Advances in
eISSN: 2377-4290


Research Article Volume 1 Issue 3
1Moorfields Eye Hospital, UK
2University College of London, UK
3Department of Ophthalmology, USA
4Department of Ophthalmology, Hawassa University, Ethiopia
5Department of Ophthalmology, Bnai Zion Medical Center, Israel
6ORBIS International, USA
7Department of Ophthalmology, Sheba Medical Center, Israel
Correspondence: Itay Ben-Zion, Department of Ophthalmology, Sheba Medical Center, Tel Hasomer, Israel, Tel 972-3-5302874
Received: October 06, 2014 | Published: November 21, 2014
Citation: Netzer OT, Moore DB, Eshete Z, et al. Outcomes of pediatric cataract surgery under local anaesthesia in a rural setting. Adv Ophthalmol Vis Syst.2014;1(3):75-78. DOI: 10.15406/aovs.2014.01.00017
Purpose: To compare the surgical outcome, visual acuity and complication rates among pediatric patients undergoing cataract surgery under local or general anesthesia in rural southern Ethiopia.
Methods: This retrospective study included pediatric patients younger than 15 years who underwent cataract surgery in rural southern Ethiopia during July 2007- August 2008. Local anesthesia was use in patients over the age of 7 years unless they suffered from traumatic or bilateral cataract. Clinical indices were collected before and following surgery, including uncorrected visual acuity categorized into ambulatory (better than hand motion) and non- ambulatory (hand motion or light perception) vision, intraocular pressure, cycloplegic refraction and ocular complications.
Results: Ninety-one eyes of 73 consecutive patients (57 male, 16 female) were included in the study. The average age at diagnosis was 7.1±0.5 years. Fifty-five operations were performed under general anesthesia (GA) and 36 using local anesthesia (LA). The percentage of patients with ambulatory UCVA improved significantly in both the GA (10.9% vs. 83.64%, p<0.0001) and LA groups (21.87% vs. 80.56%, <0.0001). No significant differences between the groups were noted regarding visual acuity results or complications.
Conclusion: Our results suggest that the outcomes of pediatric cataract surgery performed under either local or general anesthesia were comparable. LA should be considered a valid option for older children undergoing cataract surgery, especially when medical resources are limited.
Keywords: pediatric cataract; local anesthesia; general anesthesia; post-operative complications
GA, general anesthesia; IOL, intraocular lens; LA, local anesthesia; LP, light perception; SEM, standard error of the mean; UCVA, uncorrected visual acuity; VA, visual acuity; SEM, standard error of the mean
Cataract extraction the most common intraocular surgery performed in children. Advances in surgery instrumentation and technique have led to a reduction in complication rates, making cataract surgery a more accessible outpatient procedure.1,2 These changes have led cataract surgery to be available to children under more challenging conditions, such as those found in rural regions or developing countries. As most of the estimated 200,000 children who are blind from cataract are found in developing countries, making surgery more accessible in such regions is an important initiative.3,4 The accepted anesthetic method for pediatric cataract surgery is general anesthesia (GA), especially in younger children.5 This approach ensures a controlled environment during surgery and makes patient cooperation unnecessary. However, GA includes many potential risks and complications such as thermal regulation, cardiovascular events, respiratory events or death/brain death.6 Furthermore, in developing countries, lack of anesthesiologists leads to the employment of technicians as anesthesia providers, thereby increasing the potential danger to patients in cases of medical emergencies.7−9
Cataract surgery in adults is performed in most cases under local anesthesia (LA), by peri or retrobulbar injection, or topical anesthesia.10 This approach assists in rapid patient recovery with short or no hospitalization. Though this approach is not generally accepted when considering pediatric cataract surgery, there are recent reports of operations being performed under mild sedation with or without a local anesthetic.7−9 These studies showed that surgical outcomes were not different than those performed under GA. We have previously reported on the general surgical results of pediatric cataract extraction among a group of patients from rural Ethiopia.11 In this study we have focused on the relationship between the method of anesthesia and the surgical results. We retrospectively reviewed the results of cases operated under GA or LA, performed by a single surgeon (IBZ) in southern Ethiopia. We examined patients’ outcomes including visual acuity and complication rates.
