Advances in
eISSN: 2377-4290


Research Article Volume 2 Issue 3
1Davis Eye Care Associates, USA
2North Suburban Vision Consultants, USA
3University of Missouri St Louis, USA
4Koffler Vision Group, USA
5Wohl Eye Center, USA
6Department of Ophthalmology and Visual Sciences, University of Michigan, USA
Correspondence: Robert L Davis, Davis Eye Care Associates, 4663 West 95th Street, Oak Lawn, Illinois 60453, USA, Tel 708-636-0600
Received: March 12, 2015 | Published: April 21, 2015
Citation: Davis RL, Eiden SB, Bennett ES, et al. Stabilizing myopia by accelerating reshaping technique (SMART)-study three year outcomes and overview. Adv Ophthalmol Vis Syst. 2015;2(3):92-98. DOI: 10.15406/aovs.2015.02.00046
Objectives: The SMART study is a three-year, longitudinal, multicenter evaluation comparing corneal reshaping contact lenses (CRCL) influence on the progression of myopia in children (age 8 to 14 at enrollment) to the wearing of soft silicone hydrogel contact lenses (SCL) worn on a daily wear basis with monthly replacement. This study represents one of the largest patient enrollment with ten investigators and adds to the literature by verifying the outcomes of smaller enrolled investigations strengthen the outcomes of corneal reshaping techniques.
Methods: At enrollment 172 subjects were fit with corneal reshaping contact lenses worn overnight on a nightly basis (Emerald design by Euclid Systems) and 110 subjects were fit with silicone hydrogel contact lenses on a daily wear monthly-replacement basis (Pure Vision by Bausch & Lomb). Visits were conducted at 24 hours, one week, one month, three months, and every six months thereafter for three years. A regression protocol was conducted for the CRCL subjects at each yearly visit for three years by discontinuing lens wear and monitoring for stability of refraction and topography for consecutive visits until baseline was reached.
Results: The outcome of the three-year investigation indicated that myopia progressed at a statistically significantly higher degree in the SCL group as compared to the CRCL group. Mean spherical equivalent change in myopia for the SCL group was -1.03±0.58 diopters, vs. CRCL group -0.13±0.62 diopters s (p<0.0001). There were no cases of reduced best corrected visual acuity for three years for either group. There were no significant adverse events in either group from baseline to the three-years. 80% of eyes were successfully fit with CRCL with the first lens fit empirically and 95% of eyes were fit successfully with only one lens change. There was no significant difference between dropout rates during the three year study between the two groups.
Conclusion: The three year longitudinal study found that myopia progressed at a significantly higher degree in the SCL vs. CRCL subjects. . Efficacy, safety, and dropout rate of corneal reshaping in our sample population appears to be comparable to wearing SCL.
