Advances in
eISSN: 2377-4290


Research Article Volume 4 Issue 2
1Ophthalmology, Voronezh NN Burdenko, State Medical University, Russian Federation
2Department of Biomedical Engineering, University of Arizona, USA
3Division of Physics, Mathematics and Astronomy, California Institute of Technology, USA
4Fyodorov Eye Microsurgery, Federal State Institution, Russian Federation
Correspondence: Maria Kovalevskaya, Ophthalmology, Voronezh NN Burdenko State Medical University, Voronezh Russian Federation
Received: January 25, 2016 | Published: March 22, 2016
Citation: Kovalevskaya M, Milyutkina S, Fink W, et al. 3D-CTAG testing of functional and structural changes of the Macula. Adv Ophthalmol Vis Syst. 2016;4(2):45-50. DOI: 10.15406/aovs.2016.04.00103
Objective: To enhance the efficiency of diagnosis and treatment of the wet AMD by dynamic evaluation of macular area function.
Methods: 162 patients (244 eyes) were allocated to five groups. Group I (n=92) included patients with dry form of AMD; group II (n=43) consisted of patients with wet form of AMD, group III (n=28) included patients with fibrous scar; group IV (n=31) included patients with diabetic macular edema, group V (n=50) - controls. In addition to the standard procedure all patients underwent 3D-computer threshold Amsler grid test (3D-CTAG), microperimetry, OCT (optical coherent tomography) and fluorescent angiography on indication. The treatment depended on the clinical form of the disease; multivitamins with lutein and zeaxanthin, metabolic agents or inhibitors of vascular endothelial growth factor.
Results: Volume lost relative to hill-of-vision (VLRH) decrease from 0.2 (0, 0.46) of 69300 deg2% to 0% (0; 0) of 69300% deg2% in group Ia and increase from 0.26 (0, 0.49) to 0.37 (0, 0.62) in subgroup Ib, respectively. VLRH decreased from 4.35 (2.95; 6.8)% of 69300 deg2% to 1.77 (1.19; 2.82)% of 69300 deg2% (p <0,01) in the subgroup IIa and from 9.54 (5.44; 11.59) to 6.93 (4.45; 8.39) in the subgroup IIb. VLRH rest the same in group III 20,81 (13,4;29,91) )% of 69300 deg2%. VLRH decreased from 1.2 (0.73; 1.61)% of 69300 deg2% to 0.53 (0, 1.28)% of 69300 deg2% in group 4.
Conclusion: The study developed a new method for differential diagnosis and evaluation of treatment of macular disease by quantifying the central scotomes based on 3D-CTAG. Revealed clinical and functional parallels between changes in 3D-CTAG and the size of CNV corresponded to the change in brightness sensitivity on microperimetry confirmed by OCT and fluorescent angiography. 3D-CTAG rather than microperimetry is recommended as an investigation of choice in patients with low visual acuity (VA less 20/100).
