Advances in
eISSN: 2377-4290


Case Series Volume 7 Issue 2
Ophthalmology Department, Menoufia University, Egypt
Correspondence: Mohamed Samy Abd Elaziz, Department of Ophthalmology, Faculty of Medicine, Menoufia University, Egypt, Tel +201003876617
Received: June 16, 2017 | Published: July 19, 2017
Citation: Zaky AG, Elaziz MSA, Elmazar HMF, Nassar MK (2017) Our Experience with Orbital Vascular Disorders in Menoufia University Hospital, Egypt. Adv Ophthalmol Vis Syst 7(2): 00217 DOI: 10.15406/aovs.2017.07.00217
Objective: To study the common presenting features, possible management options, and outcome results in a series of patients with intraorbital and extraorbital vascular disorders.
Background: Vascular lesions constitute up to 10-15% of all orbital tumors. The shape, color, and invasiveness differ within each group: from bright red to deep blue and from a well-demarcated lesion to a more infiltrative tumor within the surrounding orbital tissue. Intraorbital vascular lesions can be categorized into arteriovenous, venous, and lymphatic disorders, each category have different clinical presentation, imaging characteristics, and management strategy.
Patients and methods: A retrospective non comparative case series study was conducted at ophthalmology department, Menoufia University Hospital, Egypt. Records of 10 patients diagnosed with orbital vascular disorders in the period from January 1, 2014, to August 31, 2016 were reviewed as regard to their diagnostic and therapeutic findings.
Results: Data of ten patients with unilateral vascular disorders were reviewed; the cohort included 4 women and 6 men with a mean age of 45 years (range, 5-66 years). Presenting findings included periocular mass (8 patients, 80%); periocular edema (6 patients, 60%); pulsation/bruit (3 patients, 30%); proptosis (5 patients, 50%); previous trauma (5 patients, 50%); elevated intraocular pressure (4 patients, 40%); pain and reduced visual acuity (2 patients each, 20%); and restriction of extraocular movements, and diplopia (1 patient, 10%). Orbital ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), and computed angiography revealed specific findings according to type of vascular disorders. Treatment options ranged from conservative follow up till surgical excision. Two patients received embolization of feeder vessels; most of the patients had initial resolution of manifestations after treatment.
Conclusion: Orbital vascular disorders can present with different symptoms and signs. Their diagnosis necessitates integrated cooperation between ophthalmological, interventional radiology, and vascular subspecialties. Computed tomography, magnetic resonance imaging and angiography are essential for both diagnosis and management. The treatment depends on patient-specific features and includes observation, embolization, and surgical excision or combined preoperative embolization/excision.
Keywords: orbital vascular disorders, angiography, orbital embolization
Vascular anomalies are classified into vascular tumors and vascular malformations based on the classification system of the International Society for the Study of Vascular Anomalies (ISSVA). Vascular tumors are characterized by proliferation and tumor enlargement, and the most common vascular tumor is infantile hemangioma, while a less common vascular tumor is hemangiopericytoma. Vascular malformations consist of non-proliferating vascular lesions in which blood flow is misdirected through anomalous channels. Malformations exist on a spectrum, ranging from high-flow arteriovenous malformation (AVM), low-flow venous (varix) and lymphovenous malformations, and capillary-venous malformations. Flow characteristics affect the natural history of vascular anomalies and are helpful in making the correct diagnosis.1,2 Patients with orbital vascular disorders seek medical advice for many reasons. Among these, exophthalmos, pain, and diplopia are most common. Patients presenting with these symptoms must undergo a comprehensive ophthalmic history and examination in order to document the type of the tumor and determine its clinical impact.3–5
Careful history taking is one of the most important tools available to the ophthalmologist. Main complaint usually includes periocular or retro-orbital pain, persistent or temporary visual loss, double vision or disfigurement. Appearance on initial examination is variable, as although the lesions are often congenital, they may not cause symptoms in childhood. Stimuli for growth include menarche, pregnancy, and trauma. Common findings include periocular pain, dilated corkscrew vessels on the globe extending to the limbus, proptosis, pulsation, bruit, and raised intraocular pressure.6 Important ancillary tests include ultrasonography, computed tomography (CT), magnetic resonance imaging (MRI), CT angiogram and MR angiogram. Each of the three major orbital vascular malformations has its own pathognomonic characteristics.7 Management of orbital disorders may be difficult due to the risk of hemorrhage, vascular occlusion during treatment. The most critical concern is protection of the optic nerve and visual acuity, followed by preservation of periocular functions such as eyeball and eyelid movements.