A retrospective study was conducted of all consecutive pediatric patients younger than 15 years of age who underwent cataract surgery during a one year period between July 2007-August 2008 in rural southern Ethiopia. Patients were evaluated and treated at Hawassa University School of Medicine, a referral center for an estimated population of 15 million people; nearly half of the patients were children less than 15 years of age and were treated for various ophthalmic conditions. This work was part of the ORBIS international and Cyber-Sight project implementing pediatric ophthalmology services in Ethiopia. The study was approved by the Hawassa university institutional ethics review board. Prior to surgery, written informed consent was obtained for all patients by an accompanying guardian. All patients underwent a full clinical eye examination of the anterior and posterior segments and were diagnosed with cataract, based on standard clinical assessment and criteria. Younger children underwent evaluation under general anesthesia followed immediately by surgery, whereas older children (>7yrs) were given LA, and if they remained cooperative, surgery was performed. GA was performed by anesthesia technicians since the hospital was not staffed by anesthesiologists. All patients were under the age of 15 at the time of surgery and underwent at least 3 post op visits (days 1, 7, 30). Exclusion criteria for LA were age younger than 7years, penetrating trauma or bilateral cataracts. LA was administered by the treating surgeon (IBZ) by means of a peribulbar injection of 1-2ml Esracain 2% (Lidocaine hydrochloride 20mg/ml) to the orbital lumen at the infraorbital notch. At follow-up visits, patients underwent a comprehensive anterior and posterior eye examination, documentation of complications and uncorrected visual acuity (UCVA), measured or estimated depending on the patient’s age and level of cooperation, with the aid of a translator for the tribal language. To facilitate comparing UCVA results among children of different ages, verbal skills and cultural background, the UCVA results were divided into two main categories:11,12 (1) ambulatory, UCVA at this level included any better than hand motion vision (including the ability to follow an object, fixate and follow an object, finger counting or better); (2) non-ambulatory, VA is limited to hand motion or light perception. UCVA at the final follow-up was compared to that prior to surgery. Statistical analysis was performed using SPSS (version 21, IBM Inc., Illinois, USA). For quantitative variable analysis was performed using Student’s t-test. Categorical variables were evaluated using Pearson’s Chi square test. The accepted level of significance for all tests was α=0.05. Results are presented as means ± standard error of the mean (SEM).
Ninety one eyes of 73 consecutive patients (57 male, 16 female) were included in the study. Fifty-five eyes were operated under GA and 36 using LA. A single case of a girl younger than 4 years with congenital Rubella and significant cardiomyopathy was not eligible for GA and was therefore sedated using intramuscular ketamine. Average age at the time of operation was 7.1±0.5 years (range 0.5-15 years). GA patients were significantly younger than the LA group (4.87±0.49 vs. 10.14±0.56 years, p<0.0001, Student’s t-test, (Table 1). The majority of patients in both groups suffered from either developmental or traumatic cataracts (Table 1). No significant differences were noted in gender distribution, follow-up period, implantation of an IOL or the power of the implanted intraocular lens (IOL). In 85 eyes, small incision-capsular cataract extraction or cataract aspiration was performed, and in 6 eyes, because of lens dislocation, an intra-capsular cataract extraction was performed. IOLs were implanted in 61 eyes (60 posterior chamber IOLs and 1 anterior chamber IOL; average power 23 diopters, range 17-27diopter).
GA |
LA |
p value |
|
# of eyes |
55 |
36 |
|
Males (%) |
69.1 |
69.4 |
0.97 |
Age (yrs) |
4.87±0.49 |
10.14±0.56 |
<0.0001 |
IOL (%) |
54.6 |
86.1 |
0.16 |
IOL power (diopter) |
23±0.3 |
22+0.3 |
0.2 |
Follow-up (months) |
7.93±0.43 |
7.06±0.45 |
0.18 |
Cataract type (%) |
|||
Developmental |
25.45 |
52.78 |
|
Traumatic |
65.45 |
47.22 |
|
Congenital Rubella |
3.64 |
0 |
|
Glaucoma |
5.45 |
0 |
Table 1 Pre-operative patient characteristic
Baseline characteristics did not differ between the two groups apart for age at time of operation
GA, general anesthesia; LA, local anesthesia; IOL, intraocular lens
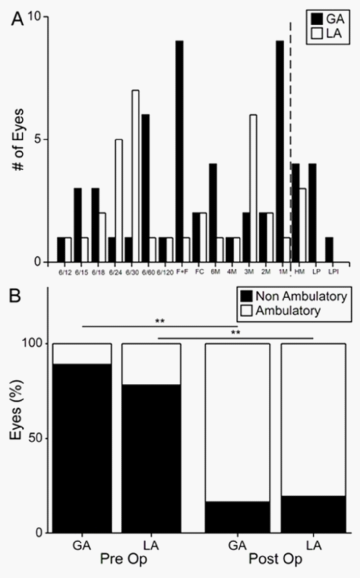
At presentation, UCVA ranged from 6/60 to light perception (LP), with 13 eyes (14.29%) having ambulatory vision (better than hand motion). Average follow-up time was 7.8±0.4 months (range 2-13 months) and all patients attended at least three follow-up examinations (day 1, 1 week and 1 month post operation). The average post-surgical UCVA was significantly improved, ranging from LP to 6/9 (Figure 1A). The percentage of patients with ambulatory UCVA improved significantly following surgery in both the GA (10.9% vs. 83.64%, p<0.0001, Pearson’s Chi square) and LA groups (21.87% vs. 80.56%, <0.0001, Pearson’s Chi square, Figure 1B). No significant differences were noted between the two anesthesia groups. Table 2 describes the post-operative complications for the entire population group, no difference was noted in the complication rate between the GA and LA groups (9.09% vs. 11.11%, respectively). No cases of retinal detachment or endophthalmitis were noted during the follow-up period. Based on our experience, a child that underwent a successful peribulbar/retrobulbar injection also withstood the surgery and was steady and compliant. In all of our patients there was not a single case that required a conversion from LA to GA. We have also noted that tribal rural children were more compliant and willing to undergo an LA trial and surgery compared to urban children (data not shown).
