Advances in
eISSN: 2377-4290


Case Report Volume 4 Issue 4
Medical University of Varna, Bulgaria
Correspondence: Grupcheva CN, Medical University - Varna, Bulgaria, 15 Doyran St. Varna 9002, Bulgaria, Tel 00359 89 9096709
Received: June 23, 2016 | Published: July 7, 2016
Citation: Grupchev DI, Radeva MN, Grupcheva CN. Blepharoplasty: one touch-serious complication. Adv Ophthalmol Vis Syst. 2016;4(4):112-114. DOI: 10.15406/aovs.2016.04.00118
Purpose: To describe and analyze a serious corneal complication following bilateral (4 lid) blepharoplasty by a plastic surgeon on patient with ultimate eye.
Case: A 59-year-old male with complicated eye history of pathological myopia, bilateral cataract surgery (June and September 2011) on both eyes and right eye vitrectomy (December 2012) following retinal detachment, decided to improve his esthetic appearance. After the plastic surgery procedure he had significantly decreased vision in his good eye. He was examined by an ophthalmologist 6 days after the plastic surgery and was diagnosed with severe bacterial conjunctivitis and a corneal foreign body. After adequate treatment it took 48 hours for the infection to be controlled but on biomicroscopy, although the cornea was absolutely clear, a strange linear lesion was identified. This lesion was apparently a result of electro-knife touch and was a reason for very poor vision of 0.1, which would not improve even with a pinhole. Corneal topography revealed 8 diopters irregular astigmatism. Anterior OCT demonstrated structural damage resulting in the reduction of corneal thickness to one half of its original size. In vivo confocal microscopy demonstrated a local area of keratocyte loss, with activation of the surrounding keratocytes. RGP lens improved the vision to useful 0.9, as the fellow eye had vision of 0.4 with notable metamorphopsia.
Conclusion: Although the complications of lower lid noninvasive blepharoplasty appear to be minimal, in the reported case corneal damage had a significant negative quality of vision and life impact. Protection of the eye surface and extreme care for the delicate anterior eye structures should be taken during surgery.
Keywords: Cornea, In vivo confocal microscopy, blepharoplasty
LSICM; laser scanning in vivo confocal microscopy; OCT; optical coherence tomography; RGP; rigid gas permeable lens
Blepharoplasty is the most commonly performed bilateral eye surgery by ophthalmologist and plastic surgeons.1 Regarding the ocular surface, it is usually associated with “minor” complications such as conjunctival oedema and dry eye.2 Although, the patient’s prospective for those “minor” complications might be different, as they are associated with significant visual, perceptual and cosmetic discomfort, usually the patient bears them in the interest of a final cosmetic improvement.3 When patients with eye problems give their consent for blepharoplasty, they must be warned of the specific potential complications. Although rare, retrobulbar haematoma4 might be a reason for severely decreased vision and even permanent blindness. Dry eye might have significant long-term impact on the patient’s vision and quality of life for a substantial period of time.
Most of the complications might be prevented with proper pre- and postoperative management such as compression bandage, antibiotic ointments, long-term lubrication, patient education, frequent examination, etc.5 Most importantly, during the surgery, together with elegant technique and precise excisions, any surgeon (regardless of their subspecialty) must pay special attention to the ocular surface and the conjunctival and corneal protection. For example, rough manipulation of the conjunctiva might be associated with damage of the goblet cells and, subsequently, dry eye associated with long-term, even life-long discomfort.3,6
We report a case of a 59-year-old male with complicated eye history of high myopia, bilateral cataract surgery (June and September 2011) on both eyes, and subsequently, right-eye vitrectomy (December 2012) following retinal detachment. The patient decided to improve his esthetic appearance. For the last 10 years he had mild ptosis of the right eyelid, which worsened especially following the vitrectomy. During the esthetic consultation he was encouraged by the plastic surgeon to improve his eye appearance with a “total” 4 eyelid blepharoplasty. The surgery included upper-lid classic blepharoplasty with an excision of more skin on the right side to compensate for the ptosis. Judging on the postoperative appearance of the wound, electro-knife was used for skin and conjunctival incisions. For the closure of the upper lid skin 6.0 Prolene was used. The surgeon also performed “noninvasive” lower-lid blepharoplasty, only on the medial fat pad. The recommendation that the patient remembered was to use ice compresses several times a day. No drops or eye ointments were prescribed.
