Advances in
eISSN: 2378-3168


Review Article Volume 4 Issue 3
1Life Science Promoting Association, Japan
2University of Delaware, USA
Correspondence: Shaw Watanabe, Life Science Promoting Association, 25-3-1004, Daikyo-cho, Shinjuku, Tokyo 160-0015, Japan, Tel 81353797785, Fax 81353797786
Received: November 13, 2016 | Published: March 11, 2016
Citation: Hirakawa A, Melby MK, Watanabe S. Comprehensive food labelling for obesity control. Adv Obes Weight Manag Control. 2016;4(3):61-67. DOI: 10.15406/aowmc.2016.04.00088
Obesity rates continue to increase and be linked to many chronic diseases worldwide. Yet existing guidelines to help people achieve energy balance are difficult to implement. We propose a new energy unit (E-unit) of 80kcal such that healthy adults’ caloric need (in energy units) can be calculated by a simple equation where the necessary energy units = body weight (kg)x0.4 for daily intake throughout most of adult life including both sexes, the elderly and even pregnant women. This formula, in conjunction with the comprehensive food icon (FI), which is a colored guide for balanced nutrition used in Shokuiku (food and nutrition education) in Japan, will allow individuals to adjust their energy intake to achieve energy balance. The comprehensive food icon (FI) includes information about energy units, balance of major nutrients and antioxidant units (AOU) as a surrogate marker of vegetables and fruits. Widespread adoption and utilization of this food icon by food producers, suppliers and consumers will support people who want to control body weight.
Keywords: energy unit, food icon, obesity control, nutrient, dietary therapy
FI, food icon; AOU, antioxidant units; DLW, doubly labeled water; TEE, total energy expenditure; SCOP, saku control obesity program; PA, physical activity; BMI, body mass index; BMR, basic metabolic rate; EI, energy intake
Obesity rates continue to increase throughout the world.1,2 Rates of overweight and obesity among adults have increased for both men (from 29% to 37%) and women (from 30% to 38%) in recent years. Overweight and obesity are linked to more deaths worldwide than underweight. Health risks such as cardiovascular disease, cancer and diabetes increase when a person’s BMI exceeds 25.3–11 In 2010, obesity and overweight were estimated to have caused 3.4 million deaths, most of which were from cardiovascular events.1
In Japan, Healthy Japan 21 was implemented by the Ministry of Health, Labour and Welfare in 2000.12 Activities were implemented nationwide, including expectations that local governments formulate goals to enable individual residents to attain good health. However, mid-term review revealed that obesity rates have increased not decreased.13 Thus, we need to consider more effective tools to improve obesity control and prevention.
Obesity prevalence in Japan
Concerns over increasing obesity rates in Japan stem from results of the National Nutrition Survey, which have shown increasing trends in overweight in several demographic groups. Increases in overweight have been largest in men in small towns.14 This is in contrast to women living in larger metropolitan areas, where there has been a decrease in weight. Japan uses a stricter cut-off for obesity (BMI>25) compared to the US (where BMI >=30 is used), because incidence of obesity-associated chronic diseases increases in Japanese people with BMI >25. A range of causes have been proposed:
Population-level programs, education & guidelines
In response to increasing rates of obesity and associated chronic disease, Japan has implemented several policies, guidelines and programs. Kenkou Nippon 21 (Health Japan 21) began in 2000,18 followed by the Shokuiku (food and nutrition education) Basic Law which was passed in 2005.19,20 Subsequently, in 2008, the government launched a special health check-up (tokutei kenkou shinsa), involving measurement of waist circumference and nutrition counselling to reduce metabolic syndrome.13
Despite these programs and guidelines, obesity remains a public health problem in Japan. While nutrition and exercise scientists have documented required energy intake and expenditure, as described below, the form of the recommendations has not been ‘user-friendly’ enough to enable lay people to effectively implement the recommendations. Thus we propose a new Food Icon with associated energy unit that are easier to understand and use.
