Advances in
eISSN: 2377-4290


Case Report Volume 2 Issue 2
1Nevsehir State Hospital, Turkey
2Aydin State Hospital, Turkey
3Ankara Numune Training and Research Hospital, Turkey
Correspondence: Nevsehir State Hospital, Nevsehir Devlet Hastanesi, Nevsehir, Turkey, Tel +905305923479
Received: February 17, 2015 | Published: April 2, 2015
Citation: Akil H, Keskin S, Mehmet NALP. Hyperbaric oxygen therapy in an isolated cilioretinal artery occlusion: a case report. Adv Ophthalmol Vis Syst. 2015;2(2):63-65. DOI: 10.15406/aovs.2015.02.00039
A 27-year-old female presented to the eye clinic with sudden vision loss in the right eye with onset of 4 hours prior to presentation. On ophthalmic examination, visual acuity was 0.05 in the right eye and 1.0 in the left eye. The anterior segment examination was normal and intraocular pressure was 14 mmHg in both eyes. Dilated fundus examination of the right eye showed an area of retinal ischemia with whitish edges in macular region. The patient was diagnosed as right isolated cilioretinal artery occlusion and underwent twenty sessions of hyperbaric oxygen therapy (120 minutes, 2 ATA). When she returned for follow-up evaluation on the 20th day the vision had improved to 10/10 in the right eye and there was a significant decrease in the previously observed retinal edema.
Keywords: hyperbaric oxygen therapy, cilioretinal artery occlusion
HBOT, hyperbaric oxygen therapy; OCT, optical coherence tomography
The arterial blood supply to the eye is provided by the ophthalmic artery, one of the branches of the internal carotid artery. The branches of the ophthalmic artery which meet the metabolic needs of the globe are central retinal artery, short and long posterior ciliaries, anterior ciliaries. The central retinal artery enters the globe through the optic nerve and supplies blood to the inner layers of the retina. The long posterior ciliary arteries supply blood to the cilioretinal artery, choroid and the outer layers of the retina. The anterior ciliary arteries and posterior ciliary arteries anastamose to form the major arterial circle of the iris.1 The human retina has two separate circulations; the retinal circulation supplies the inner layers of the retina and the choroidal circulation supplies the outer layers.2 The retinal artery occlusions mostly affect inner retinal layers because choroidal circulation supplies the majority of the oxygen to the outer layers of the retina, and only the inner layers of the retina are nourished by the retinal circulation. Cilioretinal artery is present in approximately 15%-30% of population. This artery supplies the macular region of the retina, which is responsible for central vision. Isolated cilioretinal artery occlusion is a rare clinical entity and represents only 3% of all the retinal artery occlusions. Treatment considerations in using hyperbaric oxygen as adjunctive therapy for retinal vascular occlusions are early institution of treatment. We report a patient with isolated cilioretinal artery occlusion who responded to hyperbaric oxygen therapy (HBOT) well.
A 27-year-old female presented to the eye clinic with sudden vision loss in the right eye with onset of 4 hours prior to presentation. Past medical history was unremarkable. Her best corrected visual acuity was 0.05 in the right eye and 1.0 in the left eye with snellen chart. The anterior segment examination of the both eyes with slit lamp biomicroscopy was normal. Intraocular pressure was normal in both eyes. Dilated fundus examination of the right eye showed an area of retinal ischemia with whitish edges in the macular region (Figure 1) and the left eye was normal. Visual field testing was not relevant due to the reduced vision in the right eye. Fluorescein angiography of the right eye showed delayed filling of the cilioretinal artery and masking of choroidal fluorescence because of the retinal edema. Fluorescein angiography was normal in the left eye. Optical coherence tomography (OCT) (Carl Zeiss Meditec Inc., Dublin, CA) revealed increase in thickness and hyper-reflectivity of the inner retinal layers in affected area and shadowing with decreased reflectivity of photoreceptor and retinal pigment epithelial layers, consistent with intracellular edema (Figure 2). After the diagnosis, the patient was treated with oral carbonic anhydrase inhibitors (acetazolamide 250mg tablet 1x2), intravenous hyperosmolar agent (300 cc mannitol) and topical antiglaucomatous medication (brimonidine/timolol combination).
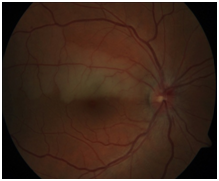
Figure 1 The color fundus photography of the right eye that shows retinal ischemia with whitish edges.
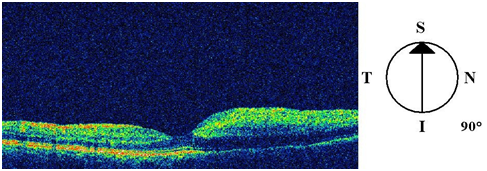
Figure 2 Optical coherence tomography of the right eye revealed increase in thickness and hyper-reflectivity of the inner retinal layers in affected area consistent with intracellular edema.
Ocular massage of the right eye was carried out for 15 minutes than the patient was referred to the HBOT center to be treated with HBOT at 2.0 ATA (atmosphere absolute) oxygen 120 minutes daily for 20 sessions. Patient was checked for any other disease which can cause vascular occlusion but only high blood homocystein; low vitamin B12 levels were found in laboratory tests and treatment was started. Twenty days after the initiation of the therapy visual acuity of the right eye improved to 1.0. Visual field test was interpreted as paracentral scotoma localized below the horizontal midline which is consistent with superior nerve fiber damage in the right eye (Figure 3). Three months after the initial visit, repeat fluorescein angiography showed remarkable improvement in fluorescein filling of the cilioretinal artery, which started almost at the same time as the choroidal flush (Figure 4). OCT demonstrated thinning of the neural sensory retina with normal foveal contour (Figure 5). Repeat perimetry showed a smaller paracentral scotom compared to the defect on the 20th day of treatment (Figure 6).

