Advances in
eISSN: 2377-4290


Research Article Volume 6 Issue 6
1Vision Ooglaseren Netherlands
2Clinica Baviera Spain
3Abu Dhabi Police Medical Service LASIK Unit UAE
4Alrijne Ziekenhuis Netherlands
5Leids Universitair Medisch Centrum Netherlands
Correspondence: Jos R Villada Vision Ooglaseren Assumburg 150 1081 GC Amsterdam Netherlands, Tel +31 203010812
Received: April 03, 2017 | Published: April 24, 2017
Citation: Mrcophth JVM, Bilbao R, Acebal M, Llama ADL, Lamme M (2017) Photorefractive Keratectomy (PRK) Retreatment of Residual Refractive Errors after Laser in Situ Keratomileusis (LASIK). Adv Ophthalmol Vis Syst 6(6): 00200 DOI: 10.15406/aovs.2017.06.00200
Purpose: This study aims to present the results of PRK treatment for residual errors after previous laser in situ keratomileusis (LASIK) in a large number of eyes.
Methods: Retrospective review of case notes of patients operated with this technique in our institution, during the period 2005-2014, with at least 2 years follow-up.
Results: Five hundred and thirty eyes were included in the study. Mean UCDVA improved from logMAR 0,28 to logMAR 0,15 after PRK retreatment. Mean BCDVA decreased slightly from logMAR 0,02 to logMAR 0,04. Ninety five percent of the eyes maintained or gained lines of BCDVA, while 2% of the eyes lost 2 or more lines of vision. Eighty seven percent of the eyes were within 1 diopter of desired refraction, while 5% had a refractive surprise of more than 3 diopters. Safety and efficacy were greater when treating myopic eyes (safety index 1,12, efficacy index 0,83) than when treating hyperopic eyes (safety index 0,95, efficacy index 0,66).
Conclusion: PRK is a good alternative for the retreatment of refractive errors after LASIK when a flap lift treatment is not recommended. The results in myopic eyes are comparable to primary myopic PRK treatment. The results in hyperopic eyes are inferior to primary hyperopic treatment. The possibility of a refractive surprise can be an issue and should be discussed with the patient prior to treatment.
Keywords: PRK, LASIK, laser-retreatment
Laser in situ keratomileusis (LASIK) is the most frequently performed corneal refractive procedure. Despite technological improvements, residual postoperative refractive errors are still an issue that needs to be dealt with, especially when they interfere with the patient´s quality of life. Retreatment after LASIK is commonly performed by lifting the flap created during the first operation followed by further application of laser. Other possible techniques are: creating a new flap, performing incisional treatment, or performing a PRK. More remote options are inserting a phakic intraocular lens (IOL) or performing surgery over the crystalline lens. These two last options are reserved for much larger errors or those cases in which further laser is not a possibility. The choice is usually between lifting the flap and performing a PRK over the flap. Febbraro1 & Agarwal2 described the advantages and disadvantages of both options. PRK retreatment is known to potentially cause haze/corneal scarring, more frequent regression, tissue melting, irregular astigmatism and overcorrection. LASIK retreatment may cause dry eye syndrome, flap striae, epithelial in growth and mechanical flap tearing.3,4 LASIK retreatment is also claimed to be more predictable than PRK retreatment,5 and infections are more likely to happen after PRK6 than after LASIK.7 Relifting a flap is not always possible due, in most occasions, to the time passed between the first operation and the second treatment and, sometimes, even if it is surgically possible, it is not recommended because of one of the following reasons:
PRK after previous LASIK was strongly dis-recommended by some authors8 after severe complications, and during some time considered a “forbidden” procedure. More recently, some publications including a small number of eyes have not reported significant complications.9‒17 In our clinic we have had to deal with a large amount of a patients whose flap thickness was not measured during the first treatment (LASIK) and therefore were retreated with PRK. In this paper we review all these PRK retreatments and the results obtained.
