Advances in
eISSN: 2377-4290


Research Article Volume 4 Issue 6
1Anhembi Morumbi University, Brazil
2Department Ophthalmology, Anhembi Morumbi University, Brazil
Correspondence: Ana L Credidio, School of Medicine, Anhembi Morumbi University, Laureate International Universities, São Paulo, SP, Francisco Cruz street, 239, apartment 21, ZIP CODE 04117-091, São Paulo, SP, Brazil, Tel +55-11971708927
Received: July 24, 2016 | Published: September 7, 2016
Citation: Credidio AL, Balarim G, Ferraz C. Assessment of the effects of intense pulsed light procedure in porcine eyes with different treatment strategies. Adv Ophthalmol Vis Syst. 2016;4(6):159-163. DOI: 10.15406/aovs.2016.04.00132
Introduction: The use of intense pulsed light (IPL) increased in recent years. This study aimed to identify the types and degrees of eye injury caused by IPL in ‘’ex vivo’’ porcine eye, correlating the distance from the shooting location of the ocular region, power and pulse duration used.
Methods: Experimental study. Intense pulsed light (IPL) was applied in five different treatment strategies (7J/5ms, 9 J/12ms, 10J/18ms, 11J/26ms and 12J/34ms) with corneal thickness evaluation pre and post procedure and classification of degree of eye injury observed in biomicroscopy slit lamp in the phase after the procedure.
Results: There was no change in pachymetry in the group of lower power and frequency - Group 1 (7J/5ms), but from 9J/12ms (groups 2, 3, 4 and 5) all groups presented reduction of corneal thickness. The biomicroscopy analysis in slit lamp showed that inferior keratitis was observed a greater number of eyes subjected to intense pulsed light procedure with minor powers (7 and 9J) and iris lesion were observed a greater number of eyes subjected to light procedure intense pulsed with greater powers (12J).
Conclusion: Ocular adverse effects were observed in all strategies of the intense light pulse procedure in porcine eye. The intraocular effects such as iris lesions were more evident in treatments with higher powers. Change of corneal thickness was observed with intense pulsed light from 9J and 12 ms. Because of the lesions observed in the evaluation after the procedure we corroborate the recommendation of using scleral lenses, possibly made of stainless steel, to dissipate the energy of the IPL when ophthalmic procedures or esthetic procedure near the eyeball margin.
Keywords: intense pulsed light, eye injury, corneal thickness
The Intense Pulsed Light (IPL) may be used for the treatment of acne, photoepilation, photorejuvenation and more recently their use has been advocated for treatment of meibomian gland dysfunction and dry eye. For the treatment of dysfunction of the meibomian gland, Intense Pulsed Light was used with the same acne treatment settings in the scenario Fitzpatrick type 1, fluent between 8 and 12J/cm2 with a 20 pulse width of 30 milliseconds depending on skin response, using four to six applications, spaced in 1 month.1 Being a relatively new method, the eye problems resulting from inappropriate IPL use are not well documented in the literature, but there are bilateral anterior uveitis accounts, decreased pupillary motility, epithelial lesions, iris atrophy, posterior synechiae and corneal pigment deposit of contact lens.2 The purpose of this study is to recognize the types and degrees of eye injuries caused by intense pulsed light according to each power, pulse duration and fluence used. From these data collected we can determine the risks of near eye area procedure and makes it safer in ophthalmological perspective.
This is an experimental prospective study in which were used “ex vivo” porcine eye. The eyes were evaluated by slit lamp and data as corneal integrity, corneal thickness, and iris shape of the edge and transparency of the crystalline lens were previously analyzed for the procedure. The measurement of corneal thickness was performed with ultrasonic pachymeter. Tomey SP100 prior to application of IPL.
No eye showed evidence of change in corneal integrity, shape of the iris edge and transparency of the lens before to the procedure. In total, were used fifty (50) ‘’ex vivo’’ porcine eyes randomly and equally divided into the following groups:
For the application of intense pulsed light Adéna® equipament was used, with a wavelength of 475-1100nm, intensity 5 to 17J/cm2 with pulse duration of 2 to 100ms and energy from 6 to 18 J/cm². The group data were statistically analyzed descriptively and analysis of variance was carried out based on a repeated measurement model and analysis of variance (ANOVA) with one factor.
The variables analyzed were: 1) corneal thickness and 2) Changes observed slit lamp.
