Advances in
eISSN: 2377-4290


Case Report Volume 3 Issue 2
DrishtiCONE eye care, India
Correspondence: Rajat Jain, DrishtiCONE eye care, Shalimar Bagh, Delhi-110088, India, Tel +91 8585977709
Received: October 27, 2015 | Published: November 4, 2015
Citation: Jain R, Mohan N. Nylon allergy after keratoplasty–fiery sun. Adv Ophthalmol Vis Syst. 2015;3(2):257-259. DOI: 10.15406/aovs.2015.03.00080
Purpose: To report a case of allergy to the nylon suture material after keratoplasty and its clinical implications
Design: Case Report
Observation: Seventy-three year old man underwent penetrating keratoplasty for pseudophakic corneal edema. Post-operatively he had profuse watering, photophobia, lid margin swelling, conjunctival ballooning and corneal edema. Persistent anterior segment and ocular surface inflammation lead to extensive suture track vascularisation giving a ‘fiery sun appearance’. Loose sutures required early suture removal by 2 months. Subsequently, anterior segment and ocular surface inflammation decreased. Systemic/topical corticosteroids were tapered. Retrospective diagnosis of allergy to suture material was made.
Results and discussion: At 6 months follow-up, patient has BCVA 6/24, normal ocular surface, no intra-ocular inflammation and normal optic disc. This is first report of presumed nylon allergy after keratoplasty. Specific problems like uncontrolled cylinder power, unstable graft-host junction and wound over-ride due to early suture removal were encountered.
Keywords:keratoplasty, pseudophakic corneal edema, inflammation, conjunctival ballooning, lid margin swelling, retrospective diagnosis
ACIOL, anterior chamber intra-ocular lens implantation; PKP, penetrating keratoplasty; DSEK, descemet’s stripping endothelial keratoplasty; ECCE, extra capsular cataract extraction
Nylon has been the most preferred suture material for penetrating keratoplasty. Toxic allergic reaction to nylon has been reported after cataract,1,2 and vitrectomy surgery.3 We report a case of nylon allergy in a patient of penetrating keratoplasty. The consequences of such an adversity are more deterrent than those after cataract surgery. To the best of our knowledge, this is the first such case reported.
A 73 year old, non-diabetic, non-hypertensive gentleman presented with watering, photophobia and painless diminution of vision in the right eye for the past 6months. Previously, he had undergone a surgery for cataract removal 15years ago and subsequent anterior chamber intra-ocular lens implantation (ACIOL) 8years ago. As per history, he could see well after the surgery till recently when the vision had dropped. He was also on three anti-glaucoma medications in both eyes for the past 12months.
At presentation, he had a best corrected visual acuity of 5/60 in right eye (OD) and 6/18 in left eye (OS). On examination, the right eye showed conjunctival hyperaemia, corneal edema, anterior chamber was quiet with presence of ACIOL which was anteriorly tilted, pupil was irregular in shape and peaking temporally where a condensed vitreous strand was attached to the corneo-scleral wound and was pulling the ACIOL towards the cornea. Figure 1A Left eye showed presence of corneal guttae and cataract. Fundus view was hazy in right eye and normal in the left eye. A pre-operative B scan ultrasound performed for the right eye was normal. Applanation intra-ocular pressure was 21 (OD) and 13 (OS) mm Hg. Based on the above a clinical diagnosis of OD pseudophakic corneal edema with ACIOL with a vitreous tag and OS Corneal Guttae and Cataract, presumed Fuchs Endothelial Dystrophy, was made. He was advised specular microscopy which showed unclear images in the right eye and profuse guttae in the left eye so much so that the endothelial count was not ascertainable. He was advised penetrating keratoplasty (PKP) with anterior vitrectomy with/without IOL exchange in the right eye. The left eye was kept under a close watch with potential cataract surgery with Descemet’s stripping endothelial keratoplasty (DSEK) later.
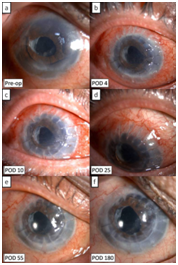
Figure 1 Composite image showing varying clinical stages of the case. (A) Pre-operative image showing mild corneal edema, anterior chamber intra-ocular lens with a vitreous tag going upto the corneal wound; Post-operative images at day 4. (B) and day 10 (C) showing lid edema and ocular surface inflammation. (D) Increased ocular surface inflammation, conjunctival hyperaemia and radiating suture tract vascularisation giving a ‘fiery sun appearance’ at day 25. (E) Stabilised ocular surface, decreased conjunctival injection and corneal scarring along the suture lines at post-op day 55. (F) Stable ocular surface and cornea at post-op day 180.
The right eye surgery was performed as planned. Intra-operatively, a 7.75mm corneal trephination was performed. The vitreous tag was cut with a vitrector. The IOL was found to be smaller, mobile and unstable. It was hence replaced with a 13mm diameter ACIOL. An 8.25mm optical quality corneal tissue was transplanted using 16 interrupted 10-0 nylon monofilament sutures. The surgery was uneventful. The eye was patched.
