Advances in
eISSN: 2377-4290


Case Report Volume 14 Issue 1
1Philadelphia College of Osteopathic Medicine, Moultrie, GA, USA
2Clayton Eye Center, Morrow, GA, USA
Correspondence: Trung Thanh Bui MS, Philadelphia College of Osteopathic Medicine, Moultrie, GA, USA
Received: April 01, 2024 | Published: April 10, 2024
Citation: Bui TT, Garcia EJ, Kim JL. Bilateral anterior capsular phimosis in an 85-year-old female patient after stand-alone cataract extraction with intraocular lens implantation. Adv Ophthalmol Vis Syst. 2024;14(1):36-39. DOI: 10.15406/aovs.2024.14.00459
Introduction: Anterior capsular phimosis is a rare complication after cataract extraction with intraocular lens implantation.
Patient and clinical findings: An 85-year-old female underwent manual phacoemulsification with toric intraocular lens implantation in the right eye (OD) without any post-operative complications. Approximately 1.5 weeks later, she had the same procedure in the left eye (OS) with similar success. At post-operative week 6 OD and week 4 OS, distance visual acuity without correction was 20/400 OD and hand motion (HM) OS. Anterior segment examination revealed intraocular lens implants with a significant fibrotic anterior capsule in both eyes. Posterior segment examination showed pigmentary macular changes in both eyes that were unchanged from the pre-operative evaluation.
Diagnosis, intervention, and outcomes: The patient was diagnosed with bilateral anterior capsular phimosis. She underwent Nd:YAG laser capsulotomy in the left eye, then in the right eye 1 week later. At Nd: YAG laser capsulotomy post-operative day 4 OD and week 2 OS, distance visual acuity without correction was 20/40 OD, OS with best corrected visual acuity 20/30 OD, OS.
Conclusions: Anterior capsular phimosis can occur in both eyes sooner than 4 weeks after cataract extraction with intraocular lens implantation in a patient with no risk factors.
Keywords: anterior capsular phimosis, capsular contraction syndrome, cataract surgery, post- operative complication
Cataract extraction with intraocular lens implantation is the standard of care in patients with cataracts when changes in glasses prescription can no longer improve the patient’s visual acuity.1 Continuous curvilinear capsulorrhexis of the anterior capsule is performed during the surgery to preserve the lens capsule as the cataract is being extracted. Post-operatively, the anterior capsule remnant can infrequently become fibrotic and contract, resulting in anterior capsular phimosis that decreases the patient’s visual acuity. With the incidence rate of posterior capsular opacification ranging from 20-100%, depending on age, studies have shown that the incidence of anterior capsular phimosis is approximately 1.5%.2,3
The risk factors of anterior capsular phimosis include pseudoexfoliation, uveitis, diabetic retinopathy, retinitis pigmentosa, high myopia, and myotonic dystrophy.4−7 Other surgical variables, such as small capsulorrhexis and intraocular lens composition, can also contribute to the risk of developing anterior capsular phimosis after cataract extraction with intraocular lens implantation.8,9 In cases where the anterior capsular phimosis does not affect visual acuity significantly, the patient can be monitored without any treatment.10 In cases where the anterior capsular phimosis leads to significant decrease in visual acuity, elective procedures, such as Nd:YAG laser capsulotomy or surgical excision using a vitrector or microscissors, have been used with success to improve visual acuity.11,12 When the fibrotic anterior capsule remnant contracts so much that it compromises the integrity of the intraocular lens implant, surgical extraction may be required.15
A literature review shows several case reports of unilateral anterior capsular phimosis that occur after cataract extraction with intraocular lens implantation; and the earliest case occurs at 2 months after the surgery in a patient with no risk factors.10,13−15 We are presenting a case report of bilateral anterior capsular phimosis that presented 4 weeks after a stand-alone cataract extraction with intraocular lens implantation in the second eye in a patient with no risk factors.
Patient’s consent for the publication of this case report was obtained at the last follow up visit.
The nature of this case report and its possible consequences were explained to the patient; and she acknowledged understanding. This case report follows the tenets of the Declaration of Helsinki.
An 85-year-old female with best corrected visual acuity 20/400 OD and 20/400 OS underwent uneventful manual phacoemulsification with toric intraocular lens implantation (Alcon AcrySof SA6AT7) in the right eye. Post-operatively, the patient was prescribed moxifloxacin, bromfenac, and prednisolone eye drops. Approximately 1.5 weeks after the surgery in the right eye, the patient underwent uneventful phacoemulsification with toric intraocular lens implantation (Alcon AcrySof SA6AT5) in the left eye. The same post-operative eye drops were prescribed for the left eye.
