Advances in
eISSN: 2377-4290


Research Article Volume 13 Issue 1
1Department of Ophthalmology, Chivasso City Hospital, Turin, Italy
2Department of Surgical Sciences, Eye Clinic, University of Cagliari, Cagliari, Italy
Correspondence: Giuseppe Vadalà, Head of Department of Ophthalmology, Chivasso Hospital (Turin, I), Italy
Received: February 15, 2023 | Published: March 13, 2023
Citation: Vadala G, Siotto-Pintor E. Intradermal suture post-surgical scar in external dacryocystorhinostomy: technique and patient satisfaction survey. Adv Ophthalmol Vis Syst. 2023;13(1):35-39. DOI: 10.15406/aovs.2023.13.00436
Purpose: Dacryocystorhinostomy surgery may result in significant postoperative scarring. Although other surgical techniques have been developed that achieve a better aesthetic result, the ab externo technique remains the gold standard for this procedure. We developed a telephone survey to evaluate the visual impact of postoperative skin scars associated with ab externo dacryocystorhinostomy.
Methods: 470 patients underwent uncomplicated external dacryocystorhinostomy surgery by two consultant surgeons from January 2014 to December 2021. Skin incisions were closed using intradermic continuous suture with prolene 6.0. The exclusion criteria were cases of dacryo-phlegmon and lacrimal sac fistulae with skin maceration. The visual effect of the postoperative scar was evaluated, and the degree of patient satisfaction was measured by a questionnaire with four subjective perceptions of the scar (very good, good, bad, very bad) given by a physician in the first postoperative month. The survey responses were used as the basis for a literature review.
Results: The survey received 470 responses (100%) Very good perception of the scar was achieved in 75,8% of patients. There were no other post-operative complications noted from medical records review.
Conclusions: Given the small percentage of patients who complained of marked scarring, it should not be the main reason for deciding on the procedure for dacryocystorhinostomy, especially in elderly patients.
Therefore, the surgical technique should be considered as a surgically acceptable choice if cosmetic results were selection criteria in the case of total stenosis of the nasolacrimal duct.
Keywords: external dacryocystorhinostomy, DCR, scar, lacrimal surgery, primary acquired nasolacrimal duct obstruction
Recently, the popularity of endonasal dacryocystorhinostomy (Endo-DCR) compared with conventional external dacryocystorhinostomy (Ex-DCR) as increased.1–3 The main factors for this success are the techniques and instrumentation advances, principally in the field of nasal endoscopes and video monitors.4,5 The success rate of endo-DCR has also increased in recent years.4,6 The main purported advantage of endonasal DCR is the absence of a surgical scar. Other advantages include the possibility of simultaneous correction of any nasal pathologic condition, shorter surgical time, and faster recovery.4 However, Ex-DCR is still preferred widely by many surgeons,7–9 with the highest reported success rates.10 This technique is still the gold standard for the management of primary acquired nasolacrimal duct obstruction (PANDO). It has a high surgical success rate which significantly increases with nasolacrimal silicone intubation11 but scar tissue formation at the incision site may be a major drawback for patients.12,13 In the current literature and in a similar survey of a smaller sample of patients interviewed during follow-up examinations of the surgical scar of this surgical technique, a high level of satisfaction has already been noted.13 We therefore developed a telephone survey to evaluate the cosmetic significance of the surgical scar of Ex-DCR as assessed by the patients themselves.
470 patients who underwent Ex-DCR surgery for PANDO from January 2014 to December 2021 after obtained informed consent were considered. The patients with dacryo-phlegmon and lacrimal sac fistulae with skin maceration were excluded. The diagnosis of PANDO was clinically confirmed by preoperative lacrimal probing and lavage, the surgeries were performed under general and locoregional anaesthesia. All patients were operated by two surgeons, G.V. and L.B. using the same surgical procedure: the linear skin incision was 12 mm in length an 8 mm medial to the medial canthus, with one third of incision lying above the medial canthal angle; the orbicularis muscle was dissected; after reaching the periosteum, the anterior lacrimal crest was exposed; C-shaped flaps were prepared on the lacrimal sac; the osteotomy was performed; C-shaped flaps were also prepared on nasal mucosa; only the anterior flaps were sutured with separate 5/0 or 6/0 Vicryl sutures, creating an anastomosis between the lacrimal sac and the nasal cavity; Subcutaneous orbicularis hasn’t been sutured, linear skin incisions were closed using an intradermic continuous 6/0 prolene suture. (Figure 1A-1E) After suturing, the wound was stabilised with sterile plasters (Steristrip) placed over the stitches. (Figure 2A & 2C) Postoperatively, all patients received the same topical antibiotic drops for 10 days, endonasal washes and steroid nasal spray for 10 days. Sutures were removed on post-operative day 8, (Figure 2B & 2D) then moisturising cream with Ubiquinone Q10 and vitamin E was prescribed for 8-10 days. The visual impact of post-surgery scar was assessed after 1 month (Figure 4) and patient satisfaction was determined by a telephone survey. Patients were asked to assess the visibility of the scar, the significance of the scar on a scale of 1 (very good) to 4 (very bad). The responses were then analysed to assess the patient’s perception about the scar.