Post-operatively the patient was prescribed oral analgesic on as and when required basis. The patch was removed the next day and the patient was prescribed moxifloxacin 0.5% eye drops 6 times a day, prednisolone 1% eye drops 6 times a day and homatropine 2% eye drops 2 times a day as done routinely for other penetrating keratoplasty surgeries. On the next visit, fourth day post-operatively, the patient presented with profuse watering and photophobia in the right eye and showed lid margin swelling, increased conjunctival hyperaemia and conjunctival ballooning. Figure 1B the dosage of topical steroids was increased to everyone hourly and oral corticosteroids 1 mg/kg body weight was started. The patient was then seen on post-operative day 10 and showed gradual increase in all the symptoms and signs. Besides, fine superficial vascularisation started to appear at the suture line in all sutures. Figure 1C Topical and systemic corticosteroids were continued in the same dosage, besides other treatment. On post-op day 25, the patient had severe ocular discomfort, profuse watering and photophobia. Conjunctival hyperaemia and chemosis had significantly increased. Cornea showed minimal corneal edema and significant vascularisation along the suture-line. Figure 1D one suture at 12 o’clock had become loose and was removed. Ocular symptoms and signs were persistent despite maximum corticosteroid treatment. The side-effect of the persistent ocular surface inflammation was that 15/16 sutures needed removal within 2 months of surgery.
Figure 1E gradually the ocular surface stabilized, symptoms significantly decreased and the patient became comfortable. Ocular surface and anterior segment inflammation decreased over the next 1month after suture removal. The suture-line showed scarring as a reminiscent of the vascularisation. Topical and systemic corticosteroids were tapered and moxifloxacin eye drops were stopped. At 6months follow-up, patient has best spectacle corrected visual acuity as 6/24, best contact lens corrected visual acuity as 6/18, a normal ocular surface, no intra-ocular inflammation and normal optic disc. Figure 1F corneal topography shows a steep cornea with 14.6D cylinder (Figure 2) possibly due to irregular wound healing and wound gape at 4 o clock. He is currently on topical prednisolone 1% 4 times a day and carboxy-methyl-cellulose 0.5% eye drops 4 times a day.
We hereby report a case of an elderly gentleman who underwent penetrating keratoplasty for pseudophakic bullous keratopathy. The pre-surgical diagnosis, surgical planning and the intra-operative events were no different than a routine PKP.4 However the patient unexpectedly showed marked ocular surface inflammation despite topical and systemic steroids post-operatively. The inflammation was relentless and it leads to suture tract vascularisation and consequent loose sutures much early than desired. Suture track proliferation was florid and was seen in all 16 sutures in our patient. This radial suture tracks appeared to be in the form of the rays of the sun and hence we call it a ‘fiery red’ appearance. Loose sutures needed early removal with its potential complications. The inflammation stabilized after suture removal and eventually decreased. A retrospective diagnosis of allergy to the suture material was made. Though cases of allergy to suture material after cataract and vitrectomy surgery have been reported earlier,1–3 this is the first such case to be reported in literature after PKP.
As specified, cases of nylon allergy after cataract and vitrectomy surgery have been reported earlier. Balyeat et al reported foreign body sensation, conjunctival injection, localized scleral infiltrates and scleral excavation underlying the running 10-0 nylon suture in 10/105 consecutive patients (9.5%) who underwent uncomplicated planned extra capsular cataract extraction (ECCE).1 Similarly Elosúa de Juan I et al.,2 reported local inflammatory reaction at the incision site after routine ECCE. Schechter RJ,3 reported a case after pars plana vitrectomy. However, all the above cases had scleral wounds and the wounds were significantly smaller in dimension to that seen after a PKP. Increased inflammatory reaction after cataract (ECCE) or vitrectomy led to early vascularisation and a better healing. However, the present case had a 360o corneal wound and the suture vascularisation which required early removal was unwarranted before the graft-host unction had stabilized and healed. This led to an unstable cylinder power which could not be controlled with selective suture removal. There also developed an area of graft override. These complications after a routine keratoplasty were undesired.
Kyrillos et al performed Boston Keratoprosthesis type 1 (KPro) surgery for a patient of aniridia. The patient had earlier undergone a glaucoma surgeries and showed foreign-body sensation, conjunctival hyperemia and edema in the early postoperative period. The symptoms had subsided after suture removal then. Hence they used proline suture in their case for Kpro surgery with no complications and a good stability.5 Hence proline could serve as a viable replacement for our case in future for any surgical intervention if needed in this or the contralateral eye.
To conclude, allergy to the suture material though uncommon is reported. The consequences of such a problem are far more undesirable when the wound is corneal or larger as seen after a PKP than after a cataract surgery which involves a smaller wound and is usually in the periphery.
None.
The author declares there is no conflict of interest.
None

©2015 Jain, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.