Advances in
eISSN: 2377-4290


A 52-year-old man with a history of multiple myeloma presented with unilateral loss of vision and evidence of infiltrative optic neuropathy as the sole manifestation of diffuse myelomatous meningitis. He received systemic and intrathecal chemotherapy along with radiation, and did not develop any additional neurologic deficits. The optic neuropathy in this case was thought to be due to infiltration of the optic nerve and meninges by plasma cells. In spite of extensive CNS involvement, including other cranial nerves, the only clinical symptom of myelomatous meningitis was decreased vision in one eye.
Myelomatous meningitis is a rare complication of multiple myeloma and is seen in 1.1% of patients with multiple myeloma.1 Optic nerve involvement in multiple myeloma is also exceedingly rare and has been reported in fewer than 20 patients. We report a case of isolated unilateral optic neuropathy due to myelomatous meningitis, which was widespread and involved optic nerves, the optic chiasm, multiple cranial nerves, and the cervical and lumbosacral regions of the spinal cord.
A 52-year-old man with a history of multiple myeloma recently started on bendamustine/bortezomib/dexamethasone therapy one month prior to presentation had noted temporary vision loss in his right eye two weeks prior to presentation. The episode lasted 10minutes and resolved spontaneously. Two weeks later, he again experienced sudden, painless vision loss in the right eye with mild photophobia, which did not resolve. When he presented two days later, he denied any ocular trauma, headache, neck stiffness, nausea, vomiting or focal neurologic symptoms. He had been diagnosed with IgG kappa multiple myeloma five years prior with partial remission after cyclophosphamide/bortezomib/dexamethasone therapy, followed by Velcade, Thalidomide, and Cytoxan. He underwent stem cell transplantation one year after the initial diagnosis and had experienced multiple relapses. Ophthalmologic examination at presentation revealed no light perception (NLP) in the right eye and best corrected visual acuity was 20/25 in the left eye, with a relative afferent pupillary defect in the right eye. There was florid edema of the right optic disc with flame-shaped hemorrhages. We also found multiple cotton-wool spots, Roth’s spots, and tortuous retinal vessels (Figure 1). His vital signs were stable, with a blood pressure of 101/59. There were no other focal neurologic deficits.
Contrast-enhanced MRI imaging of the brain and spinal cord revealed a dramatic pattern of diffuse meningeal enhancement including around the brainstem and cerebellum, in the basal cisterns, particularly around the optic chiasm and in the interpeduncular cistern, and also throughout the bilateral sylvian cisterns and to the left and right vertex. There was extensive cranial nerve enhancement bilaterally. Matching the right visual deficit, there was marked enhancement and thickening of the meningeal sheath of the right optic nerve and minimal enhancement of the left optic nerve sheath, especially in the vicinity of the optic chiasm. There was also enhancement of the cervical and lumbosacral spinal cord compatible with metastatic multiple myeloma and myelomatous meningitis (Figure 2).
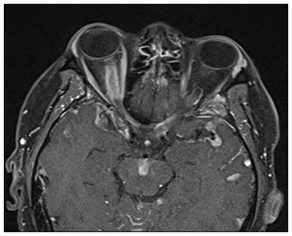
Figure 2 MRI revealed marked diffuse meningitis especially involving the meningeal sheath of the right optic nerve, optic chiasm, and multiple other cranial nerves bilaterally.
CSF analysis revealed elevation of protein (38mg/ml) and WBC count (710/ml). Flow cytometry was consistent with plasma cell myeloma (Figure 3). Fluorescence in situ hybridization (FISH) analysis demonstrated deletion of chromosome 13q in 78.5% of cells, monosomy of chromosome 17 in 87% of cells and gain of 1q in chromosome 71 of 5% of cells. The patient received 12 sessions of whole brain irradiation and intrathecal chemotherapy with methotrexate/cytarabine/hydrocortisone over the course of two weeks. However, there was no improvement of vision in the right eye. Vision in the left eye fluctuated between 20/32 and 20/100 during his two weeks of admission without any disc edema. Vision in the left eye recovered to baseline after completion of treatment. He also did not develop any new neurologic symptoms.
Both, myelomatous meningitis and optic neuropathy are extremely rare manifestations of multiple myeloma. To our knowledge, this is the first report of isolated infiltrative optic neuropathy due to myelomatous meningitis. Other unique features of this case include optic neuropathy being the initial presenting sign of recurrence and the relative sparing of the patient’s other cranial nerves despite the presence of diffuse myelomatous meningitis. The sudden, complete loss of vision may have been caused by optic nerve ischemia, due to hyper viscosity or diffuse infiltration, as imaging did not show a circumscribed mass compressing the optic nerve, but showed thickening of the sheath of both optic nerves. The patient experienced fluctuating left optic nerve compromise during aggressive radiation therapy, with full recovery of his left baseline vision after completion of radiation. The preservation of vision in his left eye may be attributable to the initiation of therapy prior to the onset of symptoms in his left eye.
In general, ocular involvement in multiple myeloma is rare but it can be the first sign of disease. Almost every ocular structure may be involved. Manifestations may include diplopia, proptosis, xanthomatosis, conjunctival and corneal deposits, episcleritis, scleritis, secondary glaucoma, ciliary body cysts, uveal plasymacytoma, hyper viscosity retinopathy, retinal vasculitis, and retinal detachment.2–6 Involvement of the optic nerve has only been described in a few cases.7–9 Findings in these cases included retrobulbar neuritis, infiltration of optic nerves by plasma cells, and optic nerve compression.7,10–14 The most frequent nervous system complications of multiple myeloma are peripheral neuropathy and epidural spinal cord compression, which may be caused by the primary disease and/or the treatment.15 Myelomatous meningitis is a CNS complication found in only 1.1% of patients with multiple myeloma. It usually presents with multiple neurologic signs and symptoms such as altered mental status, cranial nerve deficits, limb weakness, and raised intracranial pressure.1,16–19
Due to the rarity of myelomatous meningitis, there are no randomized clinical trials to guide treatment. Usually a multimodal treatment approach is used, which includes radiation, systemic, and intrathecal chemotherapy. Various combinations of cytarabine, methotrexate, cytosine and thiotepa have been reported to be effective.16,20 This patient’s multiple relapses despite repeated chemotherapy and stem cell transplant, as well as the cytogenetic abnormalities seen on FISH suggest an aggressive form of multiple myeloma. Myelomatous meningitis has also been reported as a sign of leptomeningeal relapse after allografting.16 In such cases, the leptomeningeal involvement is often resistant to intrathecal chemotherapy and irradiation. Patients with myelomatous meningitis may have a good response to treatment initially; however prognosis is poor with an average life expectancy of 8 weeks from onset of neurologic symptoms.18,21 This patient was discharged from the hospital after two weeks of radiation and chemotherapy and did not follow-up with the ophthalmology clinic so his status is unknown.
In multiple myeloma cases, a thorough ophthalmic examination may be helpful at the time of initial diagnosis and at regular intervals thereafter. Although ophthalmologic manifestations of multiple myeloma and myelomatous meningitis are uncommon, they may be the first warning sign of worsening or relapse.
None.
The author declares that there are no conflicts of interest.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.