1) Corneal Thickness: Descriptive thickness for pre and post procedure intense light pulse is shown in Table 1. Comparisons between the thickness of cornea measurements of pre and post procedure for each of the groups, the results showed that for group 1 there was no difference in thicknesses before and after treatment, however, for the other groups the average thickness of corneas before treatment were significantly higher than the post-treatment, that is, groups 2, 3, 4 and 5 using from 9J and 12ms pulse was a significant decrease in corneal thickness after the applied treatment (Graphic 1).
Descriptive values |
|||||||
Group |
Phase |
n |
Minimum |
Maximum |
Median |
Average |
d.p. |
1 |
Pre |
10 |
714,0 |
870,0 |
780,0 |
792,2 |
46,9 |
Post |
10 |
739,0 |
884,0 |
804,5 |
801,0 |
44,2 |
|
2 |
Pre |
10 |
809,0 |
928,0 |
860,0 |
859,9 |
37,4 |
Post |
10 |
786,0 |
894,0 |
827,0 |
828,0 |
36,1 |
|
3 |
Pre |
10 |
775,0 |
894,0 |
866,5 |
855,2 |
37,0 |
Post |
10 |
745,0 |
868,0 |
810,0 |
812,5 |
37,3 |
|
4 |
Pre |
10 |
746,0 |
858,0 |
787,0 |
798,2 |
42,7 |
Post |
10 |
701,0 |
802,0 |
769,5 |
765,2 |
34,9 |
|
5 |
Pre |
10 |
735,0 |
854,0 |
809,0 |
807,2 |
39,4 |
|
Post |
10 |
730,0 |
818,0 |
794,0 |
782,4 |
31,0 |
Table 1 Descriptive and comparative values of measurements of the thickness of the cornea in porcine eye in different groups (1 to 5) and phase of pre- and post-treatment (in microns)
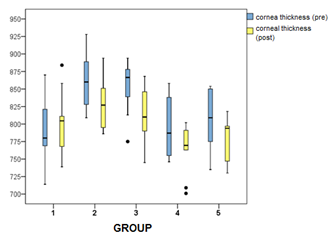
Graphic 1 Measures Box plot of corneal thickness in relation to the factors group (1 to 5) and evaluation phase (pre- or post-treatment).
Graphic 1
Measures Boxplot of corneal thickness in relation to the factors group (1 to 5) and evaluation phase (pre- or post-treatment).
2) Changes observed in biomicroscopy slit lamp:The slit lamp examination was made in the pre and post intense pulsed light application procedure. The degree of injury was classified as follows as shown in Table 2.
Group 1 |
Group 2 |
Group 3 |
Group 4 |
Group 5 |
7J 5 ms |
9J 12 ms |
10J 18 ms |
11J 26 ms |
12 J 34 ms |
Eye 1: C |
Eye 1: N |
Eye 1: N |
Eye 1: N |
Eye 1: N |
Eye 2: C I |
Eye 2: C I |
Eye 2: N |
Eye 2: DE/ I<10 |
Eye 2: N |
Eye 3: C I |
Eye 3: C I |
Eye 3: C |
Eye 3: C |
Eye 3: DE |
Eye 4: C |
Eye 4: N |
Eye 4: DE |
Eye 4: C |
Eye 4: CI/ I<25 |
Eye 5: C |
Eye 5: N |
Eye 5: CI/I<10 |
Eye 5: N |
Eye 5: I<50 |
Eye 6: DE |
Eye 6: C I |
Eye 6: CI / I 50 |
Eye 6: E/CI |
Eye 6: N |
Eye 7: C |
Eye 7: N |
Eye 7: C / I < 10 |
Eye 7: C |
Eye 7: CI |
Eye 8: C I |
Eye 8: N |
Eye 8: C |
Eye 8: N |
Eye 8: I< 25 |
Eye 9: N |
Eye 9: CI |
Eye 9: N |
Eye 9: C |
Eye 9: I< 25 |
Eye 10: N |
Eye 10: DE |
Eye 10: C |
Eye 10: D/I<10 |
Eye 10: I<50 |
Table 2 Number of eyes description and type of injury seen after intense pulsed light procedure with different power and pulse duration (groups 1-5)
N→ normal / no injury; CI→ lower keratitis; DE→ desepitheliazation; C→ cataract
The types of injuries that occurred post-procedure in each group are shown in Table 2. The different changes in different groups are displayed in Graphic 2.