Recommended energy intake in DRI 2015 in Japan
Pooled analysis between health hazards and BMI showed that both total mortality and disease-specific mortality were lowest between BMI 21 and 25.5–8 The DRI2010 in Japan showed reported recommended energy intake in kcal/day for age categories and physical activity (PA) levels.20 In DRI2015 reporting changed to recommend energy intake levels to maintain advisable BMI: 18.5-24.9 from 18-49years, 20.0-24.9 from 50-69years of age and 22.5-27.4kg/m2 for people 70years and older.21
Body weight provides an individual with an easily- monitored indicator of the adequacy or inadequacy of habitual energy intake. Energy expenditure varies greatly among individuals as well as from day to day. In Japan, physical activity is divided into 3 categories and in the USA and Canada it is categorized into 4 levels: 1.0-1.39, 1.4-1.59, 1.6-1.89, 1.9-2.5.22 But Day-to-day variation in physical activity level varies up to 30% more than variation in dietary intake”.23
In children and pregnant or lactating women the energy requirement includes the energy needs associated with the development of tissues or the secretion of milk at rates consistent with good health.24–29
Accurate measurement of energy expenditure: Doubly Labeled Water (DLW) method
Studies in whole-body calorimeters have been considered the most reliable measurement of energy expenditure.30–32 With information on total energy expenditure (TEE) derived using the doubly labeled water (DLW) method, it has become possible to accurately determine the energy expenditure of not only adults but also infants and children under free-living conditions. The most compelling evidence about underreporting of food intake, which can range from 10 to 45 percent, has come from measurements of TEE by the DLW method.33–35 TEE is relatively unaffected by fluctuations in energy balance. These changes are small and attenuate the effect of energy imbalances only modestly.33 We employed the DLW method to estimate TEE in 315 of people ranging in age from 20 to 75 and the available DLW data offered the best currently available information.21 When TEE was divided by body weight, the quotients were rather stable being 0.4E-unit/kg body weight (Table 1). This quotient was similar in the EPIC cohort study (Table 2).
Sex |
N |
Occupation |
Age |
BMI |
BMR |
TEE |
PA |
Coefficient |
M |
10 |
Graduates |
24.2±1.8 |
22.1±1.1 |
1786±181 |
2910±524 |
1.6±0.3 |
0.45 |
M |
19 |
Healthy adults |
25.1±2.7 |
22.1±3.0 |
1530 |
2631±373 |
1.7±0.3 |
0.41 |
M |
18 |
Healthy adults |
33.8±3.3 |
23.6±3.7 |
1492 |
2655±526 |
1.8±0.2 |
0.41 |
M |
na |
Healthy adults |
43.8±2.5 |
24.4±2.6 |
1546 |
2581±311 |
1.7±0.2 |
0.40 |
M |
44 |
Healthy adults |
51±14 |
23.3±2.6 |
1447±184 |
2654±361 |
1.9±0.3 |
0.41 |
M |
19 |
Healthy adults |
53.3±2.5 |
24.3±2.4 |
1430 |
2445±311 |
1.7±0.1 |
0.38 |
M |
8 |
Elderly |
72.8±6.1 |
22.4±2.5 |
1505 |
2107±88 |
1.4±0.1 |
0.33 |
M |
19 |
Healthy elderly |
73.4±4.1 |
na |
1480±144 |
2539±586 |
1.7±0.3 |
0.40 |
M |
14 |
Elderly volunteer |
74±6 |
22.2±2.5 |
1133±179 |
1876±368 |
1.7±0.2 |
0.29 |
M |
17 |
Elderly at home |
82±3.1 |
24.8±3.8 |
1434±143 |
2294±311 |
1.6±0.2 |
0.36 |
F |
17 |
Healthy adults |
24.9±2.7 |
20.9±3.0 |
1254 |
1981±361 |
1.6±0.3 |
0.31 |
F |