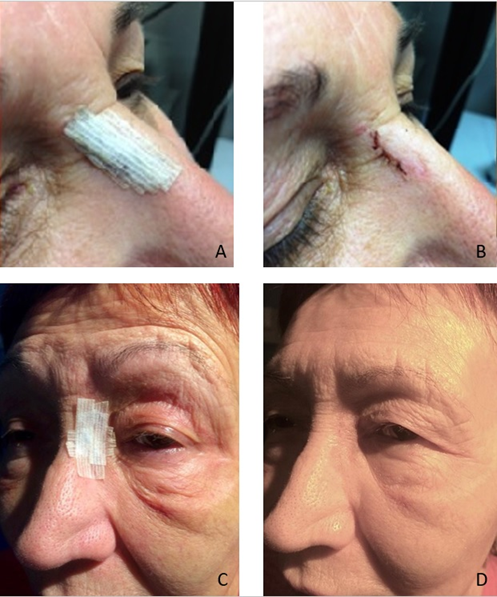
Figure 2 (A) After suturing, the wound was stabilised with sterile plasters (Steristrip) placed over the stitches. (B) Sutures were removed on post-operative day 8 and every patient received the same topical antibiotic drops for 10 days, endonasal washes and steroid nasal spray for 10 days. (D) At 1st post-operative month post-surgery scar was assessed and the patient’s degree of satisfaction is measured by means of a questionnaire.
A total of 470 questionnaires were performed via telephone to the patients on first post operative month, of whom 42 patients had bilateral DCRs. The average patient age was 67.94 +/- 16.07 years. 27.8% patients were male, and 72.2% were female of these 470 DCRs, 356 (75,8 %) were rated as very good 1 on a scale of 4. We had responses about the visibility of the scar in 94 cases, 20% of the study population (2 on a scale of 4, good). 19 scars (4%) were felt to be badly visible by the patients; (3 on a scale of 4, bad) 1 (0,2%) of these scars were assessed as cosmetically important (4, on a scale of 1 to 4, very bad) (Figure 3). 20 of these 114 scars were in 10 patients who had bilateral DCRs (17,5%). Of whom 8 of the 94 cosmetically important scars were in four patients who had bilateral DCRs. (Figure 5A-5D) Thus, 75,8% of patients had invisible or scarcely visible scars, 20% of 470 patients had visible scars, 4% badly visible scars and 0.2% had “cosmetically important” scars. Further, the average age of patients who reported a visible scar (2, on a 1 to 5 scale) was even lower, 51.6 +/- 20.2 year.
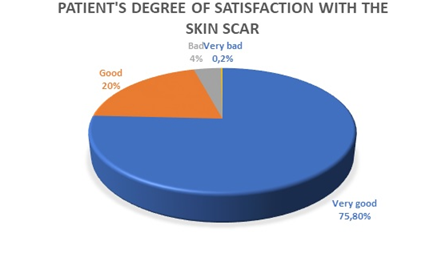
Figure 3 Patient’s degree of satisfaction with skin scar measured by means of a telephone survey: 75,8% of 470 patients had invisible or scarcely visible scars, 20% had visible scars, 4% badly visible scars and 0.2% had “cosmetically important” scars.
