Advances in
eISSN: 2377-4290


Research Article Volume 7 Issue 3
1Captain James A Lovell Federal Health Care Center, USA
2Chicago Medical School, Rosalind Franklin University of Medicine and Science (RFUMS), USA
3Scripps Health/Scripps Memorial Hospital/Scripps Mericos Eye Institute, USA
4Applied Vision Research Centre, University of London, UK
5ZeaVision LLC, 680-F Crown Industrial Court Chesterfield, USA
Correspondence: Stuart P Richer, Captain James A Lovell Federal Health Care Facility, 3001 Green Bay Rd, North Chicago, Illinois, 60064 USA
Received: July 14, 2017 | Published: July 28, 2017
Citation: Richer SP, Cebold B, Katkar M, Huntjens B, Pratt SG, et al. (2017) Restoration of Central Macular Pigment Dip with Dietary RR Zeaxanthin Supplementation in Patients with AMD. Adv Ophthalmol Vis Syst 7(3): 00219. DOI: 10.15406/aovs.2017.07.00219
Objective: Low macular pigment optical density (MPOD) is a major risk factor for age-related macular degeneration (AMD). This paper investigates the impact of 8 mg dietary RR zeaxanthin (Z) supplementation on MPOD distribution and the associated effect on macular scotomas in patients with a central foveal dip in their macular pigment spatial profile.
Methods: This is a retrospective review of The Zeaxanthin and Visual Function RCT (FDA IND 78, 973) with respect to the relation between low levels of MPOD and increased risk of age-related macular degeneration (AMD). We retrospectively examine the effect of daily supplementation of 8 mg of dietary Z on n=4 patients having a baseline central foveal dip in their MPOD distribution. The testing modalities used were a 7⁰ 3D specular reflectance and the associated kinetic 20° macular visual fields.
Results: Over a 12-month period, all four patients showed a progressive increase in central peak restoration with related kinetic and/or Amsler grid visual field data.
Conclusion: The initial results demonstrate marked improvement in macular pigment architecture and overall visual function after 12 months of Z supplementation. These results warrant a prospective clinical trial with a larger number of subjects to investigate the role of Z in central dip amelioration.
Keywords: zeaxanthin, meso-zeaxanthin, amd, central foveal dip, scotomas, macular pigment optical density
L, lutein; Z, rr zeaxanthin; Mz, meso-zeaxanthin (rs zeaxanthin); AMD, age-related macular degeneration; MPOD, macular pigment optical density
The central macula lutea (fovea) contains the highest density of cone photoreceptors, responsible for detailed and color vision in the central 2-3° of the visual field. AMD is the leading cause of permanent vision impairment in aging Western populations, with the Centers for Disease Control and Prevention estimating that 1.8 million Americans over age 40 have AMD and another 7.3 million Americans have large drusen, which places them at a high risk of developing AMD.1 Research demonstrates that the relationship between MPOD and central retinal thickness has a strong positive correlation,2 and additional studies show that reduced MPOD is associated with a higher risk of developing AMD.3 Heterochromatic flicker photometry has been used to measure the spatial profile of MPOD, with two predominant profile types emerging: typical exponential/peaked profile or atypical “central dip” profile.4 The MARS study by Dietzel et al.,5 found 19.8% of subjects possess this central dip profile, meaning they demonstrate a significantly lower MPOD at retinal eccentricities of 0°, 0.25°, and 0.5° but significantly higher MPOD at 1° and 2° when compared to subjects with no central dip. Concordance between pairs of eyes was labeled as highly significant.5
The underlying cause of this central dip profile is not well understood, though research showing a higher incidence in certain ethnic populations suggests a genetic link.6,7 The three primary risk factors for MPOD central dip have been identified as the same three primary risk factors for AMD: age, smoking, and elevated BMI.4,8 Macular pigment is composed of three carotenoids: lutein (L), RR zeaxanthin (Z), and RS meso-zeaxanthin (Mz). These three molecules are collectively known as xanthophyll carotenoids or macular carotenoids. L and Z have both been well-studied and are found in many vegetables regularly consumed by humans such as spinach, broccoli, kale, and bell peppers.9 The role of Mz is not as well understood: it has recently been found in the human food chain in the skin of a handful of species of fish, but only in trace quantities. Research has shown that Mz can be enzymatically derived from L,10 though the relative roles of endogenous Mz isomerization versus dietary consumption of Mz in retinal health remain unstudied (Figure 1-3).
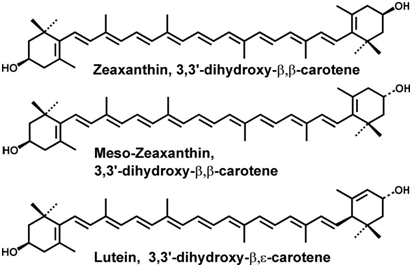
Figure 1 Molecular structures of the three macular carotenoids: Zeaxanthin, Meso-zeaxanthin, and Lutein.