Keywords: corneal reshaping, myopia progression, axial length, vitreous chamber depth
SMART, study three year outcomes and overview; CRCL, corneal reshaping contact lenses; SCL, silicone hydrogel contact lenses; SV, single vision; GP, gas permeable; AL, axial length; VCD, vitreous chamber depth; CRAYON, corneal reshaping and yearly observation of nearsightedness; SV, vision spectacles; VA, visual acuity
Myopia remains one of the most prevalent and significant ocular disorders for which a search for a suitable treatment method has not been equivalently acknowledged clinically. In the United States it affects approximately one-third of individuals over the age of 121 with a much higher percentage of people impacted in parts of Asia.2 It has been estimated that slowing the progression of myopia could impact 40 million patients in the United States as a result of the incidence of fewer ocular health risks with low (rather than high) myopic refractive error.3-8 As myopia progression is thought to be primarily due to elongation of the axial length (AL) of the eye, predominantly associated with the elongation of the vitreous chamber depth (VCD), controlling the progressive elongation is key to myopia progression control.9-12 It has been found that over a three year period, single vision soft lenses did not have any significant effect on slowing axial length progression in young contact lens wearers versus spectacle wearers.13 However a concentric bifocal dual-focus soft contact lens design has been shown to significantly reduce myopic progression in children in comparison to a soft single-vision soft lens.14 The concentric distance centered soft lens bifocal created a simultaneous myopic retinal defocus. This effect was further investigated by Sankaridurg et al.15 the study used a soft contact lens designed to reduce relative peripheral hyperopic defocus and demonstrated a significant (34%) reduction in myopia progression over a 1-year period in children in comparison to results with spherocylindrical spectacle lenses. Lam et al.16 conducted a 2-year double-blind randomized controlled trial using a DISC bifocal lens which provided an addition of +2.50 D.16 The purpose of the investigation was to determine if defocus in soft bifocal lens wear slows the progression of myopia in children. Myopia progressed 25% more slowly for children in the DISC group compared with those in the control single vision (SV) group (0.30 D/year; 95% CI -0.71 to -0.47 vs 0.4 D/year; 95% CI -0.93 to -0.65, p=0.031). Further analysis demonstrated that there was less axial elongation for children in the DISC versus SV groups (0.13 mm/year; 95% CI 0.20 to 0.31 vs 0.18 mm/year; 95% CI 0.30 to 0.43, p=0.009). This study supported that simultaneous vision with constant myopia defocus can retard progression of myopia.
Limiting the progression of myopia may serve to limit secondary pathological effects such as macular degeneration, cataract, glaucoma, retinal holes and tears, and retinal detachments.17-20 Early researchers found that progressive addition spectacle lenses21 and both PMMA22 and conventional rigid gas permeable contact lenses23,24 did result in the positive effects on the progression of myopia. However subsequently conventional gas permeable contact lenses when compared to spectacle lenses25 and soft contact lenses26 were found to offer no additional advantage in stabilizing myopia. Corneal flatting effects were attributed to the apparent myopia stabilization effects of GP lenses when compared to soft lenses during the first year of the study. No significant difference in axial length progression was noted between the two groups. Corneal reshaping treatment has exhibited great potential for myopia stabilization. Corneal reshaping (i.e., orthokeratology, corneal refractive therapy, vision shaping treatment) is a process which utilizes reverse curve technology rigid contact lenses to temporarily reshape the corneal contour and reduce the eccentricity of the cornea. Corneal reshaping reduces the myopic refractive error by applying rigid gas permeable (GP) lenses which have a central curvature that is flatter than that of the cornea.27 This concept to modify the corneal shape and power by flattening the central cornea while creating mid- peripheral steeping by the action of the reverse contact lens curve creates the induced peripheral myopic defocus that neutralizes the peripheral hyperopic defocus found in progressive myopes. The peripheral defocus has been studied by using both the optics of spectacle and contact lens.28-31 Recently studies on the mechanisms that regulate refractive progression suggest that optical treatment strategies directed at the retinal periphery might be more effective in controlling eye growth and myopia. These studies have concluded that optical interventions not only correct central refractive error to obtain clear vision but also correct peripheral hyperopia to slow the progress of myopia.32