Keywords: age-related macular degeneration, diabetic macular edema, 3d-computer threshold amsler grid test (3d-ctag), ranibizumab
Functional changes in the macula such as blurred vision, distortion of lines, defects in the visual field significantly decrease the quality of life of patients with macular diseases. Age-related macular degeneration (AMD) is the leading cause of blindness in people over 50 in developed countries. According to the World Health Organization 8.7% of the blind in the world lost their sight due to AMD.1,2 The pigment epithelial cell damage and disruption of their interaction with photoreceptors and choriocapillaris play a central role in the pathogenesis of AMD.3 Diabetic macular edema (DME) is the most common cause of visual loss in patients with diabetes mellitus (DM). The incidence of clinically significant macular edema was 20.1% in patients with diabetes type I, 25.4% in patients with type II diabetes when on insulin therapy and 13.9% in patients with ten-year diabetes history without insulin therapy. DME is an accumulation of fluid in the intercellular space of the retina as a result of integrity damage to the internal and then the outer blood-retinal barrier.4
Visual acuity (VA) is still considering as the gold standard of visual testing but Snellen acuity captures less than 0.1% of the visual field and fails to take into account other parameters of vision, such as contrast sensitivity and color vision.5 According to the opinion of many researchers and clinicians visometry should be complemented by other functional methods, such as microperimetry6 which allows to estimate the interrelation of the structure and function in macular disease and to determine the retinal sensitivity damage and gaze fixation changes.7 However, the disadvantage is the long time of the procedure and the patient’s fatigue. Furthermore, patients with visual acuity less than 20/100 can provoke errors in the topographic binding of retinal sensitivity because in 95% of the studies the fixation point does not coincide with the projection of the fovea.8 In addition, patients with visual acuity less than 0,19 brightness sensitivity indexes are not informative as in 95% of procedures the patient’s gaze fixation point does not coincide with the fovea projection.8
Amsler test with black grid on a white background is a screening technique for the diagnosis of functional macular disorders.9 In 2000 Wolfgang Fink and Alfredo Sadun created a 3D-computer threshold Amsler grid test (3D-CTAG) allowing to create a 3D-map of the central visual field which shows the location, length, slope, depth and shape of existing defects.5,10 Since 2012 the Department of Ophthalmology of Voronezh N.N. Burdenko State Medical University has been carrying out a joint research with the University of Southern California Eye Institute and California Institute of Technology to introduce the 3D-CTAG into clinical practice. 3D-CTAG identifies anomalies of vision in 16% of patients with AMD and DME, whereas the traditional Amsler test shows normal results, and 3D-CTAG also enables to make a quantitative assessment of visual disorders.11 The time spent on one eye examination is 4-5 minutes which makes it possible to use 3D-CTAG as a screening method in a large cohort of patients.
The gold standard of wet form of AMD diagnostics is still the fluorescent angiography12 as the sensitivity of fluorescent angiography and OCT in the macular edema diagnosis is 98.7% and 96.1%, respectively.13 Comparative analysis of data obtained by different methods of diagnosis is very important in making the diagnosis and determination of treatment strategies as no single method can give a complete description of the pathological process at the eye bottom. Comparison between 3D-computer threshold Amsler grid test and microperimetry, fluorescent angiography and optical coherent tomography has not been carried out so far. The objective of this study is to enhance the efficiency of diagnosis and treatment of diseases of the retina, as well as the dynamic evaluation of the function of the macula in self-examination. Thus, the tasks to solve are as follows:
Clinical studies have been conducted at the Department of Ophthalmology of Voronezh N.N. Burdenko State Medical University, Voronezh polyclinic #7, Railway Clinical Hospital and S. Fyodorov Eye Microsurgery Federal State Institution, Kaluga Branch since 2013. The study included 162 patients (244 eyes) who were divided into five groups. Group I included 60 patients (92 eyes) with dry form of AMD. The patients of this group were divided into two subgroups: subgroup A was prescribed 1 tablet Vitrum Vision forte 2 times a day, subgroup B was given 1 tablet (0.25 g) Taurine 2 times a day. The observation period was 3 months.
Group II consisted of 35 patients (43 eyes) with different patterns of CNV: classical (23 eyes), occult (6 eyes) and mixed (14 eyes). 9 patients of this group (10 eyes) had intravitreal ranibizumab (1,6±0,7 injections) in their past history. Patients of group II were administered intravitreal ranibizumab in Kaluga Branch of the S. Fyodorov Eye Microsurgery Federal State Institution. The observation period was one month after the injection. Two subgroups of patients were singled out depending on the period of clinical manifestations of wet AMD form. Subgroup II A had such period of less than 6 months, subgroup II B had such period of more than 6 months.
