Advances in
eISSN: 2377-4290


Research Article Volume 2 Issue 5
The University of Melbourne, Australia
Correspondence: Rahul Chakrabarti, Centre for Eye Research, Australia, Royal Victorian Eye and Ear Hospital, Level 1, 32 Gisborne Street East Melbourne, Victoria, 3002, Australia, Tel +613 9929 8374, Fax +613 9662 3859
Received: June 04, 2015 | Published: June 29, 2015
Citation: Chakrabarti R, Roufail E. Posterior pole detachment technique for the management of full thickness macular hole. Adv Ophthalmol Vis Syst. 2015;2(5):149-153. DOI: 10.15406/aovs.2015.02.00058
Purpose, To investigate the clinical characteristics, visual and anatomical outcomes of a series of large full thickness macular holes treated by vitrectomy, ILM peeling and gas tamponade augmented by retina expansion.
Methods, Prospective, non-comparative, interventional case series of seven eyes of seven patients with Gass Stage 3 or above full thickness macular hole presenting to a vitreo-retinal unit of a tertiary eye hospital. All patients underwent 23 gauge pars plana vitrectomy, peeling of the internal limiting membrane, retina expansion through detachment of the posterior pole with injection of balanced salt via a 41-gauge subretinal cannula, and gas tamponade with sulfur hexafluoride gas. The main outcome measures were, anatomical closure of the macular hole and post-operative visual acuity.
Results, Six cases were Gass Stage 3, and one Gass Stage 4. Preoperative visual acuity ranged from hand movement to 6/36. Patients were followed post operatively for a minimum of 6 months. Anatomical closure of the full-thickness macular hole was successfully achieved and confirmed on optical coherence tomography in six of the seven cases. All patients in our case-series recorded improved visual acuity by 6 months follow up. Six patients attained a post-operative best corrected Snellen visual acuity of 6/24 or better.
Conclusion, The retina expansion technique has demonstrated promising results in improving anatomic and visual outcomes in patients with large, chronic, full thickness macular hole. The proposed mechanism is the undermining of the retina by fluid to facilitate approximation of the hole edge and aid migration of glial cells to close the foveal defect.
Keywords: full thickness, macular hole, vitrectomy, surgery, outcomes
ERM, epiretinal membrane; FTMH, full thickness macular hole; ILM, internal limiting membrane; OCT, optical coherence tomography; PPV, pars plana vitrectomy; PVD, posterior vitreous detachment; RRD, rhegmatogenous retinal detachment; SF6, sulfur hexafluoride
Full thickness macular holes have an estimated prevalence of 1/3300, with more than fifty percent occurring in patients aged 65-74 years.1 The vast majority (>80%) are idiopathic, with smaller proportions occurring in the setting of trauma, inflammation, and myopia. Furthermore, it is estimated that even fewer (less than 1% of full thickness macular holes (FTMH)) have been reported in association with both macular on and off retinal detachments treated with vitrectomy or scleral buckling alone.2,3 Once FTMH develops few spontaneously close, with the majority requiring vitrectomy, ILM peeling and gas tamponade. For most macular holes this approach usually results in successful hole closure and improving vision.4–6 However, patients with large (>400μm), chronic, full thickness macular holes are the exception. In this subgroup there is a significantly higher surgical failure rate and poorer visual outcomes with reoperation required.7–9
The poor surgical outcomes in this subgroup of macular hole patients have stimulated the consideration of novel surgical approaches to treat this clinically important subset of patients. In recent years these modifications have included massaging the retina around the hole,10 using an inverted flap of ILM remnant to cover the macular hole11 and laser photocoagulation at the centre of the macular hole before vitrectomy.12 In addition attempts have been made to close these large full thickness defects by inducing a posterior pole detachment by injection of sub-retinal fluid using a 41 gauge needle, the ‘retina expansion technique’.13 The current study reports our experience with the retina expansion technique in patients with large idiopathic, traumatic and post rhegmatogenous retinal detachment (RRD) full thickness macular hole.