Most of the research on corneal reshaping has centered on patients before they reach 8th grade because of the patient availability before they are college bound. There is particular interest in the correction of myopia in this population soon after its diagnosis. About 15 % of children become myopic between the ages of 6 to 14 years of age33 with vision correction often necessary between 8–10 years of age.34-38 The progression of myopia will typically continue into the teenage years until approximately age 15 for girls and 16 for boys.39 Several studies have focused exclusively on young people and have concluded that corneal reshaping has great promise as an effective method of controlling myopia progression.3,40-44 Changes in axial length (AL) and vitreous chamber depth (VCD) appear to be the important anatomic factor to control myopia progression Cho et al.45 monitored AL and VCD over a two year period with 35 children aged 7-12; this group was compared to a spectacle-wearing control group from a previous study. They found an approximate 46% reduction in both AL (0.29mm for corneal reshaping versus 0.54mm for control group) and VCD (0.23mm for the corneal reshaping group versus 0.48 for the control group). These results were confirmed by Walline46 from the first year results of the Corneal Reshaping and Yearly Observation of Nearsightedness (CRAYON) study. It was found by wearing either daily wear conventional GP lenses or soft lenses resulted in a 38% increase of AL of 0.35mm whereas corneal reshaping in comparison resulted in growth of only 0.15mm. Kakita et al.47 examined the influence of overnight corneal reshaping on axial elongation VS spectacle lens wearers as a control group. After 2 years the axial length increased 0.39±0.27 mm for the corneal reshaping group and 0.61±0.24 mm for the spectacle group.47 These findings demonstrated that corneal reshaping slows axial elongation in myopic children by approximately 36%, and thereby slows the progression of myopia as compared to spectacle lens correction which increased significantly (.05). Santodomingo-Rubido et al.48 compared axial length growth in white myopic children wearing corneal reshaping contact lenses (CRCL) and distance single vision spectacles (SV) for a 2-year period. They reported that the axial length increased significantly over time for both the CRCL group (0.47mm) and SV group (0.69mm); P<0.001). Measurements of axial length in the above two studies were taken with the Zeiss IOL Master (Carl Zeiss Jena GmbH, Jena, Germany). The refractive spherical components for the corneal reshaping group increased –0.34+/- 0.29 whereas the increase in myopia for the SV group was -1.25.+/-1.38.
Hiraoka et al.49 compared axial length changes in myopic children receiving either overnight corneal reshaping or spectacles as controls.49 The increase in axial length during the 5-year study period was 0.99 mm±0.47 for the corneal reshaping group and 1.41±0.68mm for the control groups. The difference was statistically significant for the first 3 years, but not for the fourth and fifth year. These findings are similar to the COMET bifocal study in which the treatment effect seems to diminish after 3 years. Kwok-Hei Mok and Sin-Ting Chung50 measured refractive error and central corneal curvature for 34 children wearing corneal reshaping lenses and for 36 children who wore spectacles 6 years or a longer.50 All the CRCL patients had a washout period that was determined to occur when the keratometry findings at the end of the study matched the findings prior to beginning the study. Myopic progression was calculated as a change of myopia from the baseline to the final visit. Average myopic progression of the overnight CRCL group was 0.37±0.49 D (0.05 D/year) while average myopic progression of the single-vision spectacle group was 2.06±0.81 D (0.29 D/ year) after 7 years. The previous studies resulted in the development of the Stabilizing Myopia by Accelerating Reshaping Technique (SMART) study. The intent of the SMART investigation is to determine if wearing corneal reshaping lenses (CRCL) on an overnight basis slows the progression of myopia in children (AGE8-14).
The objective of this multisite investigational protocol is to investigate the myopia stabilization effects of wearing reverse geometry lenses and compare it to subjects (wearing daily wear soft contact lenses (SCL) as measured by change in refraction following regression to stable refractive and topographic state. To determine the final refractive error of the corneal reshaping group a washout period was conducted at the end of each year.51 Subjects were refracted after not wearing the lenses for a period of time until the flat corneal curvature reverted to its baseline value.
Study enrolment and locations
This study was conducted in accordance with the guidelines provided by the Declaration of Helsinki, approved by an Institutional Review Board and in adherence to the guidelines of the respective universities conducting this study. All subjects and parents were given an option of selecting the CRCL or SCL group after signing an informed consent as a strategy to avoid significant drop out rate. The study was conducted at ten investigational sites in the United States and included 172 test subjects (82 males, 90 females) who were fit with Emerald design corneal reshaping lenses fabricated in the Boston Equalens II gas permeable contact lens polymer (Euclid Systems Corporation, Herndon, Virginia). 110 subjects (42 males, 68 females), were fit with the Pure Vision (Bausch & Lomb, Rochester, New York) contact lens, and served as controls. The test group had a mean age of 11.1 years (range is 8-14); the control group had a mean age of 11.7 years (range=8-13). The control group included the same inclusion/exclusion criteria as the experimental group with the exception of the wearing of soft contact lenses.
