Advances in
eISSN: 2377-4290


Case Report Volume 8 Issue 4
Designa tión Medical Director, USA
Correspondence: Claudio Orlich, Designa tión Medical Director, Clinica20/20, Sabana Oeste, frente al Estadio Nacional, USA, Tel (506)88767525
Received: May 03, 2018 | Published: August 13, 2018
Citation: Orlich C. Annular keratectomy assisted by femto second laser: a case report. Adv Ophthalmol Vis Syst. 2018;8(4):248-250. DOI: 10.15406/aovs.2018.08.00314
We present a case of a 30year-old male patient with keratoconus in the right & left eye, without Vogt’s striae or leukoma. Annular keratectomy was performed in the right eye with the Visumax (Carl Zeiss Meditec AG) femtosecond laser using the PK program. UCVA at 9 and 12months after the procedure was 20/100 with MR -3.75 x 040 20/30. ACD reduction of 0.28 mm and flattening of the Keratometry by a mean of 8.3 D of mean were achieved with this procedure. Spherical equivalent improved 10 D, with a stable refraction after individual sutures were removed. Annular keratectomy assisted by femtosecond laser can be an option for patients with central keratoconus, thus reducing the need for a corneal transplant. More cases and future studies are needed to create a nomogram and determine safety and long-term refraction stability. The keratoconus is a multifactorial corneal degeneration. It commonly presents with corneal thinning, irregular astigmatism and poor vision that generally does not improve with glasses and typically requires the use of contact lenses. It appears in pediatric patients, adolescents and young adults and very rarely presents itself in individuals older than 35.1 In developing countries, it is one of the principal indications for a full thickness corneal graft. In these countries, it is generally difficult to obtain tissue, generating long waiting lists for corneal transplants. Fortunately, the number of penetrating keratoplasties for keratoconus has decreased in recent years thanks to earlier detection of the disease and new treatment options. Professor Theo Seiler discovered corneal collagen cross-linking (CXL) at the end of the 1990’s at Dresden Technical University in Germany. The FDA has approved it in the US. It is indicated most in young patients with evidence of progressive keratoconus, the principal purpose of CXL is to avoid progression.2 The intracorneal segments may be very effective in regularizing the cornea and improving the astigmatic component, especially when assisted by the femtosecond laser. However, the spherical component, especially in regards to high degree myopia, is difficult to correct with this technique. Some surgeons combine the use of intracorneal segments with phakic lenses to achieve better UDVA.3 However, if the segments are implanted superficially or when the segments are near to the incision, they can extrude through the anterior corneal surface. In central keratoconus without leukoma or Vogt’s striae, 355° intracorneal segments may be indicated (Keraring, Mediphacos).4 However, in our experience, they remain near to the incision and extrude with greater frequency. For this reason, we reduced the arc to 340°. We do not have enough experience with these shorter segments to make a definitive comment. More than 50years ago, Professor José Ignacio Barraquer demonstrated the law of thickness. Based on this law, there exist two alternatives for flattening the central cornea and correcting myopia, or in this case keratoconus. The first alternative is to augment the peripheral corneal thickness, as the intracorneal segments or lenticule inclusions do in the periphery of the bag created with the femtosecond laser.5 The second alternative is to take out the tissue in the center of the cornea to flatten it.6 Combining the surface ablation with excimer laser (PRK), simultaneously guided by topography and CXL, is called the Athens Protocol. In a very select group of patients, positive results are being reported with keratoconus grade I or II with minor stable refraction at 6 D of spherical equivalent and pachymetry at 400 microns.7 Enrique Graue et al. in Mexico City describe the combination of SMILE and CXL as the “Aztec Protocol” to differentiate it from the Athens Protocol in which SMILE and CXL are combined to treat thwarted keratoconus or irregular corneas, injecting riboflavin inside the bag once the SMILE lens is extracted and applying Ultraviolet A light with a wavelength of 370nm to 3mW/cm2 for 30minutes. Their results suggested that combining SMILE and intrastromal corneal CXL is a promising treatment option for patients for whom conventional laser refractive surgery is contraindicated.8 There are multiple case reports of patients with progressive keratoconus who submitted to SMILE without CXL and it was not a viable alternative.9,10 Some of these proposed techniques are still under investigation and are not appropriate for patients with advanced keratoconus. The semilunar keratectomy or “crescent keratectomy” as described by Dr. José Ignacio Barraquer, has been used for years to improve high astigmatism in patients with pellucid marginal degeneration or in cornea transplants with high astigmatism postoperatively.#ref66 At the moment, this technique can only be performed manually. Its results are not as reproducible and depend on the ability and experience of the surgeon. Recently, Dr. Carriazo published the creation of semilunar and annular resections with a laser. He resumed Dr. Barraquer’s work, but using an excimer laser instead to treat patients with keratoconus with semilunar or annular resections with greater precision. He uses a mask designed for this purpose, making the laser ablation on the mask. He has published his very promising results.11
