eISSN: 2577-8250


Review Article Volume 6 Issue 1
1Medical Education Department, Brighton Sussex Medical School, England
2Exercise & Sport Science Department, Judson University, USA
3Nursing Education Department, Loyola University, USA
4Ear, Nose, and Throat Department, New Cross Hospital, England
5Maxillofacial Surgery Department, Queen Victoria Hospital, England
Correspondence: Brendan Meany, Exercise & Sport Science Department, Judson University, USA
Received: February 13, 2024 | Published: March 13, 2024
Citation: Fenn J, Meany B, Rescober S, et al. Communication in virtual reality as applied to medical education. Art Human Open Acc J. 2024;6(1):56-59. DOI: 10.15406/ahoaj.2024.06.00222
Virtual Reality (VR) has materialized as a technology enabling users to experience computer-generated 3D environments.1 Medical education programs have recently incorporated VR into their curriculum as a supportive means of experiential learning modalities like laboratory exercises and simulation training.2 Applying Kolb’s Experiential Learning Theory,3 the use of VR in medical education allows students to acquire knowledge and develop “soft skills” like collaboration, communication, and teamwork through interactive processes.2,4,5 Traditionally, medical training has occurred in siloed specialties instead of integrated practices that require coordination across disciplines to provide excellent patient care.6 While the efficacy and realism of VR have room for improvement, incorporating VR into experiential exercises can enhance non-technical skills such as interpersonal interactions, minimize medical error, democratize opportunities, and galvanizing diverse people and practitioners.6–9 This practical review briefly explains VR’s utility, its function as an experiential learning tool, and application in clinical exercises.
Keywords: virtual reality, communication, medical education, experiential learning, clinical application
Technological advances in human communication will undoubtedly be listed as a major achievement of the 20th century.10 Virtual Reality (VR) has emerged as a nascent technology that enables communication in a computer generated 3D environment, simulating real-world or imagined experiences.1 The latest iterations of the technology allow for both interpersonal and mediated communication. This review aims to explore communication in VR as applied to Medical Education, which include the advantages and challenges of communication in virtual environments, the learning theories and models that relate to VR, and the application of VR to real-life communication in healthcare. Finally, the potential future direction of VR communication is discussed with concluding remarks.
Communication in virtual reality
VR creates a sense of presence, where a user feels as if they are physically present or immersed in the virtual environment. These VR environments facilitate unique social interaction and collaboration through features like voice-chat, spatial-audio, hand gestures, and shared experiences.11 Users can engage in real-time conversations, share experiences, and collaborate on tasks within the virtual space. Virtual meeting rooms, social VR platforms, multiplayer VR games, and simulated VR teaching applications are examples of how users connect, interact, communicate, and collaborate in VR. VR enables users to collaborate in teams and communicate remotely, devoid of geographical boundaries.
Maloney et al.,12 explored nonverbal communications in VR as it plays a crucial role in conveying meaning and emotions. In virtual environments, nonverbal cues are conveyed through gestures, body language, and facial expressions of avatars. Advances in motion-tracking technologies enable accurate capture and representation of users' real-time movements, enhancing the fidelity of nonverbal communication in VR. The ability to perceive and interpret nonverbal cues contributes to more effective, nuanced, and realistic interpersonal communication. Head nodding, eye gaze, proximity, and body orientation are an integral component of nonverbal human communication that is replicated in VR.13 Although all these cues are demonstrable, the acuity and realism of such gestures in VR can leaves a sense of implausibility compared to real life. Perhaps future developments in the technology will address this need.
VR communication in medical education
Communication skills training is now a core aspect of medical education, generally introduced early and continually developed throughout medical school programs.7 The necessity for developing effective dialogue was highlighted in a study conducted by Real et al.,14 They found that enhancing the communication capabilities of healthcare professionals improved patient interactions and led to better overall outcomes. Leveraging the imperative of interactions between colleagues and patients, modern medical pedagogical strategies are now shifting toward the use of virtual patient simulations.5 Computer modelling offers more flexible and reproducible environments, capabilities of catering to multiple students simultaneously, provide uniform clinical scenarios, and simulate rare but important clinical situations.2,4 These applications tangibly benefit teaching communication skills in the field of medical education. Virtual patient interactions and VR avatars, which can overcome some of the logistical problems associated with coordinating inter-professional groups at scale, maximizes the financial and spatial constraints many medical schools face. VR patients can be used to simulate difficult conversations in practice while simultaneously fortifying other soft skills such as empathy in more detail than real life challenging situations.15 Whereas an array of live actor responses can confuse the student, groups may experience vastly different patients in every cycle than in VR which is uniform and replicable providing consistency for all participants.
