Advances in
eISSN: 2377-4290


Case Report Volume 14 Issue 3
Vision Institute, Providencia, Santiago, Chile
Correspondence: Pérez Mauricio MD, Vision Institute, Providencia, Santiago, Chile, Postal code: 7500834, Tel +56977658 121
Received: October 01, 2024 | Published: October 24, 2024
Citation: Espinoza G, Pérez M. Paracentral acute middle maculopathy associated with non-arteritic ischemic optic neuropathy: a case report. Adv Ophthalmol Vis Syst. 2024;14(3):87-91. DOI: 10.15406/aovs.2024.14.00472
Objective: To describe a case of paracentral acute middle maculopathy (PAMM) associated with non-arteritic anterior ischemic optic neuropathy (NAION).
Methods: A 63-year-old patient presented with floaters (myodesopsia) and flashes of light (photopsia) associated with decreased visual acuity.
Results: The visual field test revealed a centrocecal defect, and optical coherence tomography (OCT) showed hyperreflective areas in the inner nuclear layer in the temporal parafoveal region, along with alterations related to edema in the neuroretinal ring (RDNFL) secondary to NAION. Hypoperfusion and reduced vascular density were noted in the parafoveal and choroidal regions, as well as in the optic nerve (ON).
Conclusion: Although there are no definitive treatments for these two pathologies, it is important to know how to interpret optical coherence tomography (OCT) and OCT angiography (OCTA). These non-invasive and reproducible techniques help monitor structural changes in these pathologies without the adverse effects of invasive tests.
Keywords: ischemic optic neuropathy, optic nerve ischemia, paracentral acute middle maculopathy, spectral domain optical coherence tomography, deep capillary ischemia, optical coherence tomography angiography
A 63-year-old male presented with sudden visual acuity loss associated with a 1-day history of left-sided headache, floaters (myodesopsia), and flashes of light (photopsia). His surgical history included bladder cancer 10 years ago, venous thrombosis associated with a venous catheter during chemotherapy (treated with heparin and later aspirin), and a cervical lymph node biopsy a month prior (with aspirin discontinued). He was on treatment with vitamin B12, bicarbonate, and rosuvastatin for mild dyslipidemia. No prior ophthalmological history.
On physical examination, the patient was overweight, alert, and oriented to time, place, and person. Visual acuity was 20/20 (+4.5 +0.50 10°) in the right eye (OD) and 20/25 (+4.75 +0.50 5°) in the left eye (OS). The visual field by confrontation revealed an apparent centrocecal scotoma in the left eye, with no relative afferent pupillary defect (RAPD). Cover test and eye movements were normal. Biomicroscopy was unremarkable, but fundus examination revealed optic nerve hyperemia with superior and nasal elevation in the left eye (OS). The macula in OS showed mild color changes (whitish-gray) and an isolated microhemorrhage in the superior papillomacular bundle.
The following tests were ordered: complete blood count, VDRL, FTA-ABS, biochemical profile, coagulation profile, lipid profile, antinuclear antibodies, anti-DNA antibodies, anti-cytoplasmic antibodies, anti-Bartonella antibodies, anti-Toxoplasma antibodies, complement C3-C4, lupus anticoagulant, anticardiolipin antibodies, Factor V Leiden, proteins C and S, metabolic profile, carotid Doppler ultrasound, cardiac ultrasound, and Holter monitoring. Additionally, fundus photography, autofluorescence (AF), computerized perimetry 24/2, optical coherence tomography (OCT), and OCT angiography (OCTA) were performed.
Fundus photography confirmed the macular findings, and AF showed hypoautofluorescent lesions over the optic nerve and macula (Figure 1). Computerized perimetry revealed a non-specific defect in OD and a centrocecal defect in OS (Figure 2). OCT of the optic nerve showed mild superior elevation in OS with RNFL analysis (Figure 3), and marked vascular density reduction in 360° in the optic nerve of OS (Figure 4). Macular OCT revealed an alteration in the external plexiform layer of OS with abundant temporal hyperreflective lesions, and a preserved foveal architecture in both eyes (Figure 5). OCTA of the macula showed a decrease in vascular density in the deep superior and choriocapillaris layers (Figure 6). Based on these findings, aspirin was reintroduced, and a follow-up was scheduled in 4 weeks with computerized perimetry, OCT, and OCTA, with a presumptive diagnosis of NAION and PAMM.
