Advances in
eISSN: 2377-4290


Aim: To determine the significant changes which occur in the corneal parameters, including pachymetry, after corneal collagen cross linking (CXL) by means of Scheimpflug imaging.
Methods: Standard CXL procedure was done for 40 eyes diagnosed as progressive keratoconus (KCN). The following parameters were monitored pre, six months and 1 year post operatively: uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), refractive spherical equivalent (S.E), keratometry1 (K1) and keratometry2 (K2), apex and thinnest point pachymetries, thinnest point coordinates (X,Y) minimum (Min.), maximum (Max.), average (Avg.) pachymetric progression indices, Max. Anterior and posterior elevations. Pentacam (Oculus, Wetzlar, Germany) imaging was used to monitor the corneal parameters of the study. Paired sample T test was used for statistical analysis.
Results: Following parameters of the study did not show significant changes after CXL: UCVA: (P= 0.65), BCVA: (P= 0.076), S.E: (P= 0.343), Thinnest point X coordinate: (P=0.545), Thinnest point Y coordinate: (P= 0.144), Max. Anterior elevation (P= 0.508) and the following parameters showed significant changes: K1: (P= 0.001), K2: (P= 0.015), Apex pachymerty: (P <0.001), Thinnest point pachymetry: (P <0.001), Max. Post. Elevation: (P= 0.001) and all (Max., Min., Avg.) pachymetric progression indices: (P <0.001 for all 3). The most significant changes occurred in pachymetric progression indices.
Conclusion: We could show six months to 1 year after CXL procedure, the corneal thickness is lower than its baseline and keratometric changes have been settled during this period. UCVA, BCVA have not been changed significantly and the pachymetric progression indices are the most significant parameters to have changes, when evaluating them by Pentacam. Validity of Scheimpflug imaging of the corneas after CXL should be determined in further studies.
Keywords: keratoconus, crosslinking, pachymetry
CXL, collagen cross linking; KCN, keratoconus; UCVA, uncorrected visual acuity; BCVA, best corrected visual acuity; SE, spherical equivalent; K1, keratometry1; K2, keratometry2; Min, minimum; Max, maximum; Avg, average; DM, diabetes mellitus; CS, contrast sensitivity
Keratoconus is a degenerative, non inflammatory, progressive bilateral thinning of the cornea. It represents a disorder of the corneal stroma associated with decreased biomechanical strength of the tissue, which is thought to be caused by diminished intra-and interfibrillar cross-links of the collagen fibers.1 It is characterized by stromal thinning leading to secondary conical ectasia. The manifestations of the disease vary from slight irregular astigmatism to visual impairment secondary to stromal scarring. Progressive distortion and bowing of the cornea results in optical aberrations and in some cases an inability to achieve good functional vision. Often, this has a negative impact on the quality of life.2 Treatment options for early keratoconus include correction of the refractive error by noninvasive therapies such as spectacles or contact lenses. Spectacles and RGPs do not halt progression of the disorder but merely improve visual acuity. ICRS implantation is a minimally invasive surgical therapy, used as an effort to flatten the central steep cornea when spectacles and contact lenses fail to improve visual acuity. It may cause complications such as extrusion of segments, anterior or posterior perforations, shallow or uneven placement of the segments, introduction of epithelial cells into the channel and infection.3,4 DALK and PKP are more invasive surgical therapies indicated for more advanced keratoconus (10% to 25% of cases).
These procedures carry major risks such as endophthalmitis, graft infection, rejection, suture problems and high corneal astigmatism.5,6 Corneal collagen cross-linking (CXL) treatment of progressive keratoconus was first introduced by Wollensak et al.7 in 2003. The CXL technique uses riboflavin and UV-A irradiation to increase corneal rigidity and inhibit the progression of the ectasia.7-9 During the last decade, the CXL technique has gained wide spread successful use in the treatment of ectasias, and many studies reported to halt progression and stabilize the disease a reduction in corneal curvature and an improvement in visual acuity.10-16 The purpose of this study was to evaluate the changes which occur in the optical properties of the corneas as indicated by UCVA and BCVA measurements, and to examine the effects of the CXL procedure on the keratometric and pachymetric parameters of the cornea before, and 6 months after crosslinking.
The study was conducted according to the principles of the Declaration of Helsinki, and Institutional Review Board/Ethics Committee of the Tabriz University of Medical Sciences approval was obtained. All patients provided informed consent. Forty eyes of 31 patients (14 male and 17 female) with progressive keratoconus were enrolled in this non randomized prospective study who were documented as having progressive keratoconus when they had one or more of the following changes over 6 months. Increase of 0.50 diopter (D) or more in the steepest keratometry (Km), an increase of 0.25 diopter (D) or more in the manifest spherical equivalent or an increase of 0.5 diopter (D) or more in manifest cylinder for patients aging over 20. For the patients under the age of 20, no such documentation was made and they were considered progressive solely on the basis of their age as the major determinant of keratoconus progression.
