Advances in
eISSN: 2377-4290


Case Report Volume 3 Issue 2
Vanderbilt Eye Institute, USA
Correspondence: Karen M Joos, Vanderbilt Eye Institute, 2311 Pierce Avenue Nashville, TN 37232 United States of America, Tel 615-936-1957, Fax 615-936-1540
Received: October 29, 2015 | Published: November 5, 2015
Citation: Ling JD, Joos KM. A successful early postoperative shunt plate erosion repair-case report. Adv Ophthalmol Vis Syst. 2015;3(2):265-266. DOI: 10.15406/aovs.2015.03.00082
An aqueous drainage shunt is a surgical option for refractory glaucoma. Conjunctival erosion over a shunt plate is a complication that frequently is recalcitrant to repair and requires explantation. This case illustrates a successful revision of an early postoperative shunt plate exposure repaired with a scleral patch graft with conjunctival repositioning as well as intensive medical immuno modulator therapy in a uveitic eye with glaucoma.
Keywords: shunt plate erosion, shunt plate revision, uveitic glaucoma, tacrolimus, cyclosporine, scleral patch graft
cm, centimeter; HPF, high power field; mg, milligram; mm Hg, millimeters of mercury
An aqueous drainage shunt is a standard option for refractory glaucoma. Erosion of a portion of the implant through conjunctiva places the eye at risk for endophthalmitis. Aqueous shunt tube erosions are routinely repaired,1 whereas plate erosions are more problematic and often require explantation.1 We report a case of successful revision of an early postoperative shunt plate exposure in a uveitic eye with glaucoma.
A Caucasian male in his mid-sixties presented with bilateral scleral buckles and uncontrolled steroid-dependent chronic anterior uveitic glaucoma despite maximal medical therapy in the right eye noted after removal of silicone oil. The chronic uveitis was noted by the referring physician after removal of the silicone oil more than 1year prior to this evaluation. He had a history of high myopia with retinal detachments in both eyes within 1year following cataract surgery. Besides scleral buckling, his eyes had undergone pars plana vitrectomy with retinotomy, membrane peeling and silicone oil placement with subsequent silicone oil removal in the right eye only. Visual acuity was 20/25, intraocular pressure was 23mmHg, visual fields demonstrated a progressive superior arcuate defect, and optic nerve examination showed a 0.85 cup-to-disc ratio in the right eye. Visual acuity was 20/400 and intraocular pressure was 16mmHg in the left eye following the retinal re-attachments. A 250-mm Baerveldt shunt (Abbott Medical Optics, Santa Ana, CA) was placed in the superotemporal quadrant over the muscles and sutured to the buckle. Extensive undermining was done to ensure no tissue tension was present. The shunt was well-covered on postoperative day 1. On postoperative day 5, a 5-mm-diameter circular exposure over his shunt plate was noted, although the distal tube was covered (Figure 1).
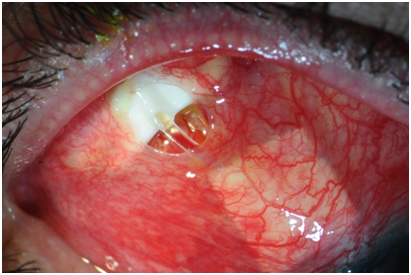
Figure 1 Exposed Baerveldt tube shunt on postoperative day 5. A Baerveldt tube shunt examined on postoperative day 5 had conjunctival erosion overlying the plate and proximal tube while the distal tissue overlying the tube was intact. The conjunctiva was extremely injected.
The patient denied eye rubbing. A revision was performed that day with a 180-degree limbal peritomy and tissue undermining. Then a scleral graft (0.5x0.8cm, Tutoplast, RTI Biologics, FL) was placed parallel and beveled against the plate ridge, thus also covering the proximal tube exposure. The conjunctiva was draped temporally to position the disrupted conjunctiva away from the shunt with closure of the hole and the peritomy with 8-0 Vicryl sutures. Postoperatively, the eye was managed with prednisolone acetate, 1% eight times daily gradually tapered over months to current topical steroid therapy, oral prednisone 40mg daily tapered off over 2weeks, doxycycline 100mg twice daily for its anti-metalloproteinase action discontinued after 5months, tacrolimus ophthalmic ointment, 0.03% three times daily tapered off over 9weeks, and cyclosporine A, 1% in olive oil twice daily tapered off over 7weeks to reduce surface inflammation. The conjunctival injection resolved in 1.5months, and the anterior chamber inflammation gradually improved over the month postoperative period, while the tube shunt remained covered.