GA (n) |
LA (n) |
|
IOL dislocation |
1 |
0 |
Visual axis opacities |
1 |
1 |
Transient increased IOP |
2 |
1 |
Choroidal effusion |
1 |
1 |
Post-operative anterior uveitis |
0 |
1 |
Table 2 Post-operative complications
There was no significant difference in the rate of complications between the two groups
GA, general anesthesia; LA, local anesthesia; IOP, intraocular pressure
In the current study, we examined the outcome and complications rates among pediatric patients that underwent cataract surgery by GA or LA. We found that (1) following cataract surgery, ambulatory vision improved significantly in all patients, especially if an IOL was implanted (2) there was no significant postoperative difference in UCVA based on the anesthetic approach (3) cataract surgery was well tolerated by patients regardless of anesthesia technique (4) the rate and type of peri and postoperative complications was similar among the two groups. In the developing world and especially in rural areas where the availability of medical care is limited, identifying and treating perinatal pathologies may be extremely delayed. In these regions, blind children are less likely to survive and many cases may never reach medical attention. Through surgical intervention we are able to offer such children the chance to be independent of constant supervision and assistance. Even moderate improvement in VA may have a profound effect on their survival and is possibly more important than achieving the best possible VA. Although the general aim is to perform cataract surgery as early as possible to minimize amblyopia and visual impairment,13 this is not always possible in these regions.14 Even so, following cataract surgery, especially if an IOL is implanted, VA may increase significantly, reducing the socioeconomic burden of such children and increasing their own chance of survival.15 Among our patients, we found that the percentage of patients with ambulatory VA increased from 14.29% to 82.42% (91.8% among IOL implanted eyes) and that the choice of anesthesia had no relation to the surgical outcome or the final VA these children achieved.
The use of LA for pediatric cataract is not considered general practice in developed countries. Concerns regarding patient cooperation and the potential for surgical complications have led to the use of GA for most pediatric surgery.5 The availability of qualified anesthesiologists, modern equipment and relatively safe anesthesia techniques has also supported the use of GA. In our study, we found that the complications rates following cataract surgery were not different between the two groups. We noted that although LA was used for older children, patient selection resulted in full cooperation with no intra-operative incidents. This reflects the relative safety of using LA in such settings and suggests LA may be a viable choice for pediatric surgery, especially under conditions where GA cannot be administered by qualified physicians or monitoring equipment is insufficient.7,8,16 It should be noted, that cultural and social differences may affect how a child behaves under such circumstances, and not all children will respond to LA in a similar manner. Careful patient selection is essential in minimizing the anesthesia risks and achieving a good surgical result.
There are several limitations for this study, mainly due to its retrospective nature. As anesthesia choice was based primarily on child age, this represents a selection bias, as the two groups differed in age. However, the mean age for patients given LA was still around 10, representing a significant pediatric population. The good visual outcome results as well as low complications rates in this group support approach that with careful patient selection LA may be considered for pediatric cataract surgery. Other limitations include limited follow-up, as well as the fact that all cases were gathered from a single site. Therefore, we must regard these results with some caution as they may only apply to similar rural settings. These findings may not be appropriate in settings where GA is performed under more controlled conditions. Future studies are needed to evaluate whether LA may be suitable for pediatric cataract surgery in such cases.
Our study suggests LA should be regarded as a valid option in cases of older children when GA may be unnecessary or medical conditions preclude the safe use of general analgesics, with post-operative results that are comparative to surgery under GA. This is especially relevant to rural areas in the developing world and sub Saharan Africa in particular as many hospitals have few qualified anesthesiologists (not to mention pediatric anesthesiologists) and depend on anesthesia technicians to deliver GA, usually with only modest monitoring capabilities.
The authors wish to thank Prof. Eugene E. Helveston for his immense support and guidance throughout this study. The authors have no financial or proprietary interests to report.
Author declares that there is no conflict of interest.

©2014 Netzer, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.