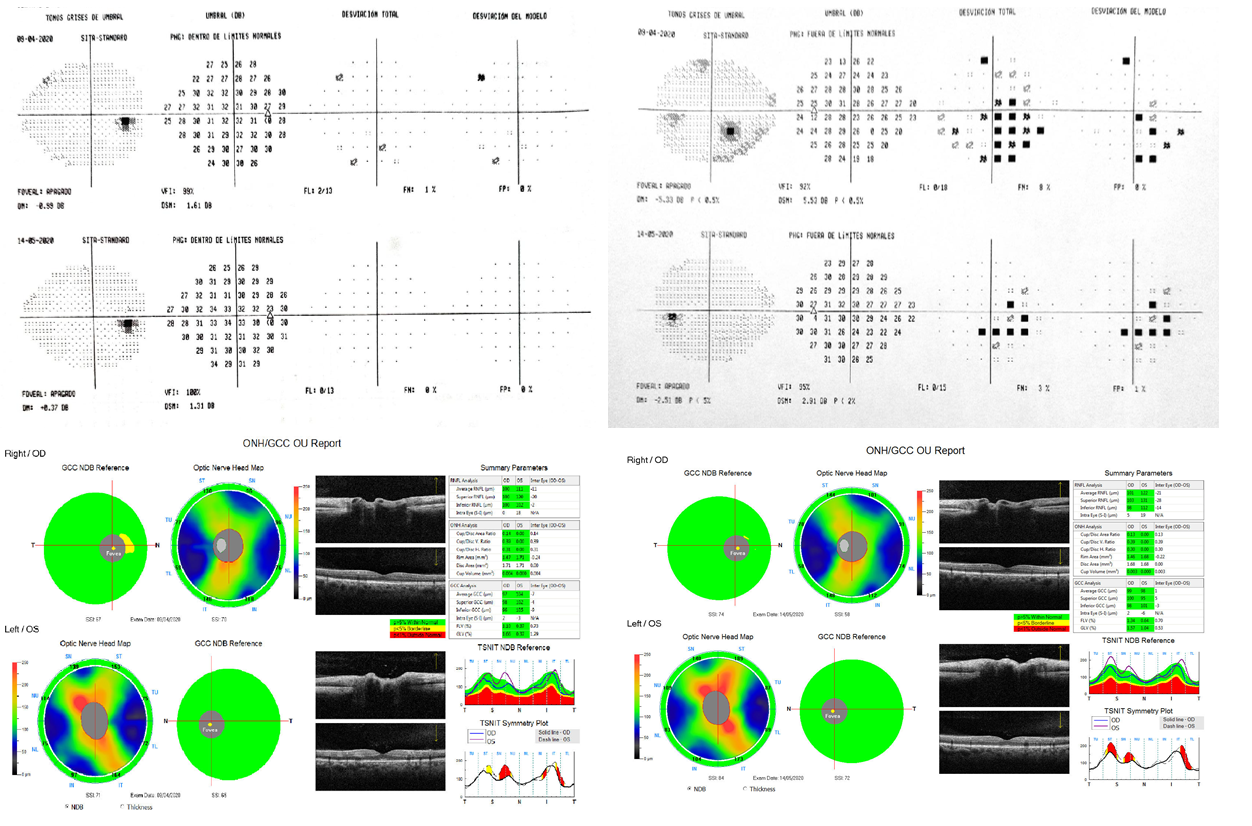
Figure 2 Computerized perimetry revealed a non-specific defect in OD and a centrocecal defect in OS.
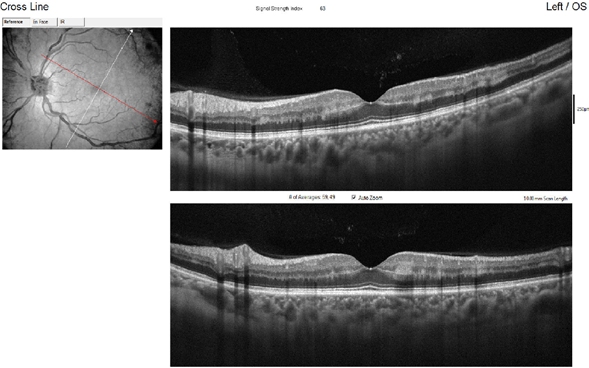
Figure 6 OCTA of the macula showed a decrease in vascular density in the deep superior and choriocapillaris layers.
At the follow-up, the patient reported that despite persistent visual symptoms, these did not significantly affect his visual field. Ophthalmic exams showed improvement in the visual field, with a more limited paracentral scotoma (Figure 7). Macular OCT showed fewer hyperreflective lesions in the temporal external plexiform layer, but worsening RNFL analysis due to increased optic nerve edema in OS secondary to NAION (Figure 8). OCTA indicated improved vascular perfusion in all retinal layers (Figure 9).