At post-operative week 3 (POW3) OD and week 1 (POW1) OS, the patient stated that she was doing well. Distance visual acuity without correction was 20/80 pinhole no improvement (PHNI); 20/100 PHNI OS with best corrected visual acuity 20/30 OD, OS (Table 1). Anterior segment findings were unremarkable.
|
Visit |
scDVA OD |
scDVA OS |
|
Pre-operative |
scDVA CF3 |
20/400 |
|
BCVA 20/400 |
BCVA 20/400 |
|
|
Surgery |
Cataract extraction with toric IOL (SA6AT7) implantation |
|
|
POW1 OD |
scDVA 20/50 |
|
|
BCVA 2040 |
||
|
Surgery |
Cataract extraction with toric IOL (SA6AT5) implantation |
|
|
POW3 OD & POW1 OS |
scDVA 20/80 |
scDVA 20/100 |
|
BCVA 20/30 |
BCVA 20/30 |
|
|
POW6 OD & POW4 OS |
scDVA 20/400 |
scDVA HM |
|
Laser |
Nd:YAG capsulotomy |
|
|
Laser |
Nd:YAG capsulotomy |
|
|
POD4 OD & POW2 OS |
scDVA 20/40 |
scDVA 20/40 |
|
|
BCVA 20/30 |
BCVA 20/30 |
Table 1 Summary of visual acuity at each visit
DVA, distance visual acuity; sc, uncorrected; IOL, intraocular lens; CF3, counting fingers at 3 feet; HM, hand motion; POW, post-operative week; POD, post-operative day; BCVA, best corrected visual acuity.
At post-operative week 6 OD and week 4 OS, the patient complained of blurry vision OS > OD with onset 5 days before this visit. Distance visual acuity without correction was 20/400 PHNI OD; HM PHNI OS. Potential acuity meter (PAM) was 20/400 OD, OS. Anterior segment examination revealed toric intraocular lens implants in good position but partially obscured by the white fibrotic anterior capsule remnant in both eyes (Figure 1A, 1B). Examination of posterior segment showed pigmentary changes in the macula of both eyes that were unchanged from the pre-operative evaluation. Optical coherence topography (OCT) macula of both eyes showed no changes when compared to scans taken at the pre-operative evaluation. The patient was diagnosed with bilateral anterior capsular phimosis and scheduled for Nd:YAG laser capsulotomy in both eyes.
The patient underwent uneventful Nd:YAG laser capsulotomy in the left eye, then in the right eye 1 week after that. At Nd:YAG laser capsulotomy post-operative day 4 OD and week 2 OS, distance visual acuity without correction was 20/40 PHNI OD, OS with best corrected visual acuity 20/30 OD, OS (Table 1). Anterior segment examination showed toric intraocular lens implants were in good position with open anterior capsules and closed posterior capsules in both eyes with no significant posterior capsular opacity (Figure 1C, 1D). Posterior segment examination showed pigmentary changes in the macular of both eyes that were unchanged from the pre- operative evaluation (Figure 2A, 2B).
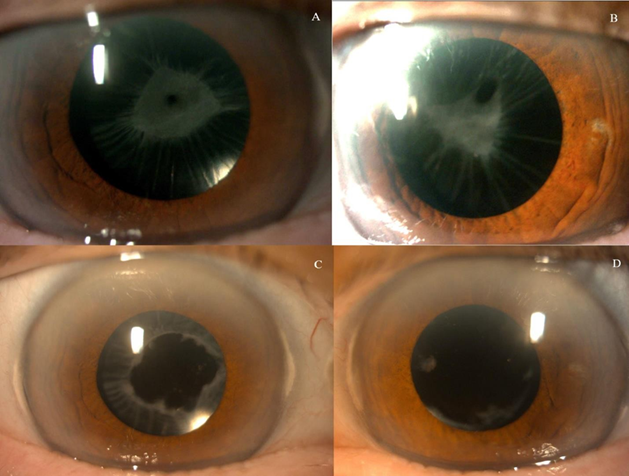
Figure 1 Anterior capsular phimosis in the right eye (A) and left eye (B) at follow-up visit status post cataract extraction with toric intraocular lens implantation week 6 OD and week 4 OS. Open anterior capsule in the right eye (C) and in the left eye (D) at follow-up visit status post Nd:YAG laser capsulotomy at week 3 OD and week 4 OS.