The inclusion criteria were:
Each patient underwent corneal collagen cross-linking with riboflavin and UV-A in the keratoconus eye (procedure described in the section Cross-linking Procedure). The following examinations were performed pre-and postoperatively at 6 and 12 months: distance uncorrected and best-corrected visual acuities (UCVA and BCVA, respectively), manifest refraction, biomicroscopic examination, endothelial cell count (noncontact specular microscope; Topcon, Corp, Tokyo, Japan), maximum and minimum keramometry measurements (Keratron Scout; OPTIKON 2000, Rome, Italy), CCT (Ophthasonic A-Scan/Pachometer III; Accutome, Malvern, PA), corneal thickness at the thinnest point, apex of the keratoconus and pupil center, anterior and posterior elevation values (Pentacam rotating Scheimpflug; Oculus Optikgerate GmbH). The Pelli-Robson test was used to evaluate contrast sensitivity (CS). Patients used trial frames with the optimal refractive correction, and Pelli-Robson letter CS was measured at 1 m with the chart luminance of 85 cd/m2. Each eye was tested separately using different charts. The test was scored using the modified method of letter-by-letter scoring, in which each correctly read letter scores one point on a scale from 0 to 48, and the result was converted to units of log CS.15
Cross-linking procedure
Topical anesthesia was achieved by instilling 1 drop of tetracaine 0.5% (Alcaine; Alcon Laboratories) into the eye every 5 minutes for 3 doses immediately before the procedure. After positioning the patient under the operating microscope, routine sterile measures were taken in the OR and a lid speculum was inserted and the central 9 mm of the corneal epithelium was removed with a blunt spatula (Asico AE2766). The riboflavin solution (riboflavin 0.1% in 20% dextran, MediocrossTM 3.0ml) was instilled every 3 minutes for 30 minutes until the riboflavin penetrated the cornea as shown by a yellow coloration in the anterior chamber on slit-lamp biomicroscopy. The required irradiance from the UV lamp (UV-X illumination system, version 1000; IROC AG, Zurich, Switzerland) of 3.0mW/cm2 was calibrated using a UV-A meter (Laser Mate-Q; LASER2000, Wessling, Germany) at a working distance of 5 cm. The UV radiation was then focused on the apex of the cornea at a distance of 5 cm for a total of 30 minutes, providing radiant energy of 3.0±0.3 mW/cm2. During the UV-A administration, the riboflavin solution was applied to the cornea every 5minutes or sooner if the corneal surface appeared visibly dry. At the end of the procedure, the eye irrigated and a bandage soft contact lens (Schalkons of Clear+0.5 D) put on the cornea after instilling one drop of chloramphenicol. The patient discharged and ordered to use chloramphenicol and betamethasone drops separately q6h and to be followed every 2 days until full epithelialization. The antibiotic drop continued one week and betamethasone drop continued 3 weeks post operatively. The bandage contact lens was removed on postoperative day 5, at which point slit lamp biomicroscopic examination was performed to confirm the presence of complete corneal reepithelialisation.15-17 Routine examinations were performed at 6, and 12 months postoperatively as described previously.
Statistical analysis
Statistical analysis was performed using PASS statistics software (version 17, SPSS, INC). A P-value less than 0.05 were considered to be of significance. Preoperative and postoperative parameters within each group were compared using the paired t test (for normally distributed data), or nonparametric Wilcoxon signed rank test (data not normally distributed). Preoperative and postoperative parameters between the2 groups were compared using the unpaired t test (data normally distributed), or nonparametric Mann-Whitney test (data not normally distributed).
Demographics
40 eyes of 31 patients were enrolled into this study. Out of the 31 patients, 13 were female and 18 were male. The mean age of the patients was 18.5±4.2 (SD) (range 10-35).
Visual acuity
The mean preoperative UCVA was 0.59±0.37 logarithm of the minimum angle of resolution (logMAR) (mean±SD). Postoperative UCVA at 6, and 12 months was 0.52±0.34 and 0.51±0. 32log MAR respectively. Pre-and postoperative UCVA differences were not statistically significant at 6 months (P=0.65) and 12 months (P =0.61). The mean preoperative BCVA was 0.25±0.04 (SD) log MAR. The mean postoperative BCVA at 6 month was 0.20±0.03 (SD) log MAR, whereas at 12 months postoperatively, the mean BCVAs were 0.20±0.03 (SD) log MAR. The differences between pre-and postoperative BCVA values were not statistically significant (P =0.076 for 6 months and P=0.073 for 12 months).