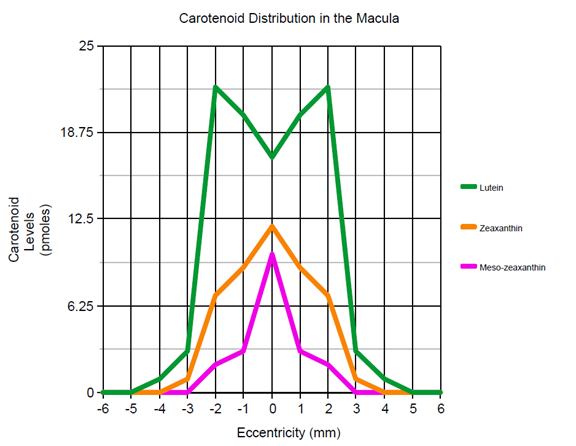
Figure 3 Distribution of macular carotenoids as a function of retinal eccentricity.40
Studies have shown that macular carotenoid supplementation provides myriad visual health benefits, including improved visual acuity, glare recovery, and contrast sensitivity function 11, along with increasing both neural processing speed and efficiency of visual signals.12 Furthermore, macular carotenoid supplementation has been linked to improved cognitive function13 and reduced cortisol levels.14 The ratios of L, Z, and Mz vary throughout the macula, though total MPOD peaks in the central fovea/foveola. Dietary Z prevents oxidative stress by absorbing harmful blue light (400-500nm),15 which reduces retinal inflammation and neovascularization within the photoreceptive/RPE layers. Z supplementation has been shown to increase MPOD and improve visual function,16,17 yet there has been no research on the impact of macular carotenoid supplementation on the volumetric profile of macular pigment, particularly the central foveal dip. This article aims to investigate the effect of Z supplementation over a 12-month period on patients with central foveal dip by measuring serial MPOD and corresponding 20° central macular visual field scotoma resolution.
The data represents individual subjects within the ZVF study (Zeaxanthin and Visual Function), a 1-year prospective, double-bind RCT at the DVA North Chicago Medical Center.17 Recruitment was staggered and began on November 26, 2007. The final subject completed his 12-month evaluation on May 19, 2009. The ZVF Study received approval from the DVA Office of Research and Development and Human Subjects Protection (ZVF-FDA IND #78, 973) and was registered with www.clinicaltrials.gov. The study included 60 subjects with early and moderate AMD assigned randomly into 3 groups, each receiving supplementation consisting of: 8mg of Z (n=25), a combination of 8-mg Z plus 9 mg L(n=25), or a “faux placebo” 9-mg L supplement (n=10). Subjects were excluded from the study if they either manifested or displayed high-risk retinal characteristics of advanced AMD, for which medical or surgical options for treatment were available. The Automated Retinal Imaging System® (ARIS, Prescott, AZ, USA) used a specular reflectance technique to acquire the spatial distribution of macular pigment. A 7°, 3-dimensional image of 3D macular pigment distribution was obtained through ARIS using an auto fluorescence technique.17 The macular visual fields were evaluated using the SimulEyes® Kinetic Visual Field (Gold Beach, OR, USA). The testing software evaluated monocular central field vision with best refractive correction at each visit. This visual field instrument incorporates an area-integrating, touch screen monitor that displays a central fixation point and movable horizontal or vertical raster lines. This allows subjects to more precisely outline the boundaries of their scotoma in comparison to an Amsler grid. Additionally, spectral separation diminishes media influences such as confounding age-related cataract. Scotomas within the central 20-degree visual field were assessed at 5 contrast levels (20,40,60,80 and 100% full contrast).
Other supplementary tests used in the ZVF study include: 1⁰ MPOD using the QuantifEye® heterochromatic flicker photometry (ZeaVision Chesterfield, MO), low- and high-contrast visual acuity, glare recovery, and photopic contrast sensitivity function using the Optec Plus (Stereo Optical, Chicago, IL, USA), auto fluorescence of the retina using the Optos 200Tx® (Optos, Dunfermline, Scotland, UK), color contrast sensitivity using the 6° blue cone Chroma Test® Color, foveal shape discrimination (Retina Foundation of the Southwest, Dallas, TX, USA), and the National Eye Institute VFQ25 visual function questionnaire. Some of these results are mentioned parenthetically in the results. We evaluated the subset of 25 patients in the ZVF Study that received 8mg of dietary Z supplementation for 12 months. These 25 patients were retrospectively analyzed for central foveal dip in their macular pigment architecture, with five subjects demonstrating this dip phenomenon. In totality, 5/25 (20%) of the subjects presented with a dip in their central macular pigment, which is consistent with previously published findings on central dip incidence.4–7 This article presents the MPOD ARIS scans and kinetic central macular visual field tests from four subjects because the fifth was excluded due to extremely poor image quality caused by dense bilateral nuclear cataracts. The cohort receiving Z supplementation was retrospectively investigated apart from the other two groups because of the scarcity of peer-reviewed publications focusing on Z supplementation.