Subject selection (inclusion/exclusion criteria)
The investigators selected potential candidates without any requirements as to gender, or racial/ethnic and religious backgrounds. Subjects currently undergoing corneal reshaping or subjects previously successful or unsuccessful in daily or overnight corneal reshaping were not eligible for the study. Baseline findings, including inclusion and exclusion criteria, for subjects have been described previously. Subjects were not randomly assigned to a contact lens group, but rather those who did not want CRCL lenses wore SCL lenses through the study to avoid high drop out.
Initial contact lens fitting
The fitting of test subjects with overnight corneal reshaping contact lenses was performed entirely with an empirical technique. Data provided to Euclid Systems included manifest refraction, keratometric values and horizontal corneal diameter measurements. Euclid Systems then applied their proprietary fitting nomogram to these data to determine the parameters of the initial corneal reshaping contact lenses for each test subject. The fitting of the control subjects with Pure Vision soft contact lenses was conducted by diagnostic contact lens evaluation. Application of diagnostic contact lenses allowed the investigators to determine appropriate physical fit and power of the Pure Vision lenses for the control subjects.
Examination procedures
Subjects were examined for eligibility at the baseline examination. Subjects had data collected at the initial visit and likewise at all follow-up visits. At the dispensing visit all subjects picked up their contact lenses and were instructed on how to apply, remove, and care for the study lenses. The day after the first night of contact lens wear the treatment subjects were examined within one hour of waking. Each test patient was instructed to wear their lenses a minimum of six hours each night so the reverse geometry lens design could take its effect. At one week, two weeks, one month, three months, six months, and one year the test subjects were evaluated, at minimum of eight hours after lens removal. The timetable of patient visits was initiated after the investigator acknowledged that the lens specifications were appropriate and appropriately managed the subject’s refractive error.
Each examination consisted of the following procedures
Visual acuity (VA) Bailey-Lovie low and high contrast acuity (total letter count and test distance recorded), corneal topography, refraction (manifest at each visit and cycloplegic annually), slit lamp examination, dilated fundus examination (initial visit and exit visit only), pachymetry (semi-annually) (A-Scan 2000 by Ophthalmic Technologies), intraocular pressure (twice a year), keratometry (Bausch and Lomb), and contact lens comfort, handling and wearing time questionnaire. Due to the number of investigational sites involved in the study the topographers and slit lamps make and model varied. For subjects in the test group only, once a year corneal reshaping contact lens wear was discontinued and a regression procedure was instituted in order to re-establish baseline refractive error and corneal shape values. At these yearly intervals, each test group subject had their treatment lenses returned to the investigator and replaced with soft lenses. Refraction, topography, and keratometric readings were monitored every three days following discontinuation of treatment lens wear until two consecutive visits exhibited stabilized readings. Stable refraction was defined as two consecutive findings of both cycloplegic and manifest refraction within +/-0.25D. Stable keratometry and topography were defined also as two consecutive findings of keratometry and simulated keratometry within 0.25D. After the data was collected, a new treatment lens with the same specifications as the lens that was returned to the investigator was dispensed and treatment was resumed. This procedure continued each year of enrollment in the three year study. Similarly, at yearly visits the control group was monitored by the same diagnostic test sequence as the initial baseline visit. The readings were compared to baseline to demonstrate the net effect of the control group. If uncorrected vision was reduced during the initial treatment period with the treatment corneal reshaping group, disposable soft contact lenses were provided or the investigational corneal reshaping lens was worn during daytime hours until adequate vision was achieved. This was necessary with some patients during the initial two to three weeks of the study while the treatment effect was occurring.