22 |
Healthy adults |
33.7±2.8 |
21.6±3.0 |
1159 |
2039±394 |
1.8±0.3 |
0.32 |
F |
23 |
Healthy adults |
44±3 |
21.9±2.8 |
1147 |
2008±234 |
1.7±0.2 |
0.31 |
F |
12 |
Middle aged |
49.4±6 |
20.9±1.9 |
1188±121 |
1921±234 |
1.6±0.1 |
0.30 |
F |
16 |
Tennis player |
50±4.8 |
21.9±1.7 |
1240±92 |
2520±335 |
2.0±0.2 |
0.39 |
F |
15 |
Healthy adults |
52.7±2 |
22.7±1.5 |
1103 |
1953±220 |
1.8±0.2 |
0.31 |
F |
10 |
Healthy elderly |
73.3±3 |
na |
1221±91 |
2201±354 |
1.8±0.2 |
0.34 |
F |
10 |
Retired elderly |
74±4.4 |
24.1±2.8 |
1145±105 |
1814±213 |
1.6±0.2 |
0.28 |
MF |
12 |
Healthy elderly |
73 |
25±3.0 |
1371±201 |
2366±342 |
1.7±0.3 |
0.37 |
Table 1 Total energy expenditure and physical activity by age category measured by double labelled water method (National Institute of Health and Nutrition)
BMI: Body Mass Index; BMR: Basic Metabolic Rate, TEE: Total Energy Expenditure; PA: Physical Activity
Country |
n |
Weight |
EI_adj |
sd |
CV |
Coefficient for Unit |
|
Italy_Ragusa |
M |
168 |
78.5 |
2677 |
675 |
0.25 |
0.43 |
Itary_Florence |
M |
271 |
78.9 |
2656 |
677 |
0.25 |
0.42 |
Italy_Turin |
M |
677 |
77 |
2629 |
681 |
0.26 |
0.43 |
Italy_Varese |
M |
328 |
77.7 |
2764 |
678 |
0.25 |
0.44 |
Germany_Heidelberg |
M |
1033 |
83.6 |
2606 |
681 |
0.26 |
0.39 |
Germany_Potsdam |
M |
1235 |
82.6 |
2630 |
674 |
0.26 |
0.4 |
Netherlands_Bilthoven |
M |
1024 |
81.9 |
2640 |
694 |
0.26 |
0.4 |
UK_General poplation |
M |
404 |
80 |
2502 |
678 |
0.27 |
0.39 |
UK_Health conscious |
M |
114 |
77.9 |
2286 |
677 |
0.3 |
0.37 |
Denmark_Copenhagen |
M |
1356 |
83.1 |
2669 |
687 |
0.26 |
0.4 |
Denmark_Aarhus |
M |
567 |
82.8 |
2752 |
681 |
0.25 |
0.42 |
Italy_Ragusa |
F |
138 |
67.6 |
1980 |
519 |
0.26 |
0.38 |
Itary_Naples |
F |
403 |
67.5 |
2026 |
505 |
0.25 |
0.37 |
Itary_Florence |
F |
785 |
66 |
1965 |
486 |
0.25 |
0.38 |
Italy_Turin |
F |
392 |
63.6 |
1982 |
506 |
0.26 |
0.38 |
Italy_Varese |
F |
794 |
65 |
1939 |
481 |
0.25 |
0.38 |
France_Southcoast |
F |
612 |
60.4 |
1953 |
492 |
0.25 |
0.4 |
France_South |
F |
1396 |
60.2 |
2029 |
489 |
0.24 |
0.42 |
France_Northwest |
F |
622 |
60.8 |
2013 |
486 |
0.24 |
0.42 |
France_Northeast |
F |
2009 |
61.4 |
2040 |
486 |
0.24 |
0.41 |
Total |
0.4 |
Table 2 Adaptability of E-unit system to European population (EPIC Cohort Study)
EI: Energy Intake
The DLW-based evaluation of TEE provides the most accurate estimate of energy expenditure (Figure 1). The DLW data have been collected on a wide range of age groups and body sizes, so that estimated energy requirements can now be based on DLW measurements of TEE.33–39 Basal, resting and sleeping energy expenditures are related to body size and most closely correlated with the size of the fat-free mass. Energy expenditure is also affected by age, gender, nutritional state, inherited genetic polymorphisms and by endocrine differences. But the TEE values were usually within the range of individual daily deviation and can provide guidelines for recommended food intake.40
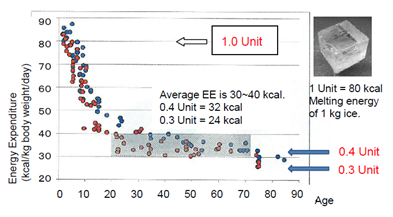
Energy expenditure (kcal/kg body weight/day) linearly decreases from birth to age 20 years, then it becomes stable throughout the life. 0.4 E-unit for this range and 0.3 E-unit for older age would be an appropriate factor for intake of energy source.