On the next day, following the surgery, the patient noted significantly decreased vision in his good eye. He started to have a bit of purulent discharge and perceived his “bad vision” as part of the recovery process. He actively demanded ophthalmology examination, and appeared in the University Eye Clinic (in another EU country) 6 days after the plastic surgery. At that stage the vision was impossible to examine, as both fornices were full of purulent discharge and chemosis was significant. Both corneas had epithelial oedema with punctate staining on application of fluorescein drops. The left cornea featured small foreign body at 4.30, very close to the limbus. The corneal body was removed, the fornices were cleaned from the discharge and adequate antimicrobial treatment, together with epithelializing gel, was prescribed to the patient. In 48 hours the infection was controlled, but on biomicroscopy, although the cornea was absolutely clear, a strange linear lesion was identified (Figure 1a).
The auto refraction of the left eye was impossible, and vision was lower at 0.1, without pinhole improvement. Corneal topography revealed 8 diopters irregular astigmatism, resembling keratoconus or ectasia (Figure 1b&c). After careful analysis the lesion was identified as electro-knife touch. The lesion was in a position matching the direction of the electro-knife at the moment of mid fat pad surgery. OCT revealed significant collagen compaction with very sharp demarcation to the neighboring cornea and confirmed the topography observations (Figure 1d). In vivo confocal microscopy demonstrated local area of keratocyte loss, approximately ½ of the corneal thickness (Figure 2a), with activation of the surrounding keratocytes (Figure 2b). The epithelium above the lesion was multilayered with signs of activity, obviously with tendency to fill in the gap (Figure 2c). The posterior stroma and endothelium were unremarkable (Figure 2d). A spherical RGP lens was fitted with an achievement of a good position and improved vision to 0.9. The improvement of the left eye immediately changed the patient’s visual performance and satisfaction, as the fellow eye had vision of 0.4 with notable metamorphopsia.
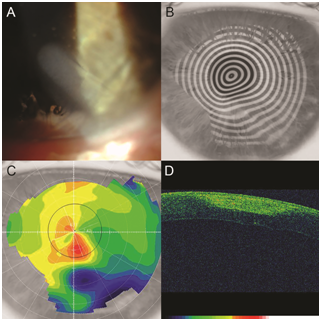
Figure 1 Clinical findings of the left cornea of the reported case. Slit-lamp photography demonstrating linear lesion, measured 2 mm in width and 6.5 mm in length with oblique location starting at 5 o’clock on lower limbus and crossing the entrance of the pupil (Figure 1a). Corneal topography - Placido image (Figure 1b) and colour-coded keratometric map (Figure 1c) demonstrating irregular astigmatism. OCT demonstrating significant collagen compaction with very sharp demarcation to the neighboring cornea (Figure 1d).
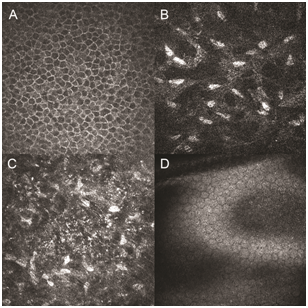
Figure 2 In vivo confocal microscopy demonstrated that the epithelium above the lesion was multilayered with signs of activity (Figure 2a). In the stroma outside of the visible lesion keratocytes presented activity and “networking” (Figure 2b). Stroma within the lesion was significantly destructured with localized keratocyte damage (approximately ½ of the corneal thickness) (Figure 2c). The posterior stroma and endothelium were unremarkable (Figure 2d).
The patient was followed for a period of three months and showed gradual improvement, but with significant structural disorganization resulting in variable, irregular astigmatism. The potential for complete corneal restoration is obviously very limited. Regardless of the fact that in such cases refractive procedures, or even hypothetically crosslinking might be beneficial, the risk of complications for this specific eye was a reason for a more conservative approach. The patient had previous experience with RGP lenses, the improvement of vision was instantaneous, therefore with proper selection of the material and design of RGP the risk for ocular surface is ignorable. The senior author believes that optical enhancement with RGP is the best and the safest approach for this case.