Advantages of VR communication
One of the key advantages of communication in VR is the heightened sense of immersion, interactivity, and engagement compared to conventional communication channels such as online e-learning or web-based lectures that became more prevalent during the covid-19 pandemic. This increased immersion can result in improved attention, memory retention, and emotional connection, leading to more efficient communication outcomes.16 By reducing distractions from the physical world, full immersion captures the learner’s attention bringing focus to peripheral skills like communication. The level of engagement is heightened as users interact with virtual objects, navigate through virtual spaces, and collaborate with others in a more natural and intuitive manner than two-dimensionally with a conventional PC, laptop, or mobile phone.
The authenticity of VR communication also enables individuals to have a more memorable and emotionally resonating experience. Studies have shown that memories formed in VR are often more vivid and entrenched compared to traditional media.17 By engaging multiple senses simultaneously, VR can evoke a stronger emotional response and facilitate a deeper understanding of information or experiences being communicated through experiential learning. Moreover, the interactive and multisensory nature of VR allows for a higher level of personalisation and customisation where users can tailor their virtual environment, avatars, and interactions to suit their preferences and needs. This flexibility enables a more tailored and meaningful collaborative experience, enhancing the overall engagement and satisfaction of participants.
In educational settings, VR offers unique opportunities for captivating learning experiences. Students can explore virtual environments, interact with virtual objects, and engage in simulations that simulate real-world scenarios. This hands-on and experiential approach to learning fosters active participation, critical thinking, and problem-solving skills.
Challenges and limitations of VR communication
While VR communication offers numerous advantages, it also faces several challenges and limitations. One significant constraint is the current affordability of the technology. VR headsets and equipment can be expensive, requiring a substantial investment for individuals or organisations. Additionally, the quality of VR experiences can vary depending on the hardware capabilities, leading to discrepancies in the level of immersion and visual fidelity which affects realism and obtaining plausible educational objectives.
Technical issues such as motion sickness and latency can also diminish the user experience in VR. Motion sickness, also known as cyber sickness, occurs periodically and is caused by a discrepancy between the user's visual perception and the body's physical sensations. Although advancements in hardware and software have mitigated this issue to a certain extent, it remains a challenge for some users, and potentially a deterrent.
Similarly, to deficiencies in authenticity effecting equilibrium, current VR capabilities may lack the depth, breadth, and wholeness of nonverbal communication cues compared to face-to-face interactions. Innovations in motion tracking and avatar animations have improved the representation of nonverbal cues and facial expressions, but conveying subtle nuances remains a challenge in VR. This limitation can affect the overall quality and effectiveness of interpersonal communication, particularly in contexts where nonverbal cues play a vital role, such as emotional expression and building rapport. The in congruency between tone of voice and facial expressions in VR can lead to inaccurate perceptions and undesirable outcomes in the learning context.
Outside of user interface, VR also raises social and ethical issues that need to be addressed. As individuals engage in virtual interactions, questions surrounding the ethics of virtual behaviour, privacy, and consent emerge. It is essential to establish guidelines and norms that govern virtual interactions to ensure individuals' rights and dignity are respected- most notably accessibility and inclusivity.18 Physical limitations, such as the need for specialised hardware or motion control, can pose barriers for individuals with disabilities or limited mobility. Moreover, affordability and availability of VR equipment can limit access to virtual experiences for individuals from disadvantaged backgrounds or regions and further widen the inequalities in health education.
In addition to physical accessibility, ensuring inclusive virtual environments is essential. Designing virtual spaces and interactions that cater to diverse populations, including different cultures, languages, and cognitive abilities, is vital to avoid excluding or marginalising certain groups. It requires careful attention to interface design, representation, and user experience considerations to create an inclusive and welcoming virtual environment for all participants.