The study was performed as a prospective, non-comparative case series of patients with large FTMHs who were referred to a tertiary eye hospital in Australia. All patients underwent a comprehensive ophthalmic examination by a vitreoretinal surgeon prior to surgery. Formal Gass grading of the macular hole was performed by measuring the basal diameter of the hole from preoperative optical coherence tomography (OCT). All patients were followed up from the time of first consultation to a minimum period of 6 months postoperatively.
Patient data recorded were age, gender, the mechanism (traumatic, idiopathic, RRD), examination findings, maximum hole diameter, Gass grading, pre and post-operative visual acuity, intraocular pressure, the time interval from trauma to surgery, and period of follow up. Surgical data recorded included presence of attached hyaloid, epiretinal membrane (ERM), successful removal of the hyaloid, type and concentration of gas tamponade.
Preoperative factors
In the current series three of seven cases were idiopathic FTMH. Two cases were secondary to blunt trauma in the context of a soccer ball and an elastic strap striking the globe. One case is of a FTMH occurring after vitrectomy for a macula-off RRD. The seventh case occurred in a patient with macular telangiectasia. The preoperative and surgical characteristics are summarised in Table 1. Five cases were male, and the sample age range was 13 to 78 years. The preoperative visual acuity of patients at the time of first presentation ranged from hand movement to 6/36. The time from loss of vision to surgery ranged from 3 to 20 months. Six patients were recorded with Gass Stage 3, and one with Gass Stage 4 macular hole.
Case |
Mechanism of injury |
Age |
Gender |
Hole size |
Eye Involved |
Preoperative clinical comments |
Initial visual acuity |
Final visual acuity |
Time from trauma to surgery |
Post-operative follow up |
Surgical technique |
Primary hole closure |
1 |
Blunt Trauma: Soccer ball |
13 |
M |
724 µm |
OS |
Traumatic FTMH |
6/36 |
6/24 |
17 |
18 |
Posterior pole detachment with 41-gauge cannula |
Closed |
2 |
Blunt trauma: |
36 |
F |
526 µm |
OS |
|
6/38 |
6/9 |
8 |
16 |
|
Closed |
3 |
Idiopathic |
64 |
M |
520 µm |
OD |
|
6/30 |
6/24 |
20 |
14 |
|
Closed |
4 |
Idiopathic |
74 |
M |
413 µm |
OS |
|
6/60 |
6/24 |
3 |
16 |
|
Closed |
5 |
Post macular-off rhegmatogenous retinal detachment |
71 |
M
|
488 µm |
OD |
|
HM |
1/60 |
9 |
18 |
|
Failed to close Failed to close |
6 |
Idiopathic |
78 |
M |
650 µm |
OD |
- |
6/60 |
6/24 |
8 |
28 |
|
Closed |
7 |
Macular telangiectasia |
70 |
F |
789 µm |
OD |
- |
2/60 |
6/18 |
6 |
6 |
|
Closed |
Table 1 Case series patient data of full thickness macular holes closed using the retina expansion technique
TMH, traumatic macular hole; PPV, pars plana vitrectomy; PVD, posterior vitreous detachment induced; ILM, internal limiting membrane; SF6, sulfa hexafluoride gas, HM, hand movements
Surgical technique
All surgeries described were performed by the same surgeon (ER). A 23 gauge, 3-port pars plana vitrectomy (PPV), with induction of a PVD (if incomplete), internal limiting membrane (ILM) peel after staining with Brilliant Peel(R) (Geuder, Germany), posterior pole detachment with sub-retinal fluid injected via 41G needle, fluid-air exchange, and gas tamponade with short-acting 30% sulphur hexafluoride (SF6) gas was performed. Fluid was left to slowly absorb postoperatively.
The ILM was peeled in six of seven cases to a size of at least 1.5 disc diameters from the foveal centre. In the case of the FTMH after macula-off RRD the ILM had already been peeled at the first attempt to close the hole. Induction of PVD was required in six cases. In all the cases, the Retina Expansion method was adopted to assist closure of the FTMH. The technique involved injecting balanced salt with the viscous fluid injector via a 41 gauge sub-retinal cannula into the perifoveal region (>500um from foveal centre). In each case multiple sites in the para fovea were injected with balanced salt to induce a posterior pole detachment. There was no massaging of retina as has been described previously 13. The fluid air exchange at the end of the procedure allowed all the multiple injection sites to coalesce into a confluent detachment of the posterior pole. Patients were advised to posture sitting up and leaning forward for a period of 7 days post operatively (Figure 1&2).