Balance between food intake and TEE
There is a need to re-evaluate the amount of energy released from macronutrients by in vivo oxidation. The values of 4, 9, 4kcal/g of carbohydrate, fat and protein, respectively, are still used widely in nutrition. The heat of combustion of carbohydrate and fat in a bomb calorimeter generally agrees with values from the Atwater system, but protein shows great variation.41–43 The energy derived by protein oxidation in a living body is less than the heat of combustion of protein, because the nitrogen-containing end product of metabolism is urea, which is excreted in the urine.44
Furthermore, as the thermal effect of protein is about 30%, the in vivo energy value of protein should be less than 2.8kcal/g. The use of 4kcal/g becomes a problem when energy intake is calculated in aging patients with sarcopenia or hypoalbuminemia.45 The difference between the estimated 4kcal/g and the more accurate 2.8kcal/g may result in energy insufficiency. Some intervention studies showing effects of a low carbohydrate and high protein diet may be explained by the difference of overestimated calorie intake.46
Humans can survive on diets providing widely varying proportions of carbohydrate, fat and protein.47,48 Large daily deviations from energy balance are readily tolerated and buffered primarily by energy stored in body fat.49
The coefficient of variation for intra-individual variability in daily energy intake is estimated to be +/- 23 percent.50 Variations in physical activity are not closely synchronized with adjustments in food intake.51 Thus, substantial positive as well as negative energy balances of several hundred kcal/d regularly occur under free-living conditions among normal and overweight subjects. For many macronutrients, there are few direct data on the requirements of children. Most recommendations are based on extrapolations from adult values.20,21
Dietary therapy for obesity control
Various dietary therapies for reducing body weight have been proposed, such as macrobiotics, Atkins diet, Zone diet, Ornish Diet, Learn Diet, etc.52 These diets can be classified as: total energy restriction with natural raw foods, low carbohydrate diet, high protein diet and balanced diet. The relative proportion of macronutrients varies among these diets. We propose a tailor-made nutritional guideline which is based upon individual energy consumption. Recent nutritional therapy does not calculate protein as an energy source, because if enough energy is obtained from carbohydrates and lipids, protein is not burned to yield heat energy.53 The necessity of carbohydrate and lipid metabolism needs further study, as shown in metabolic changes between fasting therapy and ketone diet.47,54 Accordingly, protein requirement is independently calculated by body weight x0.8 g, if there is no renal insufficiency.21
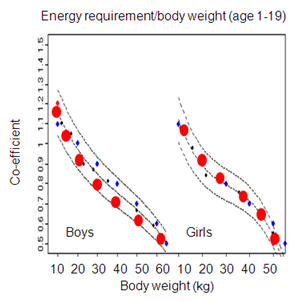
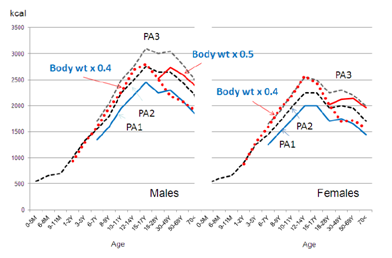
New energy unit to facilitate appropriate energy intake
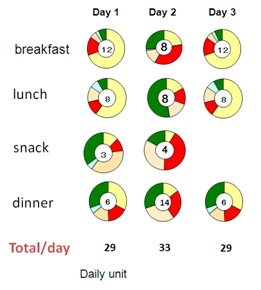
A new energy unit (E-unit), which is equivalent to the melting energy for 1kg ice block (80kcal), was proposed for the new nutritional plan based on energy intake.55 Healthy adults need [body weight (kg) x0.4] and active people need [body weightx0.5] energy units to maintain energy balance. For example, a 60kg man needs 24E-units, so 8E-units can be eaten at breakfast, lunch and dinner. In children and adolescents, higher multipliers are used, with the appropriate multiplier being 1.0 for up to 10kg body weight, 0.9 for up to 20kg, 0.8 for up to 30kg, 0.7 for up to 40kg, 0.6 for up to 50kg and 0.5 for up to 60kg (Figure 2A). The calculated values are in close agreement with those of the DRI2010. If the E-unit is shown on food labels and restaurant menus, it will facilitate the control of energy intake (Figure 2B). For example, if a person’s body weight is 75kg, necessary energy intake would be 30E-units (75x0.4), so the person may eat 10E-units each for breakfast, lunch and dinner. If people remember this simple rule, the average intake amount will approximate the recommended amount (30E-unit in the above example) (Figure 3).

Number of centre is E-unit. Weight of protein is described for low protein diet. AOU is a surrogate marker of vegetables and fruits (umole trolox equivalent/100 g). If there are balanced 4 colours, it suggests that the food contains sufficient vitamins and minerals
Comprehensive food icon (FI)
A three color guide for balanced nutrition, proposed by Toshiko Kondo, is used in Shoku-iku (food and nutrition education) at school.56 Yellow signifies food for energy, green signifies food for maintenance of the body and red signifies food for blood and muscle. Intake of specific foods such as 60g beans (mame), 5g sesame (goma), 40g eggs (tamago), 200g dairy (chichi), 10g seaweed (wakame), 120g vegetables and 150g fruits (yasai), 60g fish (sakana), 10g mushroom (shiitake) and 100g potatoes or yam (imo) are recommended by the mnemonic phrase “ma-go-ta-chi-wa-ya-sa-shi-i” which means “grandchildren are kind”.