We present a case of a 30year-old male patient, without significant medical history, with cone-shaped central keratoconus in the right eye (Figure 1) and mild keratoconus in the left eye. OD UDVA was count fingers at one meter and OS 20/40. Refraction was OD -10.75 -0.75 x 010 20/100 and OS -2.25 -1.00 x 030. The patient did not tolerate the refraction in his glasses due to anisometropia and was contact lens intolerant. Therefore, he was only able to see with his left eye. The cornea in his right eye had a mean keratometry of 51.4D and an anterior chamber depth (ACD) of 4.03mm. Both measurements were taken with the Oculus Pentacam. Given the transparency of the cornea and the few therapeutic options in this case in particular, before performing a lamellar keratoplasty, the patient was offered the option to do an annular keratectomy assisted by femtosecond laser, using the Visumax laser (Carl Zeiss Meditec AG). The Visumax laser allows for corneal grafts with software specially designed for keratoplasties. This software allows you to program two side cuts at different incline angles that are able to meet at their internal edge and separate at their external edge, creating a 360° annular ring. First, a side cut is programmed with an inclination of 130° with internal diameter of 6.50mm and external diameter of 7.69mm. Next, a second side cut is programmed with an inclination of 70° with internal diameter of 6.50mm and external diameter of 6.72mm. Both side cuts were planned at 85% depth of the thinnest pachymetry where the treatment would be applied at 490 microns (Figure 2). In this case, it was decided to leave an anterior separation close to one millimeter between both side cuts. In oversized donor grafts, corneal curvature is significantly steeper than with same-sized grafts.12 In this case, we are looking for the opposite effect, flattening the cornea close to 10D. Once the first side cut has been made, the equipment suction is released. At this point, it is necessary to make a new docking, changing the interface to create the second side cut. It is critical to mark the corneal apex with a sterile felt-tip pen (Figure 3). It is convenient to perform paracentesis and to decompress the anterior chamber to decrease the distance between the edges of the keratectomy with the sutures. Suture separate points with 10 Nylon and make a continuous suture posteriorly. The objective is to leave separate points selectively and to leave the continuous suture as support for adequate healing (Figure 4). The procedure was carried out with topical anesthesia. Topical antibiotics and steroids were used during the first weeks after surgery to avoid infection and control inflammation, but unlike a corneal graft, after two weeks the patient are able to stop taking these medications and switch to using only lubricating eye drops. Adverse effects did not present postoperatively. The separate sutures were removed between four to six months after surgery. Sutures were removed selectively guided by the topography. The UCVA at 9months was 20/100 with CDVA 20/30 (+0.75 -3.75 x 040) 20. The patient was given a prescription for glasses OD +0.75 -3.75x040 OD and OS -2.50 -0.75 x 040. With this refraction, the patient was able to see 20/30 in each eye individually and was able to function binocularly. It was possible to decrease the mean keratometry from 51.4D to 43.1 D for a reduction of 8.3D. The anterior chamber depth decreased from 4.03mm to 3.75mm for a decrease of 0.28mm (Figure 5).
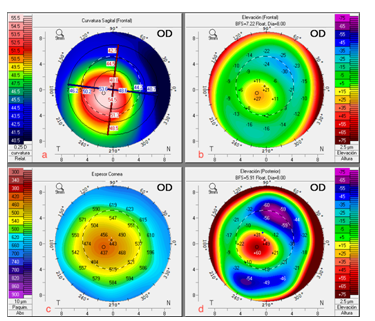
Figure 1 A) Pentacam right eye with central keratoconus. (clockwise, starting with top left image), B) Elevation of the anterior surface, C) Pachymetry map, D) Elevation of the posterior surface.
This is the first reported case of an annular keratectomy performed with the VISUMAX laser. The femtosecond laser may be used as a high precision scalpel to perform an annular keratectomy with very exact dimensions that are impossible to achieve manually. The results of this case motivate us to resume the work begun by José Ignacio Barraquer6,13,14 using currently available tools, especially the femtosecond laser. The annular keratectomy assisted by femtosecond laser may be a viable option to improve corneal curvature and visual acuity in patients with central keratoconus.
None.
Author declares that there is no conflict of interest.
declares that there is no conflict of interest.

©2018 Orlich. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.