Graphic 2
Distribution of degrees of injury among the five study groups. It was observed that the groups 1, 3, 4 and 5 showed similar results to the degree of ocular adverse effect and in Group 2 there were more eyes without injury (normal) in the evaluation of post-procedure slit lamp (Graphic 2). The lower keratitis was observed in highest amount in groups 1 and 2 (2 affected eyes) which used lower energies, 7J and 5ms pulse duration and energy of 9J and 12ms pulse duration, respectively. One eye of group 5, power 12J and 34ms pulse duration was affected with keratitis. Groups 3 and 4 did not show this change. The de-epitheliazation occurred in one eye in groups 1, 3, 4 and 5, and in group 2, power 9J and 12 ms pulse duration, occurred in 2 eyes.
The iris lesion was observed more significantly in group 5, 12J energy and 34 ms pulse duration, with 5 cases. Iris involvement also occurred in groups 3 and 4, and in group 3 were affected three eyes and in Group 4 were affected two eyes. The iris lesion occurred in the eyes treated with higher power and increased pulse duration. The occurrence of cataracts occurred in groups 1, 3 and 4, and who had more lesions were groups 1 and 4 (4 eyes), who used energy 7J and 5ms pulse duration and energy of 11J and 26 ms pulse duration, respectively. This prospective experimental study was designed to evaluate the effects of the application of Intense Pulsed Light in porcine eyes in different treatment modalities. The Intense Pulsed Light to be applied is absorbed by the target tissue photoreceptors components, chromophores, which convert light energy into heat through the absorption.3 The chromophores are4:
This study demonstrated that the application of intense pulsed light close to the eyes leads to a decrease corneal thickness in ex vivo porcine eyes, and the decrease is not progressive and not dependent on the energy and pulse duration used in Intense Pulsed Light. Group 1, which was used 7J energy and 5ms pulse, showed no decrease in thickness, and the other groups that used energy from 9J and pulses from 12ms, showed a decrease. Some hypotheses can be raised to explain the reduction phenomenon of corneal thickness, such as: a) Protein denaturation occurred in the cornea. Denaturation may occur mainly in the stroma, which represents 90% of the corneal thickness. The stroma has an extracellular proteoglycans matrix (glycosaminoglycans) and 10 types of collagen, the most important being types I, II, V and VI. IPL denaturing molecules act through the increase in temperature in region.5 b) Capture of light waves by the water present in the cornea. This funding can cause corneal dehydration. About 2/3 of the corneal thickness is water. As stated above, if a wavelength greater than 1200nm is used, this can result in capture and posterior reduce of cornea thickness.
Another point analyzed in this study was the injury degree caused by the application of Intense Pulsed Light and the results showed that the configuration used in group 2, power 9J and 12 ms pulse duration, was that caused less damage, and the other groups were not statistically different from each other.
The lower keratitis, which was observed in groups 1, 2 and 5, can be explained by the traumatic effect of the IPL can cause simulating the damage caused by UV light. The occurrence of de-epithelization in all groups probably occurred because the thermal effect of IPL on the corneal epithelium. The iris lesion observed in Groups 3, 4 and 5, can be explained by the iris pigmentation. The iris has a large amount of pigment and absorbs wide range of wavelengths (range 400-750nm), which makes it an extremely vulnerable structure to IPL.6 The iris injuries are the most reported in studies.
The crystalline lens is exclusively epithelial tissue. The primary function of the crystalline lens is transparency. It’s primary constitution is protein, 35%. The persistence of transparency is due to regular and uniform arrangement of all molecular and cellular structures. The crystalline lens is relatively dehydrated. The crystalline lens opacification can occur due to hydration of intra and intercellular fibers, pigments deposition, variations of the configuration of proteins and decreased energy potential on the protein synthesis.7 Cataracts observed in groups 1, 3 and 4, can be explained by the denaturation of the molecules generated by application of IPL. Another hypothesis to be raised is that the Intense Pulsed Light could cause this opacity of the crystalline lens to increase the water in site.
From the observed lesions and formulated hypotheses we can conclude that the application of Intense Pulsed Light close to the eyes in cosmetic procedures or treatment of meibomian gland dysfunction may result in changes in the cornea as lower keratitis and de-epithelization, iris injury and cataracts. The presence of the adverse effect was not correlated in proportion to the power or pulse duration. The intraocular effects such as iris lesions were more evident in treatments with higher powers. Change was observed in corneal thickness with intense pulsed light from 9J and 12 ms. Because of the lesions observed in the evaluation after the procedure we corroborate the recommendation of using scleral lenses, possibly made of stainless steel, to dissipate the energy of the IPL when ophthalmic procedures or esthetic procedure near the eyeball margin.
None.
None.
The authors declare there is no conflict of interests.

©2016 Credidio, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.