This is a retrospective review of cases that having had a primary excimer laser treatment for their refractive error by a LASIK technique underwent an enhancement procedure using PRK. All cases retreated between 2005 and 2012 with at least two years follow-up after the PRK treatment, were included in the study. Procedure, refractive results and intra and postoperative complications were analysed. The initial surgical technique used was a standard LASIK procedure, creating the flap with a microkeratome and following the usual postoperative regime with antibiotics and steroids for one week and artificial tears for three to six months. Eyes with any kind of complications in this first procedure were excluded from the study. PRK was performed in all retreatments. The traditional technique with alcohol 20% applied inside an 8 millimetres corneal marker centred on the pupil and left for 30 seconds was followed in most cases. In the 44 cases performed by one of the authors (JRV) a merocel sponge with a technique described elsewhere,18 followed by peeling of the weakened epithelium was used. All the PRK cases received mitomycin C 0,02% immediately after the laser during a mean time of 37 seconds (SD 32, range 10-120 seconds) and had a bandage contact lens for 4-5 days. Four eyes received a wavefront-guided treatment while the others had a standard plano-scan treatment. The postoperative medication after PRK was also standard for all patients: topical ofloxacin 3 mg/mL 4 times a day for 2 weeks, topical sodium diclofenac 0,1% 4 times a day for 5 days or until the epithelium was closed and fluorometholone 0,1% eye drops 4 times a day and tapering off during 3 months. There were no reported complications in the enhancement treatments.
Five hundred and thirty eyes from three hundred and twelve patients were included in the study. One hundred and sixty nine (54,16%) were female. The age ranged from 23 to 71 years, the mean being 45,29 years (SD 10,55). There were 239 right eyes and 291 left eyes. The mean pre-LASIK spherical equivalent was -3,77 diopters (SD 3,08; range +5,25 to -9,63 diopters). Primary LASIK treatment was performed by 12 different surgeons, using one of three different microkeratomes: Moria Two (520 instances), Moria One (6 instances) or Hansatome (4 instances); and two different excimer lasers: the Technolas 217z and Allegretto Eye-Q 100 Hz. The mean preoperative logMAR best corrected distance visual acuity (BCDVA) prior to LASIK, was 0 (SD 0,077). The mean logMAR uncorrected distance visual acuity (UCDVA) was 1,23 (SD 0,452). The mean logMAR UCDVA improved to 0,28 after LASIK while the logMAR BCDVA remained 0,02 (SD 0,075).
The flap thickness was calculated intraoperative in only 15 eyes (2,83%) with a mean of 106 microns (SD 49; range 44 to 200). The mean central corneal thickness (CCT) prior to LASIK was 562 microns (SD 32; range 479 to 653) and the mean central tissue ablated was 68,22 microns (SD 28, range 7 to 147). Mean residual error after the primary LASIK was -0,55 diopters (SD 0,97; range +2,75 to -3,25). PRK retreatment after primary LASIK was performed by 11 different surgeons. Two hundred and seventy nine eyes were treated for a myopic spherical equivalent, 113 for a hyperopic spherical equivalent and 10 eyes were treated for mixed astigmatism with 0 spherical equivalent. The mean time from primary LASIK to PRK enhancement was 46,24 months (SD 27,75; range 3 to 202 months).
Visual acuity
The mean logMAR UCDVA improved from 0,28 to 0,15 (SD 0,15) after PRK treatment and the logMAR BCDVA decreased slightly from 0,02 to 0,04 (SD 0,12). Table 1 shows the change in visual acuity values after both procedures.
|
UCDVA logMAR |
BCDVA logMAR |
Pre LASIK data |
1,23 (0,45) |
0 (0,07) |
Post LASIK data |
0,28 (0,2) |
0,02 (0,07) |
Post surface treatment data |
0,15 (0,18) |
0,04 (0,12) |
Table 1 Visual acuity data pre and after both procedures when including all data
Safety
The safety index for all the eyes was 1,07. If we subdivide the eyes into myopic, hyperopic and zero SE, the safety indexes were 1,12; 0,95 and 1,12 respectively. Figure 1 shows the change in corrected visual acuity. Four point five per cent of eyes lost lines of vision, 2% lost 2 or more lines of vision. Ninety five point five per cent of eyes remained with the same vision or gained lines of best corrected vision. Two of the eyes that lost 3 lines of vision did so due to significant cataracts and the third one due to severe dryness.