Group III included 25 patients (28 eyes) with fibrous scar. Patients took 1 tablet Vitrum Vision forte 2 times a day. The observation period was one month. Group IV included 20 patients (31 eyes) with diabetic macular edema who underwent intravitreal ranibizumab in Kaluga Branch of the S. Fyodorov Eye Microsurgery Federal State Institution. The observation period was one month. Group V included 25 healthy volunteers (50 eyes) over 45 served as control. 122 women and 40 men have been investigated. The average age of the patients was 71,69±7,98 years old (from 53 to 85 years old). Exclusion criteria were: clinically significant damage to eye optical media transparency, inflammatory diseases of the eye and its appendages, glaucoma and ocular hypertension, surgical and laser ophthalmic intervention during the last 3 months.
All patients underwent standard ophthalmic research and Amsler test, optical coherent tomography (Stratus OCT-3000, Carl Zeiss, Germany) and on the testimony of fluorescent angiography (VISUCAM 500, «Carl Zeiss» Germany). According to the OCT obtained data the height of choroidal neovascularization (CNV), detachment of the neuroepithelium (NED) and retinal edema (mm), the maximum diameter of the pathological focus (mm) and a diameter perpendicular to the plane (mm) were determined. On the basis of those parameters the area of the CNV, NED and edema (mm2), and the amount of CNV, NED and retinal edema (mm3) were calculated.
In addition to the standard procedure all patients underwent 3D-computer threshold Amsler grid test (3D-CTAG)4 assisted by iPad 3, Apple, (USA). 3D-CTAG study conducted by California Polytechnic protocol, used 5 contrast levels defined by calibration and a black grid on a white background. 3D-CTAG criteria were the following: the number of defects; lowest contrast level,%; area defects on different contrast levels deg2; absolute volume lost (AVL) deg2%; volume lost relative to hill-of-vision (VLRH) 69300% of 693000 deg2%, lost area grade (lag)%.
Microperimetry was also performed (fundus microperimetry MAIA, CenterVue, Italy, the field of view of 20° × 20°, 68 points). Microperimetry criteria were the following: the average light sensitivity, dB, brightness sensitivity in the projection of the pathological focus, dB (without hardware assistance), the localization of the fixation point in the range from 1° foveola%. The treatment of patients in clinical groups was administered by indication depending on the clinical form of macula disease: Vitrum Vision Forte (Unipharm, Inc., USA) – multivitamins, the drug for treating and preventing dry form of AMD; Taurine - metabolic and regenerative remedy; sulfur containing amino acid stimulating reparative processes in dystrophic diseases; Ranibizumab (Lucentis, Novartis Pharma AG, USA) –anti-VEGF agent and vascular proliferation blocker in wet form of AMD and DME. Statistical analysis was performed using the statistical software package Statistica 12, Microsoft Office Excel 2007. To estimate the normal distribution the Shapiro-Wilk test was used for comparison of two independent samples - Student’s t test as a parametric method and U-Mann-Whitney test as nonparametric method. Pearson and Spearman coefficients were used to identify the existence of correlations between the two variables.
The study in the 3 clinical groups with a dry, wet and a scar form of AMD showed that functional disorders of retina macular area the progressively increased in accordance with the clinical and morphological changes which is confirmed by visometry, microperimetry and 3D-CTAG see Tables 1 & 2. Best corrected visual acuity (BCVA) in groups of patients vary greatly: in dry AMD patients the values were from 20/63 to 20/20, in wet AMD patients the values were from 20/1000 to 20/25 in the subgroup 2a and the values were from 20/1000 to 20/33 in the subgroup 2b, in patients with fibrous scar the values were from 20/2000 to 20/100, in patients with DME the values were from 20/667 to 20/20 and in the control group the values were from 20/25 to 20/20.