Case 1: Z32
79-year old Caucasian male with bilateral AMD (OS worse than OD), extensive bilateral drusen, mild bilateral cataracts, and poor baseline contrast sensitivity function (Figure 4a) details impressive bilateral gradual resolution of his central scotoma; (Figure 4b) details restoration of central macular pigment peak; color vision also demonstrated improvement; finally, the subject noted modest gains in the subjective visual field questionnaire.
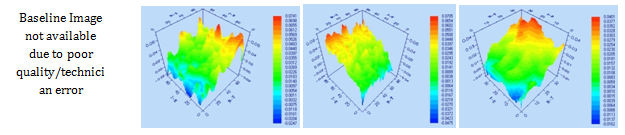
Figure 4a Case Z32 peak pigment at onset of study, 4 months, 8 months, and 12 months. The baseline measurement was unavailable due to poor quality.
Case 2: Z50
50-year old Caucasian female with progressively worsening night vision for approximately 30 years despite excellent visual acuity Figure 5a shows clearing of her central foveal kinetic visual field defect while Figure 5b shows significant rebuilding of the central macular pigment peak. Z50 also showed reduced lipofuscin in autofluorescence images along with improved photopic contrast sensitivity function, Chroma Test color contrast sensitivity, and foveal shape discrimination.
Case 3: Z55
80-year old Caucasian male with OD AMD w/lipofuscin activity Figure 6a illustrates gradual but continuous improvement in his right kinetic visual field, which corresponds with similar gains in Amsler Grid tests and the visual field questionnaire. Figure 6b shows development of better peak macular pigment architecture. Additionally, patient Z55’s photopic contrast sensitivity function displayed dramatic improvement over the 12-month study.
Case 4: Z58
87-year old Caucasian male w/ OD: combined AMD and early macula hole formation. Figure 7a details significant reduction of his scotoma and Figure 7b shows the development of a preferred central peak of macular pigment contrasting with the broader plateau-like distribution of the baseline image. Patient Z58 also exhibited increases in Amsler Grid and color vision test results. Notably, each Z-dip patient experienced improvement in one or more visual parameters: three of four subjects improved their color vision as measured by the 6° blue cone color Chroma Test, two showed better contrast sensitivity function, two demonstrated faster glare recovery, and one experienced increased foveal shape discrimination.
There have been several attempts to identify Mz in human food sources but little consensus has been reached.18–23 Currently the balance of evidence suggests that Mz is present in the skin of a handful of marine species, though the quantities of Mz present in these sources is under dispute. Even the most optimistic data shows only 0.2 mg of Mz present in an entire medium-sized trout weighing approximately 200g.24 Considering a standard western diet, the trace amount of Mz in food sources makes consumption of dietary Mz functionally zero. Given Mz’s key role in central macular health, the paucity of dietary Mz suggests an alternative source(s) of retinal Mz. This hypothesis is supported by undetectable Mz levels in serum unless Mz supplements have been recently consumed. Additionally, the macula is the only tissue in the human body containing stores of Mz.25 This stands in contrast to Z, which has been found throughout the body and has multiple functions, including photoprotective benefits within skin,26 aiding brain development in juveniles,27 maintaining cognitive function 14 and slowing memory decline28 in adults.
It has been long suggested that the major source of macular Mz in primates is enzymatically-derived from L.10 The physiological mechanism of this process was not understood until recently when Bernstein et al.,29 identified the enzyme that converts L to Mz as RPE65, or retinoid isomerohydrolase. RPE65 is located within the RPE layer and is vital for the conversion of all trans-retinyl esters to 11-cis-retinol, making it a key enzyme in the visual cycle occurring in photoreceptive cells. RPE65 has been well-researched but Mz isomerization is a secondary enzymatic activity that has not been studied extensively; the full text from Bernstein et al.,29 has yet to be published. The identification of the central dip in macular pigment in patients with AMD is a relatively recent discovery; as such there are a very limited number of peer-reviewed articles investigating treatment options. The first study to investigate the effects of carotenoid supplementation on patients exhibiting the macular dip phenomenon was published by Nolan et al.,30 in October 2016. Subjects were divided into three groups, each receiving a different ratio of carotenoid supplementation over an 8-week period. MPOD levels were measured at 0.25°, 0.5°, 1.0°, 1.75° and 3.0° of retinal eccentricity by the method of heterochromatic flicker photometry. The cohort receiving 10 mg L, 2 mg Z, and 2 mg Mz produced statistically significant gains in MPOD at only the 0.25° retinal eccentricity. Supplementation with 20 mg L, 2mg Z, and zero Mz or 3mg L, 2 mg Z, and 17 mg Mz did not produce statistically significant results at any eccentricity.