Efficacy
The efficacy index for all the eyes was 0,71. If we subdivide the eyes into myopic, hyperopic and zero SE, the efficacy indexes were 0,83; 0,66 and 0,9 respectively. Figure 2 shows the cumulative preoperative BCDVA and postoperative UCDVA when considering all eyes. Eighty six per cent of the eyes could see 0,5 and 42% could see 1 without any correction after the PRK enhancement. Figures 3-5 show the cumulative preoperative BCDVA and postoperative UCDVA when considering only myopic eyes, only hyperopic eyes and zero SE respectively. For myopes 93% of the eyes could see 0,5 and 47% could see 1; for hyperopes 67% of the eyes could see 0,5 and 29% could see 1; and for zero SE eyes, 100% of the eyes could see 0,5 and 50% could see 1. Figure 6 shows the attempted versus achieved postoperative spherical equivalent, for all eyes. The correlation coefficient was 0,65, the slope 1,11 and the y-intercept 0,15. Figure 7 shows the spherical equivalent refractive accuracy for all eyes, 63% of them were within 0,5 diopters and 87% within 1 diopter of attempted refraction. There were 5 eyes of 4 patients with a refractive surprise of more than 2 diopters. The details of these eyes are depicted in Table 2. The mean optical zone (OZ) used in the first treatment was 6,08 mm, while the mean OZ used in the second treatment was 6,17 mm. Forty six point five per cent of the eyes were retreated with the same OZ, 33% with a bigger OZ and 20,5% with a smaller OZ. The change of optical zone did not influence the final UCDVA or SE
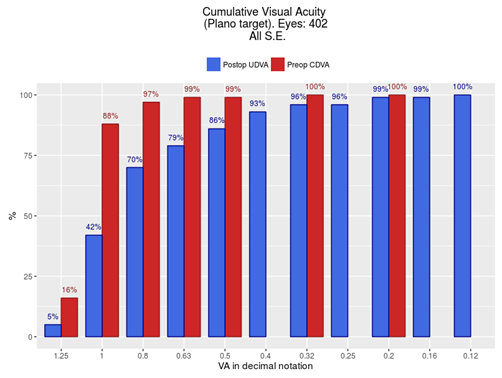
Figure 2 Comparison of cumulative visual acuity between preoperative corrected visual acuity and postoperative uncorrected visual acuity including all eyes.
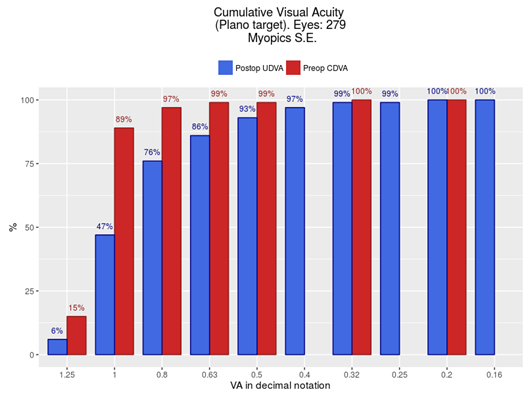
Figure 3 Comparison of cumulative visual acuity between preoperative corrected visual acuity and postoperative uncorrected visual acuity, when considering only myopic retreatments.
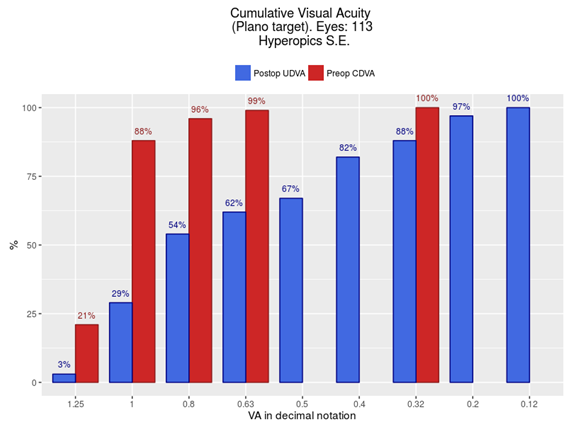
Figure 4 Comparison of cumulative visual acuity between preoperative corrected visual acuity and postoperative uncorrected visual acuity, when considering only hyperopic retreatments.