The Boston Conditioning Solution and The Boston Cleaner (Bausch & Lomb) were provided to all treatment group subjects in this study. If subjects showed clinical signs or symptoms of solution allergies, an alternate solution regimen such as Optimum CDS Cleaning, Disinfecting and Storage Solution and the Optimum CDS Extra Strength Cleaner (Lobob) was dispensed. Renu multipurpose disinfecting solution was supplied to the control group subjects in the study. If a subject showed clinical signs of solution allergies an alternate solution regimen such as Opti-free was dispensed.
Statistical analysis
Descriptive statistics were used to provide means and standard deviations. T-tests were used to assess statistical significance between the measurements at baseline and at the end of year three. Significance was determined at the level Ө=0.05. For the statistical analysis of the refractive data, it was converted from sphere, cylinder and axis into the Deal and Toop co-ordinate system: where X=-(Cyl/2)cos2Ө (Ө is the axis of astigmatism); Y=-(Cyl/2)sin2Ө (Ө is the axis of astigmatism) and Z= Sphere+Cyl/2, i.e. the nearest equivalent sphere or best sphere. Analysis was performed using Graph pad Prism (Graph pad Software Inc., La Jolla, CA).
Corneal reshaping fitting outcomes
The SMART study demonstrated that fitting corneal reshaping contact lenses utilizing a purely empirical technique can be highly successful. Initial success outcomes based on the empirical fitting method resulted in 80.5% of eyes successfully fit with the first lens ordered, 95.5% successfully fit with up to one lens change, and 99.5% successfully fit with up to two lens changes. Success was defined as the ability to wear the corneal reshaping lenses on an overnight wear basis and achieving 20/25 or better uncorrected visual acuity. Experience with fitting of the test corneal reshaping contact lenses did not seem to be important since eight of the ten investigators had no prior experience in fitting Euclid corneal reshaping lenses prior to their involvement in the SMART study.
Dropout rate
The dropout rate for the first year of the study was similar between the two groups with 34/172 (19.8%) discontinuing lens wear in the corneal reshaping test group and 20/110 (18.2%) discontinuing lens wear in the soft lens wearing control group; however, the time period from study onset to discontinuation differed significantly between the two groups. For the corneal reshaping group, the mean time to discontinuation was 27.8 days (range 1 day to 28 weeks, 57% 1 week or less). The most common reason given for discontinuation was poor comfort with lens wear (55% of discontinued subjects). For the soft lens group the mean time to discontinuation was 103.8 days (range 1 day to 55 weeks, with 57% being greater than 1 month). The most common reason for discontinuation in this group was lost interest in lens wear or lost to follow up (85%). The group dropout rate in year two for the control group was 7.8% and for the test group was 7.2%. The dropout rate in year three for the control group was 12.0% and for the test group was 9.3%. At the conclusion of the third year the total dropout rate from baseline for the control group was 33.6% whereas the dropout rate for the test group from baseline was 32.5%. There was no significant difference between the groups with regard to dropout rate.
Myopia progression
The effect of the corneal reshaping treatment is evident by the reduction in myopic refractive error to near plano while wearing the corneal reshaping lenses and remained the same after one year immediately prior to the regression period whereas the soft lens wearing control group increased in myopic spherical equivalent refractive error by mean of -0.38 diopters at the one year period. Following the brief discontinuation of treatment at one year for the corneal reshaping treatment group, myopia returned approximately to the baseline level (mean change in spherical equivalent -0.02 diopters from pre-treatment level) with an associated best corrected visual acuity measurement of 20/20 (Figure 1) depicts the mean spherical equivalent refraction at baseline and one year. The control group increased significantly in myopia from baseline to one year (from-2.32±1.03 D to -2.69±1.06 D), and the mean spherical equivalent change in myopia was -0.38±0.80 diopters. The test group data were obtained following successful regression as defined by the study protocol. Prior to the one year regression acuities and refraction were obtained and monitored throughout the regression period. Following regression the test group had a mean spherical equivalent change in myopia of -0.02±0.53 diopters (from-2.56±1.19 D to 2.59±1.21 D).