Since it was first reported by Toti in 1904 and modified by Dupuy-Dutemps in 1921, Ex-DCR have a success rate of 90% and is generally considered an extremely successful operation.3,12,14 This surgical technique has been the standard treatment for nasolacrimal duct obstruction (NLDO) for over a century.1,3,8 Recently, there has been an interest on how to overcome the disadvantage of cutaneous scar, leading to the evolution of several non-incisional DCR techniques.14–18 Caldwell attempted an endonasal approach for treatment of NLDO more than 100 years ago, but is only been in recent years with the introduction of rigid fiber optic endoscopes it has gained popularity.1,8
We undertook this telephonic survey study to determine the cosmetic significance of the scar after an Ex-DCR surgery to the patients. Other previously published studies about DCR concluded that patient satisfaction may not necessarily correlate with objective success rates19,20 and the patient feedback seems to be the only way to determine the significance of the scar.21 The Vancouver scale is usually used to assess burn scars but there is no established method for patient assessment of surgical scars to the present day.22 Similar scales in patient surveys for also have been used for this purpose.9,23 34 years ago, Harris et al.24 stated that Ex-DCR surgery can be done through an horizontal subciliary incision placed on a lower lid crease. However, it showed a better aesthetic result than the conventional method because the incision site is less noticeable. Today, there are few studies reporting the cosmetic results of this technique.25–27 Mahfouz et al.28 in his comparative study between subciliary incision DCR, conventional Ex-DCR with scar modulating treatment and DCR via transconjunctival approach evaluated their functional and cosmetic outcomes, concluding despite the proposed new surgical innovations, Ex-DCR remains the gold standard and has a slightly better outcome than its subciliary counterpart in the treatment of complete NLDO. For his part, the transconjunctival DCR is a scarless procedure that showed the best cosmetic outcome, but unfortunately its functional outcome is less effective than the other two techniques.28 Just few studies have analysed the cosmetic impact of Ex-DCR in patients, for this reason there is no agreement for post-surgical scars patient assessment method.29
Previously published studies about this technique stated that patient cosmetic satisfaction may not necessarily correlate with objective success rate and the only reliable way to ascertain the significance of the scar is from patient feedbacks.19–22 Tarbet and Custer reported that 2.6% of patients had apparent scar in their study8 reported that 33% of patients rated their scar as visible, but only 3% of them was unsatisfied with the cosmetic result.30 Sharma et al.31 concluded that 19.4% of patients had visible scars, but only 10.3% had aesthetic significant scars. Waly et al.29 reported the cosmetic results after an evaluation by both patients and an oculoplastic surgeon. The examiner scoring was higher than the patient’s one, result that was also noticed by other authors,9,25 27.5% of his patients evaluated their scars as cosmetically significant and the mean patients scar grading was 0.98 ± 1.0 while the mean examiner grading was 1.3 ± 1.0. Devoto et al.9 reported that at third month after surgery 38% of patients grading the post-op scars as minimally visible, 26% moderately visible and 9% severly visible, but six months after surgery 47% of them stated the scars to be minimally visible, 9% graded as moderately visible, and none graded as very visible. In his study Rizvi et al.32 stated that 68% of patients graded their scar as very visible (grade 3) after 2 weeks, reduced to 14% at 6 weeks which further reduction to 2% of patients at 12 weeks. In consecutive follow-up (at 2, 6 and 12 weeks) a change in scar grading perception was found to be highly significant. In this study, we found that a telephone interview with a standardized questionnaire seemed to be a safe and acceptable alternative to the usual outpatient examination, but unfortunately it would have been difficult to contact the same number of patients over longer periods of time. In a study conducted by Mandal et al.33 70 per cent having a telephone survey indicated that it was their preferred review method. During the call, 100% of patients agreed that the telephone survey was a good way to keep in touch and express their preferences.
In our study population, 27.8% patients were male, and 72.2% were female. Female preponderance has been noted in almost all studies on DCR.8,30 This has been attributed by some authors to the anatomically narrower passages in female patients and the loss of the mucosal vascular plexus in postmenopausal women.34 The mean age in our study was 67.94 +/- 16.07 years which was almost the same as the study done by Sharma et al.31 (67y) higher than Devoto et al.9 (61 years), much higher than the studies done Kashkouli et al.35 (52.9y) Ekinci et al.36 (40.8 ± 14.3 years).
The mild difference between the current study and others may be related to the fairer skin type in our Caucasian European population according to Fitzpatrick’s scale (grade between I and III) and the extent of scar may be different in other populations due to skin pigmentation texture differences and healing. In fact, scars could be of more evident in pigmented patients or with a tendency to keloid formation in whom a primary endonasal DCR may be preferred. (Figure 6A & 6B) Also, sutures used were different between studies. Prolene 6\0 continuous intradermal suture was used to close the final scar in all our patients because the monofilament sutures cause less inflammatory reaction but require more ties to assure an adequate maintenance of the knot (Figure 7).29,37 The higher incidence of visible scars may be attributed to younger age of the patients. It has been stated that in this group higher scarring could be caused by smoother and less flawed skin, making the scar more conspicuous.30,38 On the other hand in the study of Sharma et al.31 found the scar to be less prominent in elderly people, which was also reported by other authors.38,39
In conclusion, although endonasal endoscopic DCR is gaining clinical acceptance and popularity, ex-DCR is considered the gold standard in terms of surgical success and high patient satisfaction and should not be excluded when cosmetic results are a criterion for the choice of surgical technique in PANDO. The continuous intradermal monofilament suture allows the surgeon to achieve a scar that is barely visible and has little visual impact on the patient. In addition, our study suggests that telephone interview is a safe and effective method to assess personal perception of postoperative time. The main limitations of our study are that it is a nonrandomized study with no control group and that all surgeries were performed by experienced surgeons, so the results cannot be generalised to all levels of surgeon experience. In our study, only the first postoperative month was evaluated, so there is a possibility that the level of patient satisfaction will be higher in the future.
Patient consent was obtained to contain images in the manuscript.
None.
The author declares that there are no conflicts of interest.

©2023 Vadala, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.