Anterior capsular phimosis is a rare occurrence after cataract extraction with intraocular lens implantation when the anterior capsule remnant becomes fibrotic and contracts, which can cause diminished visual acuity.
Review of the current literature reveals 1 case series and 3 case reports of unilateral anterior capsular phimosis that presented after a cataract extraction with intraocular lens implantation (Table 2). One patient who initially presented with unilateral anterior capsular phimosis acquired bilateral anterior capsular phimosis when she underwent cataract extraction with intraocular lens implantation in the second eye 2 years later.10 This appears to be the first case report of bilateral sequential anterior capsular phimosis after stand-alone cataract extraction with intraocular lens implantation.
|
Study |
#Pts |
Eye affected |
Time of onset |
Treatment |
|
Kang et al.,10 |
3 |
OD then OS |
POM3-18 |
No treatment Observation only |
|
OD |
||||
|
OD |
||||
|
Al-Kharashi et al.,13 |
1 |
OD |
POM4 |
Surgical excision of anterior capsular phimosis by repeated continuous curvilinear capsulorrhexis |
|
Narnaware et al.,14 |
1 |
OD |
POM2 |
No data reported |
|
Naik et al.,15 |
1 |
OD |
POY7 |
IOL extraction and implantation of scleral fixated IOL |
Table 2 Summary of 1 case series and 3 case reports of unilateral anterior capsular phimosis
POM, post-operative month; POY, post-operative year; IOL, intraocular lens.
Jin-Poi et al.,7 reported a case of anterior capsular phimosis that presented as early as post- operative week 2 in a patient with advanced retinitis pigmentosa.7 This case report demonstrates how aggressive this post-operative complication can manifest in patients with predisposition for anterior capsular phimosis. On the other hand, Narnaware et al.,14 reported the onset of anterior capsular phimosis at post-operative month 2 in a patient without any known risk factors.14 Our case report suggests that anterior capsular phimosis can present as early as 4 weeks after cataract extraction with intraocular lens implantation. Our patient had rapid onset of anterior capsular phimosis in the absence of risk factors, such as pseudoexfoliation, uveitis, diabetic retinopathy, or retinitis pigmentosa. Alcon AcrySof SN60WF intraocular lenses have been shown to be associated with higher incidence of anterior capsular phimosis in patients with known risk factors and this patient received Alcon AcrySof SA6AT intraocular lenses which have an identical composition.
Naik et al.,15 reported a case of unilateral anterior capsular phimosis where both haptics folded on the intraocular lens implant inside the capsule without any cells, flare, or posterior synechiae.15 The author cited the risk of severe image distortion, metamorphopsia, and resultant aniseikonia as the reason why Nd:YAG laser capsulotomy was not an appropriate treatment in this case.
Instead, the patient in this case report underwent intraocular lens extraction and implantation of scleral-fixated intraocular lens implant.15 The final best corrected vision after this surgery was 20/20. It is unclear whether the patient had any risk factors for anterior capsular phimosis.
While Nd:YAG laser capsulotomy was used to restore the visual acuity with success in other case reports, Kang et al. reported 3 cases of anterior capsular phimosis with stable visual acuity and anterior capsulotomy opening that did not require any treatment.10 The author reported that one of the patients had type 2 diabetes; but no medical history was reported. All patients in this case series had SA60AT intraocular lens implants.10
The patient in the present case did not have any risk factors for anterior capsular phimosis. While the visual acuity initially improved following cataract surgery, the rapid onset of bilateral anterior capsular phimosis led to significantly decreased vision. Anterior segment examination indicated intraocular lens implants were in good position bilaterally. As such, the decision was made to perform Nd:YAG laser capsulotomy in both eyes. Similar to other case reports of unilateral anterior capsular phimosis, Nd:YAG laser capsulotomy was performed to successfully treat bilateral anterior capsular phimosis.
This case highlights the first reported incident of bilateral anterior capsular phimosis in a patient without risk factors. It also demonstrates that anterior capsular phimosis can occur as soon as 4 weeks after manual phacoemulsification with intraocular lens implantation.
What was known:
What this paper adds:
None.
The authors report no conflicts of interest.

©2024 Bui, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.