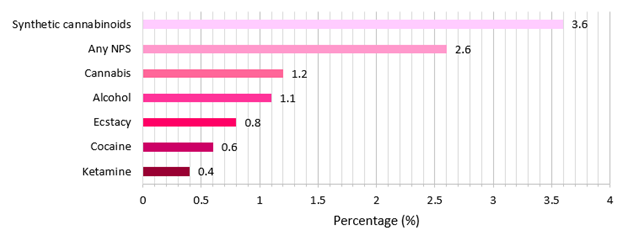
Figure 14 Percentage of users in 2016 who sought Emergency Medical Treatment following the use of substances. Modified from the Global Drug Survey 2016.39
It is emphasised by Public Health England, that it is important to have ‘an effective, highly trained and professionally skilled Public Health workforce’ and as a result, based on the increasing number of users who require medical treatment for NPS use, it is vital that health professionals are made more aware of these substances and their potential health risks.51 For example, Wood et al.29 found that healthcare professionals have reported less knowledge of NPS and therefore show less confidence in treating NPS toxicity when compared with traditional illicit drug effects. Furthermore, in a survey conducted by Campbell et al.57 on 196 members of medical staff in 2015, only 42% of the cohort reported good levels of confidence when dealing with NPS use. In the same study, respondents were asked what information sources they would commonly use if they required additional information on NPS to update their knowledge. It was found that colleagues were the majority (81%) of respondent’s information source followed by users, media, training and the Drug and Alcohol Monitoring and Information System (Table 4).57
|
How do you Receive Information on NPS Issues |
% of All Respondents who Reported ‘Yes’ |
|
Colleagues |
81% |
|
Users |
66% |
|
Media |
58% |
|
Training |
54% |
|
Drug and Alcohol Monitoring and Information System (DAMIS) |
54% |
Table 4 Information points on NPS recorded from 196 participants. Modified from Campbell, O'Neill & Higgin.57
In addition to the training of healthcare professionals, it is a reoccurring issue that there is no routine clinical laboratory tests which make it possible to detect NPS. Therefore, patients that are presenting themselves to emergency rooms who have taken NPS with no recollection of what they have consumed cannot be treated correctly.55
A way in which this shortage of knowledge is being combatted is by a project known as NEPTUNE. NEPTUNE is the UK network for NPS and has been established to enhance clinical practice when dealing with the effects of NPS through the use of clinical guidance documents. It is primarily aimed at settings within the forefront of medical care including, emergency departments, mental health services, drug treatment and recovery services and sexual health services.58 This project considers conceivable gaps in knowledge and has provided comprehensive guidance relating to the management of acute and chronic harms associated with club drugs and NPS use.57 Additionally, it is important that a lack of knowledge relating to drug interactions is addressed urgently so behaviours of drug training can be understood.57 It is of high importance that the range of services encountering these substances are connecting and sharing information based on NPS, to build and develop networks and supply users with the best possible treatment.54 For example, analysis by the EMCDDA found that health responses are being employed to intervention locations, including schools, nightlife venues and sexual health clinics where NPS users may seek advice and support.56
This literature review confirms the threat and disabling effects of the ongoing manufacture and supply of NPS. Whilst researching these synthetic substances, it has become clear that the information known has considerable limitations. Though the majority of factors surrounding NPS are commonly uncertain, it is certain that as the ever-increasing number of these analogues continues, they have the potential to evolve into compounds with increasing toxicity and risk. As discussed, many challenges are presented by the NPS phenomenon including; the vast diversity and large numbers of products, short-lived production relating to law evasion, wide availability, serious health risks/implications, and limited training of both medical and forensic professionals. As a result, it is becoming increasingly important that intensive research, copious reference standards and validated, universal methods of analysis are developed, that have the potential to match the rapid emergence of these products. This forensic data collected from these sources can then be forwarded to other professional bodies, to catalyse effective law enforcements and medical interventions, which aid in reducing this trade and providing effective treatment for victims.59
Conclusively, the developing trade of NPS, with the addition of high variability, unreliability of constituents and law evasion, makes the future of NPS hugely indefinite. Though the UK and many other international governments are attempting to introduce major controls against the production, supply and use of these substances, until they are able to advance ahead of the market, it is common their efforts will almost always be in vain. Ultimately, we are chasing the chemists and like most criminals, they have no intention on being caught.
None.
None.
None.

©2017 Hagan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.