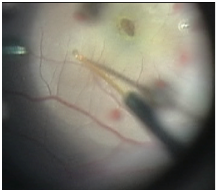
Figure 1 Still from video demonstrating parafoveal injection of balanced salt using 41 gauge sub-retinal cannula.
Postoperative outcomes
Routine post-operative assessment of patients at day one involved measurement of visual acuity, applanation tonometry, and indirect ophthalmoscopy by the vitreoretinal surgeon. Follow up for all patients occurred at minimum at one week, one month, three months, and extended up to eighteen months. There were no cases of vision loss, rhegmatogenous detachment or endophthalmitis.
Macular hole closure after primary surgery
Anatomic closure of the macular hole was assessed by Macular OCT (Cirrus HD-OCT 400, Carl Zeiss Meditec, Inc. Germany) performed by one masked observer. Closure was defined when the entire circumference of the macular hole flattened against the retinal pigment epithelial layer (base-width). In this series FTMH closure was achieved in six of the seven patients after primary surgery (Figures 3&4).
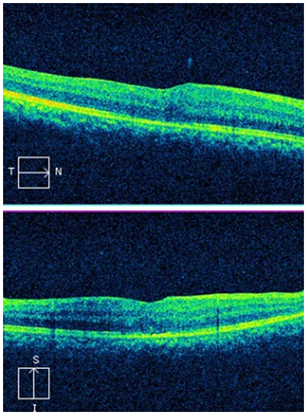
Figure 4 Postoperative OCT of case 1 demonstrating closure of full thickness macular whole and minimal pigment epithelium thickening.
Post-operative visual acuity
All patients in our case-series recorded improved visual acuity by 6 months follow up. Six patients attained a post-operative best corrected Snellen visual acuity of 6/24 or better.
Case 1
The largest FTMH defect observed in this series was 724µm, observed in a 13 year old male. The patient had been struck by a soccer ball to the left eye, and had a period of 17 months from time of injury to surgery. Preoperative visual acuity was 6/36 in the left eye, and examination revealed a FTMH with no PVD, and extensive peripheral “leopard spotting” appearance consistent with previous commotio retinae. No other ocular injury was evident. Given the interval to surgery, the size of the hole and the absence of other injuries the retina expansion approach was used. At one week post-operatively the hole was noted to have closed. Follow up of the patient at routine intervals over the next 12 months demonstrated the hole had remained closed, and the final visual acuity was 6/24 in the left eye.
Case 2
The case in which the retina expansion technique failed to close the FTMH in this case series involved a previously well 71 year old male with 6/6 visual acuity in both eyes. The patient presented initially with a macular-off rhegmatogenous retinal detachment in the right eye that was treated with 23 gauge pars plana vitrectomy, endolaser, cryopexy and 30% SF6 gas. At one month post surgery of the RRD the patient’s vision had deteriorated to counting fingers, and clinical examination revealed a 488μm FTMH had developed. Six weeks after the first procedure the patient underwent an attempt to repair the macular hole using a 23-gauge vitrectomy approach, peeling of the ILM, 30% SF6 gas and face-down posturing for 4 hours. However, the FTMH failed to close and vision remained 1/60. A second attempt at closing the FTMH using the retina expansion technique was undertaken four months post primary vitrectomy. Despite this, the FTMH had failed to close and visual acuity remained 1/60 in the right eye. Failure to close the FMTH in this case was likely due to retinal stiffness, a probable manifestation of very mild proliferative vitreoretinopathy. Given the excellent vision in his unaffected (left) eye, no further attempt to close the hole was undertaken.