Learning theory and communication
Providing excellent patient-centred care necessitates dynamic training that emphasises effective communication and collaboration.8 Recently, medical education has incorporated VR training to develop non-technical skills in replicable, standardised, and unique interprofessional competency simulations.5,19 Through experiential learning with systems like VR, heterogeneous medical teams can train soft-skills like collaboration and communication that are vital to patient outcomes.8
The premier theoretical underpinning for experiential learning was devised by Kolb.3 In his phases of learning theory, Kolb posits that for comprehension to take root, learners must pass through four phases of learning Concrete Experience (doing and feeling), Reflective Observation (reviewing or reflecting), Abstract Conceptualisation (drawing conclusions), and Active Experimentation (application of material) (Figure 1).20
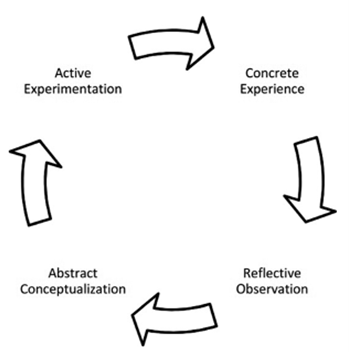
Figure 1 Kolb’s experiential learning cycle stages.21
Education has traditionally been a passive experience where the learner is seated for an extended period, listening intently, and expected to flawlessly regurgitate and apply the material. Kolb3 challenged this archaic model by suggesting that learning is an interactive process where knowledge is forged through the transformation of experience in conjunction with many modalities.6 Although important and necessary, theory is only a small portion in the equation of concept attainment. For comprehensive and flexible application only passing through Reflective Observation and Abstract Conceptualization neglects the Concrete Experience and Active Experimentation aspects of learning- real-world hands-on experiences are vital.3 This becomes even more apparent for working professionals who are continuing education towards advanced degrees, new certifications, or professional development.9
The idea of experiential learning meshes quite well with the field of Medicine. Health care has a longstanding history of skill development through action.9 Until recently though, much of medical training has occurred in siloed schools geared towards specific medical specialities.8 Medicine has become an integrated practice that requires communication and collaboration across disciplines to provide excellent patient care, but many health care providers rarely train those skills in medical school.8 Implementing curriculum, especially in the clinical setting, that uses Kolb’s Experiential Learning Theory (ELT) as a foundation, could solidify knowledge for the learner and greatly improve application, retention, but also communication and collaboration.6 Hospital Associations have reflected a need for new methods of instruction that ultimately end in a better experience for the patient, increase performance of integrated teams, and minimise expenditures for the patient and hospital.8
In a qualitative study conducted by Fewster-Thuente and Batteson,19 undergraduate interdisciplinary students (n = 515) were tasked with completing a scripted simulation focused on patient ward round care. The experiment’s goal was to incorporate Kolb’s ELT as a theoretical framework for Interprofessional Competencies. Post interview, students’ responses were thematically coded to better understand common perceptions of the experience. Frequently, through all four phases of ELT, students used the terms “improved and effective” communication and collaboration as descriptors of their experience. Using experiential learning in the situation setting provided opportunities to connect with the material in an applied manner, but also better understand team members roles and contributions.19
Designing authentic learning experiences can present challenges though. Space, time, and finances all constrain how, what, and when students develop interpersonal patient communication and within group dynamics.8 The literature seldomly examines which method or medium is optimal to deliver the learning experience at scale.6
Application of VR communication to real life communication in healthcare
The use of VR as a source of multidimensional medical training first appeared in the late 1960s and has steadily increased as the first head-mounted displays have come to market.22 Healthcare institutions continuously strive to improve quality and safe standards of care, and effective communication skills remain at its core. In 2012, The Joint Commission identified that ineffective communication among members of the healthcare professional team were at the root cause of sentinel never events in hospitals from 2004 to 2012 in the USA. Lack of communication became the leading cause of preventable errors leading to delays in medical treatment, inaccurate diagnosing, and patient injury and death.8
Effective communication and delivery within the healthcare profession are skills that develop over time, but it begins with the learning environment in which these basic concepts and strategies are obtained. Standards of best practice emphasise the need to create a psychologically safe learning environment for students, and institutions continue to seek ways to enhance their experiences in the clinical setting. They have turned to various simulation modalities such as computerised mannequins, standardised patients, and VR. Some modalities have been found to be more cost effective and sustainable in comparison to “human-controlled” facilitators.23 These teaching strategies promote learning in a low-risk environment. By facilitating experiences in non-threatening environments, students have proven to feel more comfortable to participate, share their thought processes, and take risks without fear of judgment or making mistakes.