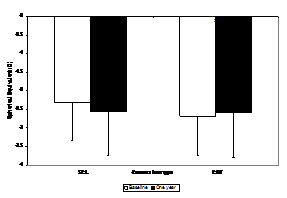
Figure 1 Mean spherical equivalent (D) with standard deviation for the soft contact lens and corneal reshaping group at the baseline and one-year visit.
At the second year the change from baseline in spherical equivalent for the control group was significantly more myopic than for the test group (p <0.0001) after the regression period. The change from baseline at the second year for the test group was -0.09D±0.60 D and for the control group was -0.83D±0.58 D (Figure 2). At the 3-year the spherical equivalent change from baseline for the test group was -0.12D±0.64 D and the spherical equivalent change from baseline for the control group was -1.01D±0.67 D. The control group increased in myopia from baseline from -2.32±1.03 D to -3.33±1.16 and the test group increased in myopia from baseline from -2.56±1.19 D to 2.68±1.11 D which was statistically significant (p<0.0001) (Figure 3). The difference in myopia progression between the test and control groups was statistically significant at the p<0.001 level of confidence after the regression period (Figure 4). Mean change in manifest spherical equivalent over three years based upon baseline myopia and treatment group. Low myopia was defined as less than -1.50, moderate myopia -1.50 to 3.00 and high myopia -3.00 and above (Figure 5). Mean change in manifest cylinder over three years based upon baseline myopia and treatment group. Low astigmatism was defined as -1.00 and below.

Figure 2 Mean spherical equivalent (D) with standard deviation for the soft contact lens and corneal reshaping lens group at the baseline and two-year visit.

Figure 3 Mean spherical equivalent (D) with standard deviation for the soft contact lens and corneal reshaping lens group at the baseline and three-year visit.

Figure 4 Mean change in manifest spherical equivalent over three years based upon baseline myopia and treatment group.

Figure 5 Mean change in manifest cylinder over three years based upon baseline myopia and treatment group.
Axial length measurements did not corroborate with the changes in refractive error between the two groups. There was no statistically significant change in either axial length or in vitreous chamber depth measurements between the test and control groups (p>0.05), however there was high variability in these measures that likely were attributable to measurement errors between the various investigational sites. There was no statistically significant change in the astigmatism values for either group from baseline to the one year analysis (p>0.05). In addition, significant central corneal flattening of approximately 1.5D occurred in the CRCL group with less than 0.25D change in the SCL group. There were no statistically significant or clinically significant reductions in best corrected spectacle acuity levels for either the corneal reshaping or soft lens groups (p≤0.0001) (Table 1).
% of Eyes Achieving Uncorrected VA Levels |
|||
Yr 1 |
Yr 2 |
Yr 3 |
|
20/15 or better |
12% |
10% |
12% |
20/20 or better |
61% |
70% |
71% |
20/25 or better |
71% |
82% |
88% |
20/30 or better |
81% |
90% |
96% |
20/40 or better |
83% |
95% |
99% |
< 20/40 |
17% |
5% |
1% |
Table 1 Efficacy of corneal reshaping on visual acuity
The SMART study was conducted at ten investigator sites and enrolled 110 control (soft contact lens daily wear) and 172 test (overnight wear corneal reshaping treatment) subjects. These subjects were monitored over a three year time period. The primary outcome of the SMART study evaluated was the difference in myopic progression between the test and control subjects. The secondary outcomes evaluated included the efficacy of empirical fitting for corneal reshaping treatment, differences in dropout rates between the test and control groups and safety as indicated by best corrected visual acuity at the start of the study vs. the termination of the study. There was a significant difference in the progression of myopia between the test group and the control group during each of the three years of the SMART study. At the conclusion of the study the corneal reshaping test group increased from baseline in myopic spherical equivalent by a mean of -0.12D±0.64 D while the soft lens wearing control group increased from baseline in myopic spherical equivalent by a mean of -1.01D±0.67 D. The objective correlate to myopic refractive error progression is axial elongation and increased vitreous chamber depth. The outcomes of the SMART study failed to show any statistically significant changes in either of these measures between the test and control groups when compared at the end of each of the three years of the study. There was, however great variability in these measures between investigational sites. As such, we felt that this data outcome may not be valid and should not put in question the results of other studies of corneal reshaping where definitively greater axial elongation and increased vitreous chamber depth measures were found in control groups vs. test groups. In those studies there typically were not the numbers of investigational sites as was the case in the SMART study.