Ischemia of the optic nerve can occur in different anatomical regions. When it affects the anterior portion, it is classified as anterior ischemic optic neuropathy, which can be arteritic (AAION) or non-arteritic (NAION). Posterior involvement defines it as posterior ischemic optic neuropathy (PION). NAION has a multifactorial etiology, with risk factors including diabetes, hypertension, sleep apnea, toxic-metabolic disorders, nocturnal hypotension, and anatomical variations of the optic nerve. Its pathophysiology is not fully understood but is believed to involve circulatory deficits or infarction in the retrolaminar region of the optic nerve head and its collateral branches. Anatomical predispositions, such as a reduced optic nerve size or a small cup-to-disc ratio (<0.3), are also considered risk factors.1–3
The cause of the edema is also not fully understood, bearing similarities to a compartment syndrome caused by axonal swelling, which leads to apoptotic damage and a reduction in retinal ganglion nerve fibers. Clinical signs indicative of this condition include decreased visual acuity (which can vary across studies), altered pupillary reflexes (such as a relative afferent pupillary defect), visual field defects (mainly altitudinal and centrocecal), and impaired color vision, which is typically proportional to the level of visual acuity. Fundus examination often reveals hyperemic edema with splinter hemorrhages, and in some cases, soft exudates and a reduction or blurring of the cup-to-disc ratio (CDR) may also be present.
Although NAION is a clinical diagnosis, auxiliary tests help exclude secondary causes (e.g., hypercoagulability, cardiovascular, inflammatory, compressive, or demyelinating conditions). Neuroimaging is not first-line but can help rule out compressive or inflammatory causes. The management of NAION remains unclear, with conflicting evidence regarding antithrombotic measures, systemic steroids, and optic nerve decompression surgery.2,3
The prognosis is variable, but it is known that the condition can improve depending on protective factors such as age and good initial visual acuity. Generally, the condition stabilizes within 2 to 6 months. However, some studies report that recurrence in the affected eye can occur in 3 to 8% of cases, or that the other eye may become involved in 15 to 24% of cases within 5 years. Even though preventive measures can be taken, they do not necessarily have a positive effect in preventing involvement of the contralateral eye.3–5
Paracentral acute middle maculopathy (PAMM) was described as a variant of acute macular neuroretinopathy (AMN) by Sarraf et al., primarily suggesting an ischemic etiology based on imaging findings from spectral domain optical coherence tomography (SD-OCT). This allowed PAMM to be subdivided into two types: Type 1 PAMM, characterized by reflectivity changes in the inner nuclear layer, and Type 2 AMN, associated with reflectivity alterations in the outer plexiform layer, the latter being a much rarer or underdiagnosed entity. These lesions are associated with disruption and loss of the ellipsoid zone, leading to thinning of the outer nuclear layer. OCTA studies demonstrate that these findings are due to ischemia in the intermediate and deep retinal capillary plexuses in the affected regions. This also reveals the presence of an intermediate vascular layer in addition to the previously known superficial and deep layers, which had been difficult to study using traditional angiographic techniques.6–8
Although this phenomenon is a finding in both OCT and OCTA, it does have a pathological component primarily associated with ischemic etiologies in the retina, which may have either a local or systemic origin, such as venous or arterial obstructions in the retina, sickle cell retinopathy, diabetic retinopathy, hypertensive retinopathy, or antiphospholipid syndrome, among other conditions. The disease manifests with the appearance of a paracentral scotoma, associated with changes in visual quality (blurry vision) with or without affecting visual acuity, and it can involve one or both eyes. On fundus examination or retinal photography, pigmentary alterations may be found, or the findings can be mistaken for cotton wool spots in the macula, or no pathological findings may be present at all.9–11
Regarding disease progression, patients may experience variable degrees of improvement, or there may be a permanent deficit due to atrophy of the affected inner nuclear layer (INL). On autofluorescence imaging, parafoveal hypoautofluorescent lesions can be observed. In fluorescein angiography (FA), hypoperfusion lesions secondary to other pathologies may be detected, but FA does not provide significant diagnostic value for PAMM. OCT and OCTA remain the most effective imaging modalities for diagnosis and follow-up.12–15
Despite the recently acquired knowledge about PAMM, no specific treatment has been described for this condition, and therefore, the associated underlying pathologies are treated.16
This clinical case allows us to assess a previously unpublished association between NAION and PAMM, and how PAMM behaves during its structural and vascular evolution as measured by OCT and OCTA. Additionally, it highlights the importance and benefits of OCT and OCTA as part of the auxiliary studies for managing these pathologies. These imaging techniques allow us to analyze, quantify, and track structural changes in the optic nerve and macula, as well as vascular behavior, without exposing the patient to invasive tests that may carry adverse or allergic reactions. This is complemented by the use of functional studies to assess the patient's vision.
None.
The authors received no financial support for the research, authorship, and publication of this article.
The authors have no conflicts of interest to declare.

©2024 Espinoza, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.