Group, subgroup |
Number of eyes (n) |
Average light threshold, dB |
Localization of the fixation point in 1° from the foveola,% |
|||
|
|
|
Visit 1 |
Visit 2 |
Visit 1 |
Visit 2 |
I.Dry AMD |
IA |
46 |
24,8 (22,8;26,5) |
25,7 (25,2; 28,8)** |
95 (90;99) |
98 (92; 100) |
IB |
46 |
24,8 (21,4; 27,6) |
25,2 (22,2; 27,3) |
94 (89;99) |
94 (89; 98) |
|
II.Wet AMD |
IIA |
19 |
23,1 (21,5;24,2) |
24,7 (23,1; 25,2) |
54 (29; 60) |
79 (60; 92)** |
IIB |
24 |
13,45 (8,45; 19,1) |
15 (11,3; 20,65) |
29 (20,5; 39,5) |
34 (25; 47,2) |
|
III.Fibrous scar |
28 |
1,1 (0,5;2,8) |
1,2 (0,5;2,8) |
27 (17;32) |
27,5 (18,5;28,5) |
|
IV.DME |
31 |
18,35 (16,65;21,05) |
21,15 (18,35;22,13) |
54 (50;57) |
54 (50; 60) |
|
V. Control |
50 |
29,1 (28,8; 30,8) |
30,5 (28,73; 31) |
95 (93;99) |
98 (95;99) |
|
Table 1 Results of microperimetry in patients with macular diseases. Data are presented as M (median) and interquartile range (25%; 75%)
*Differences in comparison with the significant visit 1, p <0,05.
**Differences with significant visit 1, p <0,01.
On microperimetry patients with low visual acuity had eccentric and unstable fixation, so the performance of the brightness sensitivity in wet AMD patients, fibrous scar and DME was evaluated at visual acuity more than 20/100 (Table 1). At the same time the resolution of the 3D-CTAG was 20/2000 as the patient was able to fix eyes on the frame plate and outline their positive scotoma. In wet AMD patients microperimetry identified depression in the projection area of CNV where the light sensitivity are 18.92 (17.36; 20.27) dB compared to 23.1 (21.5; 24.2) dB in average so the light sensitivity in the projection of the pathological focus is more informative than the indicator of the average light sensitivity (Figure 1).
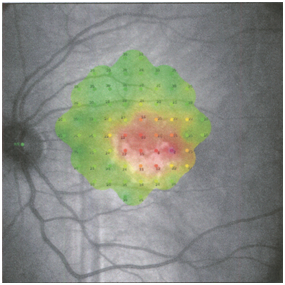
Figure 1 Example visual field defect in wet AMD patient represented as a microperimetry sensitivity map.
The 3D-CTAG detected scotoma in 65.22% of dry AMD patients (30 eyes), and 90% of scotomas were detected on some contrast levels. These changes are corresponded to multiple medium and large single druses and focal destruction of the pigment epithelium without affecting the central hole. In the control group, visual field defects were detected. In patients with wet AMD (group II) following 3D-computer threshold test Amsler 2 types of visual field defects were marked: the fresh edema (subgroup II A) - metamorphopsia in which scotoma area at the 4th contrast level is greater LAG> 100% (Figure 2), and edema period was more than 6 months (sub-group II B) – an absolute scotoma, surrounded by a relative scotoma which manifests itself by the most scotoma area at 0 or 1 contrast level and LAG<100% (Table 2). All patients with neovascular AMD demonstrated leakage from CNV (fluorescent angiography) (Figure 3).

Figure 2 Example visual field defect in wet AMD patient from Figure 1 represented as a 3D surface plot of contrast sensitivity across the tested visual field obtained with 3D-CTAG.