The most recent research on carotenoid supplementation comes from the 24-month longitudinal Central Retinal Enrichment Supplementation Trial (CREST).31 Subjects with early AMD were assigned one of two supplements: the AREDS2 formula or the AREDS2 formula plus 10 mg Mz. The patients that received Mz supplementation showed no additional benefits in visual performance or macular pigment when compared to the subjects that received the traditional AREDS2 formula. Taken together, the respective papers by Nolan et al.,30 and Akuffo et al.,31 provide important insight in understanding how carotenoid supplementation affects AMD progression, but they ignore the effects of dietary Z in re-pigmenting the macula by using a small and non-variable supplemental dose of Z. Xanthophyll carotenoids were initially thought to be absorbed by passive diffusion, but identification of apical membrane transporters in intestinal enterocytes now point to an active absorption process.32 This is supported by research demonstrating competitive inhibition between carotenoids,33 though the details of this physiological mechanism are still being researched. Carotenoid bioavailability is a complex, multifactorial process influenced by the quantity and species of carotenoids consumed, whether carotenoids are consumed with fat and/or fiber,34 the presence of key vitamins and nutrients that act as co-factors 35, serum HDL levels, body fat percentage, and endogenous carotenoid stores.36
Like Mz, Z is most highly concentrated in the central foveola, though very few studies have isolated dosing effects of dietary Z on retinal health. Research has demonstrated that carotenoid supplementation increases MPOD in patients with AMD, yet little is understood about re-pigmenting targeted regions within the macula. Furthermore, the handful of studies that have investigated carotenoid supplementation almost universally utilize a L:Z:Mz ratio of 10:2:0. This was the ratio used in the AREDS2 study35 and is based on the average ratio of dietary xanthophyll carotenoid consumption in the United States. Interestingly, the serum ratio of these carotenoids is 3:1:0,37 yet no trial has ever supplemented at this ratio. Although the link between dietary carotenoid supplementation and reduced risk of ocular disease is robust, the interactions between the three macular carotenoids as well as their individual roles within specific areas of the retina (e.g. the foveola) remain unclear.
Supplementation with Z has been shown to improve visual performance and suppress retinal neovascularization that is characteristic of advanced AMD38 while yielding a lower cost-utility ratio than identical treatments without Z supplementation.39 The authors believe this paper provides the first evidence of resolution of a central dip in macular pigment density from dietary Z supplementation. The ongoing debate over the efficacy of dietary Z versus supra-physiologic/pharmacologic doses of Mz in re-pigmenting the macula remains open to further scientific inquiry, as the few investigations into Mz supplementation have produced contradictory results.30,31 These issues encompass the larger question of whether the two carotenoids ubiquitous in the human diet (L and Z) are sufficient to address age-related macular degeneration, or if Mz must be included as well. When considered in the context of recent publications such as the CREST study31 and Bernstein et al.,29 the findings of this study justify further research into the role of Z versus Mz in re-pigmenting the foveola, particularly in patients that demonstrate a central dip in MPOD. These results warrant investigation into supplementation of Z at higher dosages than the L:Z: Mz ratio of 10:2:0, which has become the de facto standard following the landmark AREDS2 study.35 The authors suggest a double-blind, randomized, placebo-controlled study that investigates higher doses of supplemental Z, using the serum ratio of 3:1:0 as a minimum. Future prospective studies utilizing larger sample sizes and variable doses of Z would provide key insight into the relative roles of the three xanthophyll carotenoids in retinal health, regardless of underlying macular pigment architecture.
This article and the medical cases reported within represent further analysis of the published ZVF study (ZVF-FDA IND #78, 973), which was approved by the Human Subjects and Research and Development IRB of the Department of Veterans Affairs. This work is supported by the Optometry/Ophthalmology sections of the Captain James A. Lovell Federal Health Care Center, a Department of Veterans Affairs and Department of Defense/US Navy Medical Center located in North Chicago, Illinois, USA.
SR is the global scientific research director of the Zeaxanthin Trade Association. DG is the Co-founder, Chairman and Chief Science Officer at ZeaVision. The remaining authors declare no conflicts of interest.
None.

©2017 Richer, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.