Refraction
There were no significant differences between the pre-and postoperative mean spherical equivalent at 6 and 12 months (-4.06±2.75, -3.91±2.55 and -3.83±2.61 respectively; P=0.426).
Keratometry
The mean maximum and minimum keratometry measurements (K1 and K2) at 6 and 12 months postoperative compared with preoperative levels have demonstrated in (Table 1).
Mean |
Pvalue |
|||
Preoperative |
6Months, Postop |
12Months, Postop |
||
K1 |
45.20±2.92 |
44.48±3.08 |
44.40±3.00 |
0.001 |
K2 |
49.43±4.22 |
48.95±4.42 |
48.84±3.86 |
0.015 |
Table 1 Preoperative and postoperative keratometry values
Pentacam scheimpflug analysis
Mean corneal thickness values measured using Scheimpflug analysis with the Pentacam at the thinnest point and corneal apex are shown in Table 2. The mean reductions at the thinnest point and apex of the cornea at 6 and12 months postoperatively compared with preoperative values were all of which were statistically significant (Table 3). The changes in the thinnest point location (X, Y coordinates) were not statistically significant (P=0.54, P=0.14 respectively). All of the 3 pachymetric progression indices had significant changes (P<0.001 for each). (Table 4) shows the mean pre-and postoperative anterior and posterior elevation values of the cornea. The change in the Max anterior elevation point, was not significant (P=0.50) but the same, for the posterior elevation point was significant (P=0.001). There was correlation between the apex pachymetry and Max PI, r =0.36 (Figure 1).
Mean±SD |
P value |
||||
Preop |
Postop 6m |
Postop 12m |
|||
TPP |
469.25±31.65 |
421.53±50.22 |
429.23±52.29 |
<0.001 |
|
CCT |
481.95±29.65 |
437.73±45.3 |
444.22±50.00 |
<0.001 |
|
TPL |
X |
-0.51±0.24 |
-0.54±0.27 |
-0.53±0.26 |
0.545 |
Y |
-0.45±0.23 |
-0.40±0.25 |
-0.40±0.28 |
0.144 |
|
Table 2 Pre and postoperative corneal thickness and thinnest point location
Mean±SD |
P value |
||||
Preop |
Postop 6m |
Postop 12m |
|||
PI |
Avg |
1.8 1 ±0.45 |
2.78±1.27 |
2.60±1.28 |
<0.001 |
Max |
2.53±0.84 |
3.66±1.60 |
3.65±1.66 |
<0.001 |
|
Min |
1.41±0.42 |
2.15±1.03 |
2.19±1.00 |
<0.001 |
|
Table 3 Pre and postoperative pachymetric progression indices
Mean |
P value |
|||
Preop |
Postop 6m |
Postop 12m |
||
AE |
24.00±11.78 |
24.75±14.41 |
24.70±14.39 |
0.508 |
PE |
49.13±22.23 |
57.93±29.26 |
58.01±29.28 |
0.001 |
Table 4 Pre and postoperative anterior and posterior elevation indices
Contrast sensitivity test
The mean contrast sensitivity (CS) at baseline for all 40keratoconic eyes was 1.48±0.17 log CS. In eyes undergoing CXL, CS improved from a mean of 1.52±0.16 log CS to 1.68±0.8 log CS (P=0.001) over 1year of follow-up.
This study evaluated refractive and topographic outcomes for patients undergoing riboflavin/UV-A cross-linking treatment for keratoconus. In this study the spherical equivalent value did not demonstrate significant decrease at 1 year postoperatively. In Henriquez et al.16 study the spherical equivalent value was reduced by a mean of 2.25 D at 1 year postoperatively. Similar refractive results after riboflavin/UV-A cross-linking were reported by Caporossi et al.2 who found a decrease in the mean spherical equivalent value of 2.21 D at 3 months postoperatively, and by Wollensak et al.7,8,18 who reported that the spherical equivalent improved significantly by an average of 1.14 D at 6 months postoperatively. We found, the CXL procedure to cause flattening effect of around 0.72 D in K1 reading and about 0.75 D in K2 reading as measured by Pentacam (Simulated K’S) in 1 year period. It has been shown that the flattening process may continue for years.17,18
Our keratometric findings are in accordance with Henriquez et al.16 who found significant reductions in the mean maximum and minimum keratometry values at 1 year postoperatively of 2.66 and 1.61 D, respectively. Wollensak et al.7,8,18 reported similar results, with a postoperative average reduction of the mean keratometry measurement of 2.01 D. Caporossi et al.2 similarly reported a reduction in the mean keratometry reading of 2.1 D in the central 3.0 mm. There is little evidence in the literature defining what constitutes normal or abnormal anterior or posterior corneal elevation values. Studies using Pentacam however, do agree that anterior and posterior corneal curvatures of the cornea are different in normal and keratoconus eyes, with larger curvature values in eyes with keratoconus.19 Grewal et al.20 did not observe a significant change in anterior or posterior corneal elevation point’s values when they examined their patients by Pentacam pre and post CXL procedure in a one year period. We found the anterior elevation point value not to change significantly (P=0.508), but the posterior elevation point value to change (be increased) significantly (P=0.001) although both of these parameters had large standard deviation values pre and post CXL procedure (Figure 2).