Parameter |
Visit |
Group I dry AMD |
Group II wet AMD |
Group III fibrotic scar (n=17) |
Group IV DME(n=31) |
Group IV controle (n=50) |
||
Number of Defect per Eye |
1 |
1 (0,1) |
1 (0,1) |
1 (1;2) |
1 (1;1) |
1 (1;1) |
2 (2;3) |
0 |
2 |
0 (0,0) |
1 (0,1) |
1 (1;1) |
1 (1;1) |
1 (1;1) |
1 (0;2)** |
0 |
|
Lowest Contrast Level, % |
1 |
7 (5;11) |
8,5 (5;13) |
21 (9;25) |
16,5 (12;25) |
28 (25;36,5) |
9 (6;13) |
4,5 (4;6) |
2 |
5 (4;7)* |
12,5 (5;13)* |
15 (7;19) |
16,5 (12;23) |
27 (25;35) |
8 (7;13) |
4 (3;5,75) |
|
AVL,deg2% |
1 |
136,5 (0;320) |
183 (0;341) |
3012 (2043;4711) |
6606,5 (3770,5; 8032,5) |
14421 (9288,5;20729,5) |
829 (508; 1119) |
0 |
2 |
0 (0;0)** |
254 (0;427)* |
1195 (650; 1456)** |
4495,5 (2567;5813,5) |
14883,5 (8899,5;24037,5) |
280 (0;888)* |
0 |
|
VLRH, % of 69300 deg2% |
1 |
0,2 (0;0,46) |
0,26 (0;0,49) |
4,35 (2,95;6,8) |
9,54 (5,44; 11,59) |
20,81 (13,4;29,91) |
1,2 (0,73; 1,61) |
0 |
2 |
0 (0;0)** |
0,37 (0;0,62)* |
1,77 (1,19; 2,82)** |
6,93 (4,45;8,39)** |
21,48 (12,84;34,69) |
0,53 (0;1,28)* |
0 |
|
LAG, % |
1 |
- |
- |
200 (136,76;376) |
30,57(25,09;40,75) |
74,69 (63,77; 81,22) |
116,67(58;87,51) |
- |
|
2 |
- |
- |
62,57(47,65; 103,21)** |
49,45(25,99; 69,97) |
72,68(63,55; 80,04) |
46 (0;116)** |
- |
Table 2 Dynamics of 3D-CTAG. Data are presented as M (median) and interquartile range (25%; 75%)
*Differences in comparison with the significant visit 1, p <0,05.
**Differences with significant visit 1, p <0,01.
Significant functional impairments in wet form of AMD are connected to the local destruction of the outer blood-retinal barrier and damaged pigment epithelium and photoreceptors in the early stages of CNV onset. Forming an absolute scotoma indicates disease progression and irreversible changes in the retina. Thus, patients with fibrotic scar (group 3) 3D-CTAG revealed cylindrical shape defects with a similar defect area at each contrast level (absolute scotomas). The absence of relative scotomas at low contrast levels is due to the absence of liquid leakage outside the scar which was confirmed by fluorescein angiography.
The results of our study revealed that the steep slopes of the scotoma are not unique to the dry form of AMD, but also for the fibrous scar which significantly expands the data obtained by Robison CD et al.14. Patients with cystic diabetic macular edema, unlike the patients with wet form of AMD dominated metamorphopsia multiple (number of defects per one eye is two (2:3) in group IV, 1 (1:1) in a group 2b, respectively). Scotoma in patients with DME was detected only when having a neuroepithelium detachment accompanied by the long-existing edema. Meanwhile RV Jivrajka et al.,11 found that in DME patients 3D-CTAG can detect multiple defects (defects 3.56±2.96 in 1 eye) which can be explained by the presence of several points of leakage and scotoma having the form of an inverted cone. Smaller functional changes in the DME if compared with the wet” form of AMD are explained by late damage in the outer blood-retinal barrier and pigment epithelium and photoreceptor damage. The parameters of functional tests have correlated. For example, the data analysis of patients with dry form of AMD (group I) revealed a negative correlation between the amount of absolute volume lost on 3D-CTAG, and the average light sensitivity to microperimetry (ρ = -0,63) and a strong correlation between the lowest contrast level to the 3D-CTAG and the average brightness sensitivity to microperimetry (ρ = -0,82).