Blepharoplasty is one of the most desired cosmetic surgical procedures, believed to be safe and with minimal complications. However, in the literature there are several reports for surgical mishaps, not necessarily related to the blepharoplasty per se.7,8 Our case is unusual, but considering that ultimate eye is a problem with increased frequency after 50 years of age (as a result of different pathology), we believe that extra measures should be taken in those special cases, when they are consented for cosmetic improvement. According to the patient’s explanation he was not even asked how good his vision was, and he, himself, did not consider blepharoplasty as an eye-endangering procedure. Unfortunately, he ended up with severe damage which might require RGP lens correction for life. Although this patient was wearing lenses for 20+ years, he was experiencing problems and his acceptance of this kind of correction was with a great deal of concern. Moreover, in a situation when only one eye will be corrected with RGP lens, the perceptual comfort is questionable.
The lesson learned from this case is that special precautions should be taken for protection of the ocular surface when electro-knife or radio-knife is used.1,3,9 In any patient, but especially in those with visual problems, dry eye would decrease the quality of vision and life. It is logical that electro-knife might damage the goblet cells and the Meibomian glands. We have managed to evaluate the microstructural dynamics of the cornea and our observation demonstrates very slow recovery after such damage of the epithelium and also anterior stroma. Interestingly, the damage is much localized, but the affected area is completely destructured, with grave prognosis regarding recovery. Considering that the thickness of the damage is more than 200 microns, one can assume that conjunctival damages would be full-thickness and when tarsal conjunctiva is cauterized Meibomian glans are injured also. If the patient looks up, the damage of the sclera might also have refractive consequences. So, in summary, when working in a “noninvasive” manner, the surgeon must take care of any adjacent anterior segment structure, and a protective shield is ultimately a must.
Cosmetic eye surgery is an attractive procedure for the male and female gender after the age of 50-55, as it improves the appearance and it may really enhance the looks of a person. In general, it is fast, with a relatively short recovery period and satisfactory outcomes. However, it is performed close to the ocular surface which is most important for the patients’ eye comfort. There are 3 recognized levels of eye comfort: visual (I see well), perceptual (I feel my eyes fresh and lubricated) and cosmetic (my eyes are bright and no redness is visible). In the reported case, as a result of plastic surgery, all three levels of eye comfort were negatively impacted. This situation might last for the entire life of the patient, when he becomes dependent on RGP contact lenses. In fact, five months after the surgery the patient was not concerned about his looks, but was very anxious about his poor vision, followed by discomfort and redness.
The complications of lower-lid noninvasive blepharoplasty appear to be minimal; however, in the reported case corneal damage had a significant negative quality of vision and life impact. Protection of the eye surface and also extreme care for the delicate anterior eye structures should be taken during lid surgery at all times, by both plastic and ophthalmic surgeons.
None.
We are grateful to Mr ANB for his agreement to allow all evaluations and analyses and his will to present the case to the wider medical specialists.
None.
None.

©2016 Grupchev, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Glaucoma Week 2026 (March 8th to 14th), we proudly join the global movement
to raise awareness about glaucoma often called the silent thief of sight. As one of the leading causes of irreversible
blindness, glaucoma often progresses unnoticed in its early stages, making regular eye examinations vital for early detection
and timely treatment.
To emphasize the importance of proactive eye care and to support this crucial campaign, we are offering a 40% discount on any
article submitted to AOVS. Let’s unite to spread awareness, inspire preventive eye care, and champion the fight against glaucoma.
World Glaucoma Week 2026 (March 8th to 14th), we proudly join the global movement
to raise awareness about glaucoma often called the silent thief of sight. As one of the leading causes of irreversible
blindness, glaucoma often progresses unnoticed in its early stages, making regular eye examinations vital for early detection
and timely treatment.
To emphasize the importance of proactive eye care and to support this crucial campaign, we are offering a 40% discount on any
article submitted to AOVS. Let’s unite to spread awareness, inspire preventive eye care, and champion the fight against glaucoma.