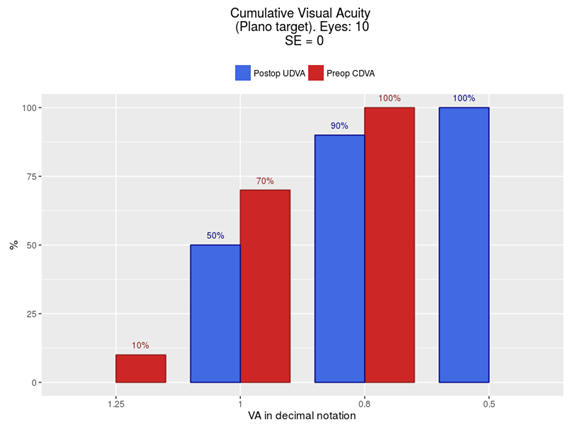
Figure 5 Comparison of cumulative visual acuity between preoperative corrected visual acuity and postoperative uncorrected visual acuity, when considering only zero spherical equivalent eyes.
Author |
Year |
No eyes |
UCDVA = 1 |
UCDVA ≥ 0,5 |
± 0,5 Diopters |
± 1 Diopters |
Safety index |
Efficacy index |
≥ 2 Lines iost |
Complications |
|
CARONES |
2001 |
17, all Myopes |
|
|
|
|
|
|
82,3% |
Severe haze |
|
SHAIKH |
2005 |
15*, 11 Myopes and 4 hyperopes |
40% |
87 % |
40% |
60 % |
|
|
None |
Not significant |
|
CAGIL |
2007 |
24, No separated results |
|
87,5 % |
|
|
|
|
4,15 % |
1 Severe haze |
|
BEERTHUIZEN |
2007 |
18, No separated results |
67% |
92% |
83% |
100% |
1,03 |
1,11 |
None |
2 Significant haze |
|
NEIRA-ZALENTIN |
2008 |
3 Hyperopes |
|
|
100 % |
|
|
|
|
Not significant |
|
|
|
4 Myopes |
|
|
50 % |
75 % |
|
|
|
Not significant |
|
SAEED |
2008 |
22, No separated results |
|
95,4 % |
55,4% |
77,3 % |
|
|
None |
Not significant |
|
SRINIVASAN |
2008 |
30, No separated results |
|
|
|
|
|
|
None |
None |
|
NG-DARJUAN |
2013 |
16 |
|
88% |
56 % |
94 % |
|
|
None |
None |
|
LEE |
2014 |
14 Hyperopes |
50 % |
100 % |
|
|
|
|
|
6 Refractive surprises |
|
|
|
29 Myopes |
65,5 % |
100 % |
|
|
|
|
|
2 Refractive surprises |
|
Table 2 Safety and accuracy in previously published similar studies
Ninety one eyes (17,17%) were reported to have some degree of haze. Seventeen of them had haze grade 2 and 3 haze grade 3. No patients presented haze grade 4. Three eyes (0,57%) had an infectious keratitis. All 3 were treated with scrapping of the epithelium and fortified antibiotics. None of them lost lines of best corrected vision. Ectasia was not diagnosed in any of these eyes.
Thirty one eyes underwent further enhancement
Surface laser excimer re-treatment after previous LASIK seems to be more common than what the little research published about it shows (Fernando Mayordomo, Felix Gonzalez, Raul Casado, all personal communications). Güell19 and, much later Hara20 proposed a technique consisting in correcting the error directly over the epithelium. Hara20 who called the procedure E-PRK, claimed that its effect lasts for a mean of 2,75 months and can be repeated two or three times a year. Carones8 was the first to publish his results using PRK retreatment after previous LASIK. The results were devastating, with 82,3% of the eyes having severe haze after an initial promising period, and, they strongly recommended not to use this technique for re-treatments after LASIK. Mitomycin C was not used in any of the 17 eyes of the series. There have been several publications using surface retreatment after LASIK after Carones, most of them including only a limited number of eyes.9-17 Table 2 shows safety and accuracy data in these studies.