In wet AMD patients a statistically significant correlation between the indicators of the average light sensitivity and VLRH (ρ = -0,69, p <0,05) was revealed. At the same time the light sensitivity in the projection of the pathological focus has a strong negative correlation with VLRH (ρ = -0,85, p <0,05) which shows the depression areas coincidence detected by both methods. Fixation parameters also have a negative correlation of medium strength with the volume of lost visual field: ρ = -0,65, p <0,05 for the localization of the fixation point in the range from 1° foveola. Thus, the more the scotoma volume is, the less central fixation is. The maximum corrected visual acuity decreases when the size of the central scotoma increases (ρ = -0,60, p <0,05). The volume of lost visual field is also closely correlated with the size of the pathological focus on fluorescent angiography (ρ = 0,88, p <0,05).
In the analysis of structure-function relationships in wet AMD patients there is a strong direct correlation of absolute volume lost visual field on 3D-CTAG and the volume of retinal edema (ρ = 0,77), the area and volume of neuroepithelium detachment (NED) (ρ = 0,72, and ρ = 0.73, respectively), and the direct correlation of moderate volume lost sight with the area of edema (ρ = 0.67) and the volume of CNV (ρ = 0.56) (Figure 4). Thus, the presence of retinal edema and NED, as well as the large size of CNV are unfavorable factors with regard to visual function, as the area affected by increasing macular area increases the volume of the central scotoma and, consequently, the quality of patients’ life decreases. We have not found any correlation between the thickness of the retina in the central zone and the functional tests data in dry AMD patients.
The functional tests dynamics during the treatment was also analyzed. Patients with the dry form of AMD in subgroup IA after 3 months of therapy with Vitrum Vision Forte demonstrated the improvement in BCVA (0,1 LogMAR) (p <0.05) whereas no changes were observed in subgroup I B. According to the results 3D-CTAG (Table 2) the number of defects in each eye in subgroup I A significantly decreased 1 (0.1) to 0 (0,0), the lowest contrast level significantly decreased from 7 (5; 11)% to 5 (4; 7)% AVL 136.5 (0; 320) deg2 to 0% (0; 0) deg2%,VLRH 0.2 (0, 0.46) of 69300 deg2% to 0% (0 ; 0) of 69300% deg2%, while in subgroup IB negative dynamics was noted: the lowest contrast level increased from 8.5 (5; 13) to 12.5 (5; 13) (p <0,05), AVL from 183 (0; 341) to 254 (0, 427) (p <0.05), VLRH from 0.26 (0, 0.49) to 0.37 (0, 0.62) (p < 0.05). Average light sensitivity significantly increased after treatment from 24.56±3.39 dB to 2.69 dB±26,39 (p <0.01) in the subgroup 1, whereas two changes have been verified. Thus, the administration of Vitrum Vision Fort showed its positive effect on the function of the retina macular area in patients with dry form of AMD which resulted in the visual acuity increase, reducing the number and scope of the central scotoma, and increased sensitivity of the retina compared to the control group.14
The subgroup II A had the same improvement in BCVA 1 month after ILI (0,2 LogMAR) (p <0,01) compared with the subgroup II B (0,2 LogMAR). Light sensitivity in the projection of the pathological center increased from 18.92 (17.36; 20.27) dB to 21.2 (19.9; 22.96) dB (p <0,01); in the 3D-CTAG AVL significantly decreased from 3012 (2043; 4711) deg2% to 1195 (650; 1456) deg2% (p <0,01) in the subgroup II A and from 6606.5 (3770.5, 8032, 5) to 4495.5 (2567, 5813.5) in the subgroup II B; VLRH decreased to 4.35 (2.95; 6.8)% of 69300 deg2% to 1.77 (1.19; 2.82)% of 69300 deg2% (p <0,01) in the subgroup 2a and 9.54 (5.44; 11.59) to 6.93 (4.45; 8.39) in the subgroup 2b, respectively. Moreover, the effect of anti-VEGF therapy depends on the time of the 1st injection: it has proven to be most effective with the edema no older than 6 months. (AVL and VLRH decrease in 2.46 times) and slightly lower effective in the later periods (decrease AVL and VLRH 1.38 time).