This is a retrospective non comparative case series study for all patients diagnosed with orbital vascular disorders at ophthalmology department, Menoufia university hospital, Egypt from January 1, 2014, to August 31, 2016. The study was designed according to the principles outlined in the Declaration of Helsinki and after obtaining the approval of the institutional review board at the Department of Ophthalmology, Menoufia University, Egypt, also a written consent for surgery, photography, and to be included in the study was obtained from all cases. Medical records were reviewed as regard to: age; sex; duration of symptoms and signs; clinical presentation; site involved; imaging findings on ultrasonography, angiography, computed tomography, or magnetic resonance imaging angiography were reviewed (Figure 1A-1F); treatment modalities; and outcomes. Response to treatment was evaluated by resolution of the signs and symptoms noted at the initial examination and patient satisfaction.
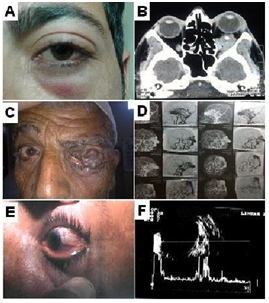
Figure 1 (A) Patient no. 2 with LT lower lid congestion, (B) CT show orbital varix in posterior orbit with phlebolith, (C) patient no. 5 with giant vascular malformation in left eye, (D) angiography identify feeder vessels from ophthalmic artery, (E) patient no. 10 with low flow fistulae that mimic chronic conjunctivitis, (F) orbital ultrasound showing dilated superior ophthalmic vein of patient with low flow arteriovenous malformations.
This study included 10 patients (4 women and 6 men) with a mean age of 45 years (range, 5-66 years). All of the cases were unilateral. The mean duration from initial clinical signs and symptoms to diagnosis and treatment was 10 years (median, 8 years; range, 6 months to 20 years). The presenting signs and symptoms are summarized in Table 1. The most common finding was periocular mass (8 patients, 80%) and periocular edema (6 patients, 60%). Computed tomography or magnetic resonance imaging localized the lesions to the superomedial quadrant of the orbit in 2 patients, the superolateral quadrant in 2 patients, posterior orbit in 1 patient and intracranial in 1 patient.
Manifestations |
Number (%) |
Periocular mass |
8 (80) |
Periocular swelling |
6 (60) |
Pulsation/bruit |
3 (30) |
Proptosis |
6 (60) |
Previous trauma |
5 (50) |
Elevated intraocular pressure |
4 (40) |
Pain |
2 (20) |
Reduced visual acuity |
2 (20) |
Restriction of extraocular movements, and diplopia |
1 (10) |
Table 1 Initial Clinical Signs and Symptoms in 10 Patients with Orbital vascular Malformations
We encountered 3 cases of indirect carotid cavernous fistula whose visual acuity was good, pupillary reaction was normal in both eyes. Difference in exophthalmometric readings between both eyes was 2-3 mm. Ocular motility was normal in both eyes. No bruits were noted on auscultation and the proptosis was not accentuated by Valsalva maneuver. Ophthalmologic examination of the affected eye revealed dilatation of conjunctival vessels especially in the inferior fornices and chemosis. Ophthalmoscopy was unremarkable. Neurologic examination revealed no deficits. Brain computed tomography (CT) was normal, multiplanar MRI revealed ectatic & dilated left superior ophthalmic veins. After few months, 2 cases showed raised IOP=30-40 mm Hg (even uncontrolled by antiglaucoma eye drops). Angiography revealed an indirect carotid cavernous fistula, feeder vessels from meningeal branches of both internal & external carotid arteries.
Embolization of feeder vessels by embolic agent 6% ethylene vinyl alcohol copolymer, soluted in dimethyl-sulfoxide (onyx18) was performed in 2 patients. One month after embolization, there was improvement of symptoms, manifestations and IOP was less than 24 mmHg without any treatment. Feeder vessels were ligated in another patient, with careful excision of the malformations ensuring hemostasis but failed. Histologic analysis in cases that underwent surgical debulking revealed lesions with thickened arterial and venous components, consistent with AVMs. Seven cases needed surgical interferences as shown in Table 2 which were aspiration, embolization, surgical excision/debulking or combined embolization and debulking. After which, substantial symptomatic improvement was noted regarding proptosis, raised intraocular pressure, reduced visual acuity, and periocular swelling in most of the patients. Pain was persistent in 2 patients (20%), with 1 requiring further surgical intervention. Diplopia was reported in 1 patient (10%) postoperatively, which required strabismus surgery to attain binocular vision. Patients' demographics and management are outlined in Table 2.