Recommended intake amounts are derived from the National Health and Nutrition Survey and nutrients were calculated using the 5th Foods Contents Table.57 Adequate nutrient intake of amino acids, essential oils, vitamins and minerals can be obtained by following the above schema.21 The proposed Food Icon (FI) utilizes this 3-color schema.
In addition to the energy unit in the center of the food icon (FI), the relative proportion of carbohydrate, protein and fat is shown in the outer circle based on weight (Figure 3). As vegetables and fruits have different weights, we employed antioxidant units (AOU) as a surrogate marker. AOU aims to measure the free-radical-reducing capacity of all antioxidants in the diet and takes into account synergistic effects between substances.58–60 We defined the measured antioxidant capacity (μmol TE/day) in 242 foods and daily intake amount was calculated by 7-day weighed dietary records of 390 subjects over four seasons.61,62 TAC intake/day varied from 10,189 (summer) to 12,292 (winter). Vegetables (2827), fruits (2696) and beans (4151) were the three major sources. TAC can be used as a surrogate marker of vegetables and fruits intake.
For many nutrients, estimated requirements are based on balance, biochemical indicators and clinical deficiency data, because there is little information relating health status indicators to sufficiency or insufficiency of functional ingredients. If we obtain appropriate energy from diets based upon the FI system, the daily allowance of vitamins and minerals are usually achieved by consuming foods with 4 colours (magotachi-shoku). Although the units of AOU are different from those of the macronutrients, of the icon serves to convey the idea of balance, including micronutrients and functional food factors. Awareness of the balance of food colors facilitates healthy food choices.
Importance of self-awareness and individualized tailor-made nutrition counselling
Although control of total energy intake is essential to control obesity, individual awareness and practice are also important.63 We developed a weight loss program based on a behavioral approach with dietary and exercise intervention (Saku Control Obesity Program (SCOP)) in Japan.64–66 In this program, we emphasized individual-tailored counseling, instead of uniform instruction and the changes made in the diet and physical activity were designed for each participant. In the questionnaire, participants chose one of the five stages developed by Prochaska et al.,66 pre-contemplation (participants are not seriously considering changing behavior), contemplation (participants are considering changing behavior, but they have no intention of carrying this out within the next month), preparation (participants are considering changing behavior and they will carry this out within the next month), action (participants have already changed behavior months) within the last 6months) and maintenance (participants have already changed behavior for at least 6months.67,68 After one year intervention, 10% body weight reduction was achieved in more than half of the participants, for both males and females.68
Cooperation of food providers and industries
The food industry can play a significant role in promoting healthy diets by reducing the fat, sugar and salt content of processed foods.69,70 They can also provide useful and comprehensive information to consumers using the proposed FI (Figure 4). Food labels with detailed contents of nutrients are often too complicated and difficult to understand by ordinary consumers. Consumers primarily want to eat cheap and tasty foods and are generally not concerned with the exact nutrient content of foods. Ensuring that healthy and nutritious choices are available and affordable to all consumers will be easier if the FI becomes widely used. Fortunately, 80kcal=1 unit size has been long used by the Japanese Diabetes Society and the Food Exchange Tables are popular among patients.71 Practicing responsible marketing, especially those aimed at children and teenagers, will also help. Standardized labeling system would be useful for consumers, providers (such as restaurant menus and bento (lunch) boxes) and food industries (Figure 5).
Control of energy intake is essential to maintain healthy body weight. However, the units of kcal or MJ are not easily used or measured in daily life. Serving size or portion size is used in many food guidelines, but these do not provide quantitatively accurate bases for consumption. Use of a new energy unit (1E-Unit=80kcal) leads to a simple equation where the necessary energy units = body weight (kg)x0.4 for daily intake throughout most of adult life including both sexes, the elderly and even pregnant women. For growing children, the coefficient is modified from 1 to 0.4 for body weight ranges starting at 10kg and going up to 60kg. The comprehensive food icon (FI) includes information about energy units, balance of major nutrients and antioxidant units (AOU) as a surrogate marker of vegetables and fruits. Widespread adoption and utilization of this food icon by food producers, suppliers and consumers will support people who want to control body weight.
None.
The author declares no conflict of interest.

©2016 Hirakawa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.