Figure 3 Visual field test was interpreted as paracentral scotoma localized below the horizontal midline which is consistent with superior nerve fiber damage in the right eye.
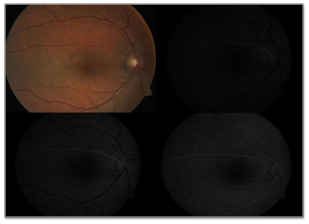
Figure 4 Three months after the initial visit, repeat fluorescein angiography showed remarkable improvement in fluorescein filling of the cilioretinal artery, which started almost at the same time as the choroidal flush.
HBOT may be used as an adjuvant or major treatment modality in many ocular disorders, progress in this field needs understanding the effects of hyperoxia on the normal eye. According to theoretical models during systemic hyperoxia, oxygen could be supplied to the deeper regions of the retina by choroid. So under hyperbaric oxygenation, the calculations showed that choroid should meet needed oxygen to both inner and outer retinal layers.3,4 Many clinicians have been using different treatment choices to decrease intraocular pressure and produce vasodilatation for retinal artery occlusions with a main purpose of facilitating movement of the emboli if present. Most of these conventional treatments are found to be ineffective,5 but HBOT may be useful reversing vision loss in at least some cases of retinal artery occlusion. So we treated our patient with HBOT besides conventional treatment regimens. Hertzog et al.6 studied the importance of the HBOT timing in central retinal artery occlusion cases. They reported that preserving visual function may be possible if HBOT applied within 8 hours from the onset Henderson et al.7 Evaluated the prognosis of 16 patients treated with HBOT for central retinal artery occlusion. The patients who had been late for the treatment more than 24 hours, showed no improvement.
Weiss et al.8 reported five patients with symptoms secondary to branch and cilioretinal artery occlusion who were treated with HBOT. All patients responded to HBOT well without any complication. They concluded that HBOT may be more effective treatment for patients with branch retinal and cilioretinal artery occlusion because of the localized ischemic lesion compared to the central retinal artery occlusion Takeuchi et al.9 Reported a patient with central retinal artery occlusion occurring after a long surgical procedure. HBOT and systemic vasodilator treatment initiated after the diagnosis and the therapy resulted in improvement of the affected eye.
The visual prognosis associated with retinal artery occlusions remains poor and current acute managements have limited and unproven benefit to improve the vision.10,11 Many studies reported a variety of treatment attempts such as ocular massage, acetylsalicylic acid, beta-blocker, carbogen (95%oxygen and 5% carbon dioxide), topical timolol maleate, acetazolamide and anterior chamber paracentesis but these have not been found as a safe and efficacious option for this visually disabling condition.12,13 Our patient responded to the HBOT treatment well. The improvement may also be related with the early timing of the treatment, the young age, and absence of the any precipitating factor. HBOT is a relatively safe, easily administered treatment which may produce an improvement in vision.6-9 Further study is required to define the value of this therapy in the treatment of retinal artery occlusions.
None.
Author declares that there is no conflict of interest.

©2015 Akil, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Glaucoma Week 2026 (March 8th to 14th), we proudly join the global movement
to raise awareness about glaucoma often called the silent thief of sight. As one of the leading causes of irreversible
blindness, glaucoma often progresses unnoticed in its early stages, making regular eye examinations vital for early detection
and timely treatment.
To emphasize the importance of proactive eye care and to support this crucial campaign, we are offering a 40% discount on any
article submitted to AOVS. Let’s unite to spread awareness, inspire preventive eye care, and champion the fight against glaucoma.
World Glaucoma Week 2026 (March 8th to 14th), we proudly join the global movement
to raise awareness about glaucoma often called the silent thief of sight. As one of the leading causes of irreversible
blindness, glaucoma often progresses unnoticed in its early stages, making regular eye examinations vital for early detection
and timely treatment.
To emphasize the importance of proactive eye care and to support this crucial campaign, we are offering a 40% discount on any
article submitted to AOVS. Let’s unite to spread awareness, inspire preventive eye care, and champion the fight against glaucoma.