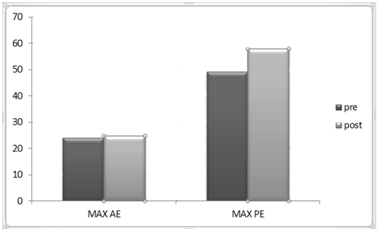
Figure 2 Shows mean changes occurring in the Max. Anterior and the Max. Posterior elevation points pre and 6 months post operatively.
The elevation data gained by optical devices such as Pentacam may not be reliable after the CXL procedure. The corneal haze and the demarcation line present after the procedure may disturb data acquisition by the instrument as Koller et al.21,22 have shown. These data acquisition artifacts may also affect pachymetric measurements as well. Besides, ultrasonic pachymetry, in these instances, is not absolutely valid as thickness measurements are questionable in moderate and severe keratoconus which has been shown in various studies.21,23,24 We found significant changes in all pachymetric parameters including the apex, the thinnest point and all of the 3 indices of pachymetric progression (Min. Max. Avg.) values postoperatively (Figure 3&4). The reduction in some pachymetric values at 6 months post CXL have also been shown in Greenstein et al.25 study using Pentacam for their measurements. It is important to have pretreatment CCT of at least 450µ including the epithelium, which is approximately 50-µ.2,7 Wollensak et al.7 suggested that in human corneas with a CCT less than 400µ, the cytotoxic endothelial UV-A irradiance of 0.36mW/cm2 is reached using the standard treatment surface irradiance of 3.0 mW/cm2. In our study, all the subjects had CCT greater than or equal to 450µ and we did not encounter any serious complications.
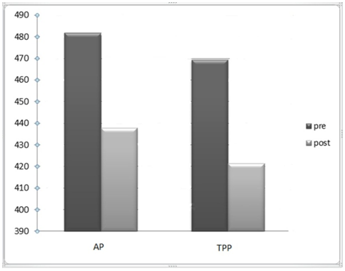
Figure 3 Shows mean changes in the apex and the thinnest point pachymetries pre and 1 year postoperatively.
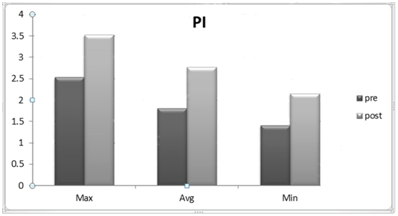
Figure 4 Demonstrating changes in the mean Max. Avg. Min. pachymetric progression indices pre and 1year postoperatively.
There is no extensive study of the pachymetric progression indices after CXL procedure in the literature. We evaluated them in our study and found significant changes in all of the 3 indices (Min, Max and Avg) (P<0.001, for each of the indices). Indeed, the indices increased in their values although they had large SD measurements at 6 months post CXL. The changes which occur in the pachymetric progression indices after CXL procedure require more studies and we consider them, to be the most significant changes which occur after CXL. As mentioned previously, the artifact effect of the Pentacam in acquiring these kinds of data should be seriously appreciated when analyzing them. The correlation between, the Max PI and the apex pachymetry, showed moderate significance (r=0.36) (Figure 5). In other words the apex thinning after CXL predicted abnormally high values for the Max PI.
Evaluation of thinnest point coordinates (X, Y) with assumption of their displacement as an indirect measure of corneal reshapping after CXL was done in our study. They had no significant change in their values post operatively. We believe that their insignificant change is due to minimal change in the shape of the cornea after CXL. This finding is in favor of Koller et al.22 study. Further studies are required on this matter. The improvements in visual acuity, refractive error, and keratometry readings were found to occur progressively over the postoperative follow-up period, suggesting that a longer follow-up is required to achieve the total functional and anatomic effects of the cross-linking treatment and to obtain stable refractive and keratometric values and this is one of important limitations of this study. Once these results are achieved, complementary refractive treatment options such as intrastromal corneal rings may be considered.
In summary, we could show six months to 1 year after CXL procedure, the corneal thickness is lower than its base line and keratometric changes have been settled during this period. UCVA, BCVA have not been changed significantly and the pachymetric progression indices are the most significant parameters to have changes, when evaluating them by Pentacam.
This study was supported by the vice-chancellor of the research center of Tabriz University of medical sciences, Tabriz, Iran through a grant. The authors would like to thank patients for participation in the study.
Author declares that there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.