Whilst surgery for macular holes and their outcomes has been well described in the literature there is a paucity of evidence concerning the management of large, chronic, full-thickness macular holes, particularly in the setting of trauma. This has led to a growing body of interest in modified approaches to the traditional surgical technique to augment anatomical closure and improve vision. This case series demonstrated the potential for the retinal expansion technique to achieve hole closure in a subgroup where traditionally poor results are expected.14 Predictors of poorer anatomical and visual outcomes of full thickness macule hole described in the literature are greater pathological severity (Stage 3 and above compared to Stage 1 and 2), and longer preoperative duration (particularly > 24 months).15,16 However, we achieved hole closure and improved visual acuity in six out of seven cases after the primary vitrectomy procedure augmented by retinal expansion. The results showed that despite variation in hole diameter and pathological grade, preoperative visual acuity and timing of surgery, this approach still delivered comparable anatomical and visual outcomes to the series of idiopathic holes treated with this technique described by Wong.13 Compared to Wong, we used a shorter acting gas (SF6 compared to C3F8), did not manually manipulate or massage the retina, and patients were not routinely postured. Additionally, we observed that anatomical closure and improved vision was achieved using this technique amongst patients with traumatic FTMH. Whilst our sample is small, it adds to the body of knowledge to show that this approach can be applied in the management of blunt trauma related macular hole.
It is well known that strategies to promote or facilitate migration of glial cells to the edges of the macular hole assist in anatomical closure. The retina expansion approach aimed to utilise the inherent elastic properties of the retina to appose the edges of the hole. Yamada et al postulated that migration of glial cells or retinal pigment epithelium to the banks of the hole edges was critical in facilitating hole closure in a series of spontaneous TMH closures in patients with an absence of an operculum or epiretinal membrane.17 This has served as the basis for several novel approaches for macular hole surgery. Alpatov et al.10 attempted to massage the retina gently around the hole from the periphery and then mechanically appose the edges with forceps, followed by intravitreal air tamponade. Compared to a conventional technique this had comparable anatomical closure and a small improvement in visual acuity. However, this was associated with retinal pigment epitheliopathy caused by the mechanical manipulation. Michalewska et al.11 proposed the inverted ILM flap approach whereby a segment of the peeled ILM was left attached to provoke gliosis and act as a scaffold for tissue proliferation at the edges of the hole. However, a practical limitation of this technique was the observation that 14% of the inverted ILM flaps detached spontaneously during the air-fluid exchange. Similarly, Cho et al.12 performed a randomised control trial using three argon laser burns directed toward the RPE at the centre of the macular hole in attempt to promote the formation of a glial plug. The authors demonstrated a higher proportion of hole closure and greater magnitude of improvement in visual acuity in the group undergoing vitrectomy plus laser compared to vitrectomy alone.
Fundamentally, these alternative approaches have attempted to modify the method by which large macular holes close. OCT studies have demonstrated that frequently large macular holes have flat borders with bare RPE (flat-open macular hole);9 and that closure of macular holes in this manner may limit visual acuity.8 It is postulated that the mechanism of the retina expansion technique is the undermining of the retina by fluid in the same way that a tight skin wound may be undermined to facilitate wound edge apposition. An important limitation of the retina expansion approach is that by detaching the posterior pole, there is disruption to the photoreceptor-RPE interface. Thus, any pre-existing damage at this neural and pigmentary retinal interface may further compromise successful anatomical closure. This may explain why the FTMH in the patient described in Case 5 failed to close despite two attempts. However, given that over 40% of patients with macula-off rhegmatogenous retinal detachments still attain final central vision of better than or equal to 20/50 it support the theory that photoreceptor outer segment preservation can still be achieved.18
In conclusion, the retina expansion technique has demonstrated promising results with improved anatomic and visual outcomes in patients with large, chronic, FTMH. Our case series with a small, yet heterogenous sample of cases demonstrated a comparably safe and reproducible technique involving posterior pole detachment without face-down posturing that improved visual acuity. However, future studies should incorporate a control group and physiological assessments of the fovea in order to verify the long-term visual function implication of this technique. This would also shed insight into the trade-off between early anatomical closures with this approach versus the physiological impact of posterior pole detachment.
None.
Author declares that there is no conflict of interest.

©2015 Chakrabarti, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.