Patient |
Duration of symptoms |
symptoms |
Side |
Ultrasound |
Treatment |
Progress |
Comments |
1/M/27 |
7 y |
Periocular mass, slowly |
R |
AVM anterior |
Refused treatment |
Lost to follow- |
Boxing trauma to left side |
2/M/26 |
5 y |
Periocular mass, |
L |
CT show varices |
Conservative treatment & Follow up |
Remission & |
Idiopathic |
3/F/53 |
1.5 y |
Pain, eyelid lesion, and bulbar conjunctival hyperaemia (Figure 2) |
L |
Indirect carotid |
Embolization by onyx 18 |
Resolution of |
Hypertensive & menopause |
4/F/43 |
27 y |
Both upper & lower lid, Episcleral mass and |
R |
CT show no |
Surgical debulking |
Incomplete |
Idiopathic |
5/M/62 |
10 y |
Periocular mass, pulsation, episcleral congestion and reduced VA (Figure 1C) |
L |
giant AVM filling |
Ligation of the left superficial |
Failed surgery |
None |
6/M/6 |
3 months |
Sudden painful proptosis |
R |
Isolated orbital |
Drainage of the chocolate cyst by maxillofacial surgeon |
Resolution of |
None |
7/M/32 |
10 y |
Periocular mass and swelling, 5-mm proptosis, decreased VA, increased IOP, |
R |
AVM anterior |
Preoperative |
Resolution of |
None |
8/F/9 |
2 y |
Several soft bluish masses in upper nasal quadrant of epibulbar surface not increase in size with valsalva (anterior lymphangioma) |
R |
No posterior lesion |
Surgical debulking |
Recurrence; |
Upper respiratory tract infection |
9/F/70 |
3 months |
Periocular mass, |
R |
AVM anterior |
Surgical excision |
Resolution of |
None |
10/M/53 |
2 Y |
Mild proptosis, periocular edema & congestion (Figure 1E) |
L |
Dilated superior |
No treatment |
Spontaneous |
None |
Table 2 Patient Demographics, Diagnosis and Management of Orbital vascular disorders
A 53 year-old female patient presented with a one-year history of left sided headache, pain, redness and congestive symptoms together with protrusion of her left eye. She had no history of orbital trauma or family history of vascular disorders. Visual acuity was 20/20 and 20/30 in right and left eyes, respectively. Pupillary reaction was normal in both eyes. Exophthalmometric readings were 20 mm in the right and 22 mm in the left eye. Ocular motility was normal in both eyes. No bruits were noted on auscultation and the proptosis was not accentuated by Valsalva maneuver. Ophthalmologic examination of the affected eye revealed dilatation of conjunctival vessels especially in the inferior fornices and chemosis (Figure 2A). Ophthalmoscopy was unremarkable. Neurologic examination revealed no deficits. Brain computed tomography (CT) was normal, multiplanar MRI revealed ectatic & dilated left superior ophthalmic veins (Figure 2B). After 2 months, she experienced worsening of symptoms & manifestations IOP = 30-40 mm Hg (even uncontrolled by antiglaucoma eye drops). Angiography revealed a left indirect carotid cavernous fistula, feeder vessels from meningeal branches of both left internal & external carotid arteries (Figure 2C). Endovascular treatment of left dural CCF by embolization using Onyx 18 was done. One month after embolization, there was improvement of symptoms, manifestations and IOP was 23 mmHg without any treatment (Figure 2D).
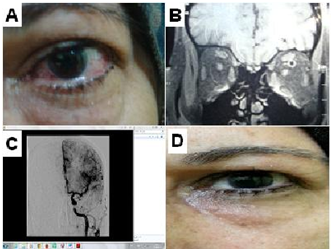
Figure 2 Patient no. 3 (A) dilatation of left conjunctival blood vessels, chemosis and lid puffiness, (B) coronal MRI show dilated left superior ophthalmic vein, (C) external carotid angiography demonstrated left cavernous sinus filling during early arterial phase, and (D) patient 1 month after embolization by onyx 18.