Most recently VR has allowed students to take action in a variety of clinical situations. It places the student in a virtual environment and acts as a safe space for learning.24 It allows students to examine patients, performing physical assessments, and conducting patient interviews.25 Utilization of VR increases situational sensitivity and gives students the opportunity to recognize cues, process information, identify interventions, and evaluate outcomes in a controlled space. Nonetheless, it allows the application of critical thinking strategies to make sound clinical decisions.
VR uniquely allows reproducible real-world situations that train socialisation in the professional role. It offers great benefits as students engage in the experience, ask questions, strategize, and utilise their clinical reasoning skills. According to Shorey et al.,5 many students were so focused on the didactic portion of learning, some claimed they needed practice with the communication aspect, appropriately and effectively relaying information with patients, families, and other healthcare professionals. VR helps to bridge this gap from theory to practice by keeping students actively involved through the use of virtual role playing. By placing them in uncomfortable situations, students are challenged by others who may have attitudes, values, and beliefs different from their own. This helps students understand what lies within their scope of practice as well as navigate through the psychosocial barriers and ethical decision-making processes. As a result, these experiences have been viewed as worthwhile and have shown to enhance positive attitudes, increase preparedness, and allow proper dialogue.5
Though VR has proven to provide enhanced educational effectiveness with the communication process, this simulation modality is recognized to have limitations of its own. Arguably, VR still lacks many technological capabilities, and students oftentimes struggle with engaging in the experience. Challenges associated with replicating the variability of human expression- realism, empathy, emotion, and body language- could influence students’ perception of the situation.5 Non-verbal cues such as facial expressions and body language may be lacking, making it difficult for students to accurately diagnosis the issue and connect and communicate.
Studies have revealed that VR has good potential in assessing students’ clinical reasoning skills.24 The educator can utilize VR for safety competencies, interprofessional team training, and practice incorporating tools such as Identity, Situation, Background, Assessment, and Recommendation, as a means for exchanging information between healthcare professionals.23 VR offers great value for appropriate delegation and prioritization as well as evaluating students’ readiness to transition into the professional role.
Communication, leadership and management, teamwork and collaboration, time management and delegation, professionalism, and the ability to problem-solve are important skills for effective patient care. Those who actively engage in VR are able to make recommendations that are realistic and achievable. VR is transferable, applicable, and can serve as a medium to improve communication skills, strengthen performance confidence, and enhance team efficacy in various healthcare settings. This can include palliative care, intensive care, and surgical settings.22 VR can offer opportunities to provide patient education and practice therapeutic communication in instances such as end-of-life care and mental health. Practicing various communication approaches can assist with overcoming challenges related to working in a collaborative group. It can strengthen interprofessional communication skills and aid in teamwork and the decision-making process when collaborating with patients, families, and members of the healthcare professional team.
Virtual reality communication is an emerging technology that transcends physical boundaries and opens new possibilities for remote work, education and social interaction. Virtual spaces and simulations are already revolutionising the way we communicate and collaborate remotely. While the technology is not a panacea, or a replacement for medical education, there is utility as supplementary training for interpersonal skills, which can overcome the limited exposure in formal medical pedagogy. Financial benefits can be made with respects to the higher running cost of simulation centres and logistical problems of gathering interprofessional learners from a myriad of backgrounds and locations. Globally there is a need to train more healthcare professionals and VR communication as a tool to achieving this feat through knowledge sharing.
Currently there is very little literature published comparing the use of VR in consultation training compared with the current methods and this is something that necessitates investigation in the future. Looking ahead, the technology will advance in the level of immersion, realism, and collaborative experiences. Augmenting VR with real-world elements, will provide new possibilities in communication and training healthcare workers to improve patient outcomes.
None.
The authors declare that there is no conflict of interest.

©2024 Fenn, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.