The efficacy of empirical fitting for corneal reshaping utilizing the Emerald lens design (Euclid Systems Corporation, Herndon, Virginia) was confirmed in the SMART study. 80.5% of subjects were successfully fit with the initial empirically fit lens, an additional 15% were successful with only one lens change, 4% more with a second lens change and the remaining 0.5% with a third lens change. Our results of high first lens fitting success are in agreement with the outcomes of Chan41 who reported a first lens fitting success of 73.5% and second lens success of 90.0%. Experience in fitting of the corneal reshaping lens design did not seem to have any influence on the success of empirical fitting based on the fact that eight of the ten investigators had no clinical experience in fitting the Emerald lens design prior to participating in the SMART study. Dropout rates during the three years of the SMART study were very similar between the test and control groups. The initial year of the study showed a dropout rate of 19.8% for the control group and 18.2% for the test group. This is very similar to results of Cho.45 however that study was conducted on a much smaller group of test subjects (35 vs. 172). Although the dropout rates were very similar, the time periods to drop out and reasons for dropout were quite different. The control group tended to drop out over a more prolonged period of time (57% over one month, with a mean of approximately 3.5 months) and the main reason for dropout was loss of interest in contact lens wear or loss to follow up. For the test group the dropout tended to occur earlier (57% less than two weeks, with a mean of approximately one month) and the most common reason given for dropout was discomfort with corneal reshaping lens wear. Cumulatively after the three years of the SMART study the dropout rate was 33.6% for the control group and 32.5% for the test group. This indicates that success as defined by continued wearing of lenses is similar between corneal reshaping and the wearing of daily wear use soft contact lenses. Clinically practitioners can utilize this information to better manage their patient’s expectations during the adaptation period. The most concerning complication of contact lens wear is the loss of best corrected visual acuity due to some complication of lens wear. In the SMART study after three years there was no loss statistically significant loss of best corrected visual acuity in either the test or the control group. This is a critically important safety measure of both vision correction modalities, especially when considering that we are implementing treatment for children.
The SMART study outcomes can be added to those of numerous other investigations supporting the efficacy of overnight corneal reshaping treatment to reduce the rate of myopia progression when compared to other vision correction modalities. In addition SMART outcomes illustrate the ease and success of fitting corneal reshaping lenses empirically both by novice and experienced contact lens practitioners. Finally, the SMART study suggests that overnight corneal reshaping treatment is a safe and effective method of vision correction for myopic children.
The authors would like to acknowledge Bausch & Lomb (Rochester, New York) for providing an unrestricted research grant for the study as well as providing the soft contact lenses and solutions for the study and Euclid Systems Corporation (Herndon, VA) for providing lenses used in this study. We also would like to acknowledge Natalie Cogswell, the SMART Study Coordinator and Lisa A. Jones-Jordan, PhD for statistical assistance. Lastly data are being provided by the SMART study group Ed Bennett, OD, FAAO, Cary Herzberg, OD, FAAO, Michael Lipson OD, FAAO, LaMar Zigler, OD, FAAO, Doug Becherer, OD, FAAO, Bruce Koffler, MD, Rob Gerowitz, OD, FAAO, Lisa Wohl, MD, S Barry Eiden OD, FAAO and Robert L Davis OD, FAAO.
Author declares that there is no conflict of interest.

©2015 Davis, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.