Our study includes a large number of eyes with at least 24 months follow-up. Safety index (mean postoperative BCDVA divided by mean preoperative BCDVA) was 1,07 when including all the eyes, 1,12 when including only myopic eyes and 0,95 when including hyperopic eyes. These results compared well with long term PRK for myopia or hyperopia studies. Shalchi21 found a safety index of 0,998 in eyes that underwent myopic PKR 18 years before, while Wahg22 found a safety index of 0,83 in eyes that underwent hyperopic PRK, with the same time follow-up. The only author mentioning safety index after surface retreatment after LASIK was Beerthuizen11 with an index of 1,03 in a mix of myopic and hyperopic eyes treated. Two per cent of the eyes in our study lost 2 or more lines of vision. Only 2 other authors reported eyes with 2 or more lines of vision lost. Cagil10 1 in 24 eyes (4,15%), due to severe haze, and Schalhorn17 with a percentage very similar to ours (2,34%) in an already significant number of eyes (171). Murray23 in a large review of PRK treated eyes in the literature, found 2 or more lines of vision lost in 0,5% of eyes after low to moderate myopia treatment and 7% after low to moderate hyperopia treatment.
Overall, 42% of our eyes had a UCDVA of 1 and 86% has a UCDVA of 0,5 or better. When taking into account only myopic treated eyes, the figures improves to 47% and 93% respectively, but for hyperopic treated eyes there only 29% of eyes with UCDVA of 1 and 67% with UCDVA of 0,5. These results are in general inferior to what other authors have published. Lee16 in the only study separating myopic and hyperopic treated eyes (14 hyperopic and 29 myopic) had 50% of hyperopic eyes with 1 UCDVA and 65,5% of eyes with 0,5 UCDVA. Sixty three per cent of our eyes were within 0,5 and 87% within 1 diopter of planned correction. Schalhorn17 in his study including 171 eyes found 84,2% of eyes within 0,5 and 97,7% of eyes with 1 diopter of planned refraction. The results found by Murray23 in her large review of the literature are also better than the ones in our study: 71,6% of eyes and 90,4% within 0,5 and 1 diopter respectively for low to moderate myopia, and 75,4% and 86,8% within 0,5 and 1 diopter respectively for low to moderate hyperopia.
Infectious keratitis, significant haze and refractive surprises were our more frequent postoperative complications, with 3 instances each. Table 3 shows the details of our 5 eyes with more than 2 diopters of refractive surprise; none of them had significant intra or peri-operative complications. We speculate that these changes could be due to abnormal epithelial healing. The complications rate for other authors was also low, Beerthuizen11 2 in 18 eyes severe haze and Lee16 8 in 43 refractive surprises were the more remarkable. Cagil10 has one eye out of 24 with severe haze that did not respond to treatment and dis-recommend this technique in eyes with more than -2 diopters error or those needing a central ablation greater than 40 microns. Neira-Zalentin12 did not report any significant complication in his series but recommends that PRK retreatments after LASIK are performed more than 2 years after the primary operation, when the corneal sub-basal nerve density has reached an adequate density.
Age |
Sex |
SPH EQ pre LASIK |
SPH EQ post LASIK |
Mytomicin time |
final SPH EQ |
Complications |
48 |
F |
-8,12 |
-1,75 |
30 |
+3,50 |
Nil |
|
|
-8,25 |
-2,12 |
30 |
+3,75 |
Nil |
63 |
M |
-4,75 |
+2,25 |
30 |
-2,25 |
Nil |
32 |
M |
-4,00 |
+0,75 |
30 |
-3.00 |
Haze grade 1 |
29 |
F |
-7,37 |
+0,75 |
30 |
-2,37 |
Nil |
Table 3 Data for the 5 eyes having a significant refractive surprise
Liu24 reports a case of visually significant haze after PRK for refractive error after LASIK. He claims a prolonged used of mitomycin C to avoid this complication. In resume PRK is a useful technique for the treatment of residual errors after primary LASIK. The results are satisfactory after myopic error but are more questionable when treating hyperopic errors. Our results in term of safety and accuracy are worse than in previously published papers, in which there are practically no complications. The only reason we can speculate is that this study includes a much greater number of eyes and in procedures with very small rates of complications this can be determinant. The most remarkable issue is the high proportion of refractive surprises, attributable probably to defective healing. The possible occurrence of these surprises and the possibility of other complications, more associated with PRK than with LASIK, like infections and haze should be discussed preoperatively with the patients together with the longer recovery period required for this technique.
None.
The authors declare there are no conflicts of interest.

©2017 Mrcophth, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.