At 4 months after surgery, the conjunctiva and anterior chamber remained quiet. The intraocular pressure initially ranged 22-27mmHg during the early postoperative period while on 3 glaucoma medications. After the tube opened 2months following surgery, the intraocular pressure remained between 10 and 15mmHg at each visit over the next 10months while on 2 topical glaucoma medications, and then remained between 10 and 15mmHg over the past 3years while on 1 topical glaucoma medication. The patient had one mild anterior chamber inflammatory flare episode as evidenced by trace conjunctival injection and rare anterior chamber cells (2/hpf) three years after placement of the tube shunt because he discontinued his anti-inflammatory drop. It resolved with resumption of loteprednol 0.5% every other day. Although the scleral patch over the plate and most of the original tube scleral patch dissolved postoperatively, shunt exposure has not recurred for the past 4years (Figure 2) with IOP 13mmHg on timolol maleate, 0.5% twice daily and loteprednol, 0.5% every other day at his last examination. Humphrey visual fields 30-2 were performed every 6months and remained stable throughout the four years of follow-up. The optic disc appearance in the right eye remained stable with a cup-to-disc ratio of 0.85 over the four years.
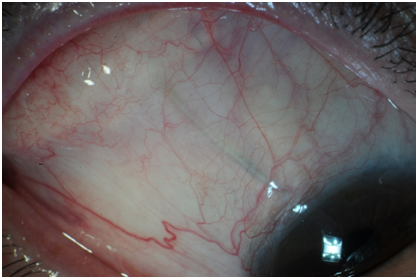
Figure 2 Baerveldt shunt appearance 4 years after revision. Four years after shunt plate revision and supplementation with immunomodulators, the shunt remains well covered. The plate scleral patch and most of the original tube scleral patch melted during the postoperative period. A small piece remains (arrow).
The literature regarding exposed shunt revision techniques generally discusses distal tube exposures.1–4 Simple closure of the exposure is inadequate, and a collagenous human tissue graft of sclera, pericardium, split-thickness cornea, or buccal membrane is placed over the tube and under the transposed intact or repaired Tenon’s and conjunctival layers.1–4 Very few report on shunt plate exposure repair.1,2 Published literature describing revisions during the postoperative period is also limited.3 The complication rate can be high with 45% of tube and 29% of plate erosion repairs requiring additional surgery, and 19% of shunts requiring explantation in one case series.2 Plate exposure treatment reports are limited with a high explantation rate.1,2 Despite being covered with buccal membrane, 1 of 2 exposed plates required removal.1
The patient with chronic uveitis presented with early postoperative plate erosion in the setting of increased conjunctival inflammation postoperatively. A mechanical contribution is also possible as reported in later shunt erosions.3,4 Uveitis was reported to not significantly increase the chronic risk for shunt exposure.5 However, early tube erosion in an inflamed eye was previously described.3 The patch graft was positioned bevel and parallel to the shunt ridge as well as covered the adjacent shunt tube to reduce mechanical forces upon the transposed conjunctiva. The size was large enough to entirely cover the exposed portions. As in the original shunt placement, the conjunctiva was undermined widely to avoid erosion from traction. Although use of steroid to treat ocular inflammation can be complicated with elevated intraocular pressure; it is also important for preventing blockage of the shunt drainage due to inflammatory substances as well as reducing fibrosis in the sub-Tenon space. Careful follow up is essential to achieve this balance. The adjunctive use of steroid-sparing agents may help avoid an intraocular pressure spike, and reduce inflammation by other pathways.
Tacrolimus and cyclosporine A are immunomodulators that block T-cell activation by inhibiting calcineurin. Both are used as treatment for Thygeson’s superficial punctate keratitis, graft vs. host disease, Sjogren’s syndrome, and other severe ocular surface inflammations.6 We report use of these immunomodulators and steroids as adjunctive therapy to reduce marked surface inflammation in a case of successful repair of early shunt plate erosion. Subsequent consultation with a uveitis specialist attributed the monocular chronic anterior uveitis to the past multiple surgical procedures in that eye with no evidence of posterior uveitis, autoimmune disease, or systemic inflammation. Topical low-dose steroid has prevented reoccurrence of flares.
Early erosion over a glaucoma shunt plate may be repaired by immediately covering the exposed implant with a collagenous human tissue graft, closing and transposing the eroded conjunctiva away from the shunt, and aggressively controlling the ocular inflammation.
Both authors had full access to all of the data in the observation and take responsibility for the integrity of the data and the accuracy of the data.
None for both authors, supported by an unrestricted departmental grant from Research to Prevent Blindness, N.Y. to the Vanderbilt Eye Institute (funding only).
None.

©2015 Ling, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.