Management of Orbital Vascular disorders is a real challenge. As regard AVMs, they are congenital lesions with numerous large feeding arteries, a central nidus and numerous dilated draining veins. AVMs may pulsate and have associated bruits on auscultation. They have a number of larger arterial feeding vessels on angiography and are histologically composed of abnormal dysplastic vessels. Intraorbital AVMs are rare lesions.8 Wright9 reported only 3 cases of arteriovenous shunts among 627 patients with various orbital diseases. In this study, we reported 5 cases with orbital AVMs, 2 cases were high flow shunts and 3 cases were low flow. Intraorbital AVMs are most often related to an intracranial or maxillofacial arteriovenous shunts [8]. Management of intraorbital AVMs may be difficult due to the risk of hemorrhage, vascular occlusion during treatment, and collateral damage to surrounding organs.8
Identification of all arterial feeders from both internal and external carotid systems is critical in developing a therapeutic plan. AVMs may be treated by surgical excision or embolization alone. However, in the hands of an experienced interventional neuroradiologist and surgical team, most AVMs may be treated by a combined approach of preoperative embolization followed by surgical excision of the vascular mass. The goal of therapy is closure of the low-resistance shunt. In our cases, the AV disorders had different feeders' vessels; from the external carotid system, the internal carotid system or ophthalmic artery. Embolization of the external carotid system feeder vessel was performed and seems to be easier, but intervention through the ophthalmic artery was not possible without iatrogenic risks.
Chakrabortty et al.10 reported complete removal of the intraorbital contents after unsuccessful endovascular and surgical treatment of AVM. In our cases, the AVM had two major feeders' vessels, the larger from the external carotid system and the other from the internal carotid system and ophthalmic artery. Kim & Kosmorsky11 reported a case of arteriovenous communication between branches of the internal and external carotid systems and the ophthalmic veins located within the orbit. Embolization therapy of the lesion resulted in a branch retinal artery occlusion. This shows the complications that may result from management of such cases and how much these cases are rare and difficult in management. The therapeutic options are very limited in cases of AVM in the posterior orbit, particularly when the dura of the optic nerve is involved.12 In our cases, because of the posterior extension of the lesion (Figure 2), it was not possible to remove the nidus surgically and debulking was limited to the anterior vascular loops. Significant decrease in symptoms, chemosis and exophthalmos in our patients after embolization of the feeding artery suggests that this method is useful for similar cases and may be considered as an appropriate treatment option for intraorbital AVMs.
Rootman et al.13 described their clinical and radiologic experience with orbital vascular malformations using the International Society for the Study of Vascular Anomalies (ISSVA) classification and the preferred radiologic techniques. They concluded that evolving and future treatment strategies for orbital lesions should be based on a better understanding of the pathophysiology and use of a common classification. The standard of care and reporting should include dynamic assessment before, during, and after therapy. There are possibilities for new glue agents, sclerosants, or gels that could be left in the lesions, thereby curing them via minimally invasive image-guided methods. Also, as noted, serial injection of newer sclerosants may be useful in ablating and controlling progression of the lesions and may be combined with surgical interventions with and without gluing techniques. In this study we recorded 2 cases with orbital varices, one in the posterior orbit which is followed up without any interference while the other is at anterior orbit and underwent surgical debulking.
In our study, 2 cases of lymphangioma were recorded. One of them complicated by chocolate cyst and was aspirated by maxillofacial surgeon, the other one was excised by us. The diagnosis can be aided by clinical history and noninvasive tests, such as flow Doppler studies, and by computed tomography and magnetic resonance imaging to highlight the extent of the lesions. Diagnosis of orbital AVMs is based on angiographic findings highlighting an engorged, rapidly filling proximal arterial system, a malformation, and distal venous outflow.8 In our case series, CT was helpful in detecting calcification (phleboliths) of orbital vairx while MRI was more diagnostic in cases of AVMs. Although, angiography is an invasive technique, it's very important when decision of surgery or sclerotherapy is taken to localize the feeder vessels. This agrees with Warrier et al.14 who record 8 cases of orbital AVMs. The risk-benefit ratio must be evaluated on a case-by case basis before interventional management is undertaken in orbital vascular disorders. Their natural history must be understood and considered, alongside the risks of neuroradiologic and surgical interventions. Visual compromise and persistent or progressive patient discomfort are the main indicators for intervention.
Orbital Vascular disorders form a major multidisciplinary problem that needs comprehensive understanding of many anatomical and pathological aspects. Computed tomography, magnetic resonance imaging and angiography are essential for diagnosis and for planning the management of different orbital vascular lesions. The management of these cases necessitates integration between ophthalmological, radiological and vascular subspecialties, this cooperation should continue throughout the management process in order to achieve the best results.
None.
The authors declare no conflicts of interest.

©2017 Zaky, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.