In group III visual function did not significantly changed after 1 month indicating the irreversible destruction of the photoreceptors and RPE cells in the fibrous scar. No signs of retinal edema during the observation time in this group were detected. Patients with DME demonstrated positive dynamics of metamorphopsia 1 month after ILI: the number of defects significantly decreased from 2 (2, 3) 1 (0, 2) (p <0,01), in the 3D-CTAG the AVL decreased 1.6 times from 829 (508; 1119) deg2% to 280 (0, 888) deg2% (p <0,05) and VLRH - from 1.2 (0.73; 1.61)% of 69300 deg2% to 0.53 (0, 1.28)% of 69300 deg2% (p <0,05), respectively. Thus, the addition of a standard diagnostic scheme to detect macular pathology with 3D-CTAG is able to enhance the efficiency of diagnosis and treatment of macular diseases due to timely diagnosis of macular edema.
3D-CTAG method provides more opportunities in the diagnosis of the severity and nature of macular area lesions, including dry and wet AMD and DME forms compared with traditional Amsler test.11 We must objectively define the role of 3D-CTAG in quick testing and dynamic self-control in the diagnosis and treatment of macular diseases and create the algorithm of its use among other diagnostic methods. Partial defects like relative scotoma or metamorphopsia in the central visual field are typical changes in patients with the dry AMD registrable by 3D-computer-threshold Amsler grid test. In rare cases we saw the absolute scotoma with steep slopes. The localized reduction in light sensitivity in the large drusen field and atrophy lesions was revealed by the microperimetry. Microperimetry reveals early changes in light sensitivity in patients with the dry form of AMD which are not detected by other methods.
In 90% of the wet form of AMD we can see the enormous central vision loss so it is important to diagnose the macular edema earlier and conduct anti-VEGF therapy. The study conducted by Robison CD, et al.,14 revealed that the patients with wet AMD have such defects as a shallower slope only in 57% of the cases. These areas correspond to the brightness sensitivity depressions in microperimetry. Unstable fixation was detected in 53.5% of patients with wet form of AMD. We found that steep slopes defects were typical not only for dry form of AMD, but also for the fibrous scar which significantly expands the data obtained by Robison CD et al.,14 Zero value of the contrast level in patients with dry form AMD is 4 times less than that value in patients with wet AMD (7 (5; 11) over 28% (25; 36.5)%, respectively).
According to the study conducted by Jivrajka RV et al.,11 multiple defects are defined as “scotoma of inverted cones” (defects 3.56±2.96 1 eye) in patients with DME. In our study we revealed multiple metamorphopsia (number of defects per 1 Eye 2 (2, 3)) in patients with cystic DME which is confirmed by horizontal and vertical slopes on the histogram. The microperimetry in DME patients has revealed diffuse decrease in brightness sensitivity which should be considered in the dynamic monitoring of those patients. However, the microperimetry is a laboratory, time-consuming (an average of 15 minutes or more in one eye) and difficult-for-patient procedure so it can hardly be suitable as a screening test. The original - 3D-computer-threshold Amsler grid test allows to determine the size and nature of the pathological focus in the retina macular area in patients with wet form of AMD and fibrous scar as the size of the central defects is closely correlated with the data of OCT and fluorescent angiography that is very important in the prognosis of visual function.
Thus, the positive effect of multivitamins in the treatment of the patients with dry form of AMD is confirmed by the lowering numbers and volumes of central scotomas. The efficacy of anti-VEGF therapy of wet AMD depends on the time of edema: decrease of AVL in 2.46 times in the period of less than 6 months; and slightly lower decrease AVL in 1.38 times in the period of more than 6 months. In DME cases metamorphopsia reduction with anti-VEGF therapy has been recorded. 3D-CTAG can be used as self-monitoring for timely detection of macular edema recurrence in patients with fibrotic scar.
None.
The author declares there are no conflicts of interest.

©2016 Kovalevskaya, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.