eISSN: 2378-3176


Case Report Volume 6 Issue 2
1Nephrology, City Clinical Hospital n.a. S.P. Botkin, Russia
2Nephrology and Hemodialysis, Russian Medical Academy of Continuous Postgraduate Education, Russia
3Nephrology, State University of Medicine and Dentistry, Russia
4Radiology, City Clinical Hospital n.a. S.P. Botkin, Russia
5Radiology, Russian Medical Academy of Continuous Postgraduate Education, Russia
6Pediatrics, State University of Medicine and Dentistry, Russia
7Pathology, City Nephrology Center, Russia
Correspondence: Elena V Zakharova, City Clinical Hospital n.a. S.P. Botkin, 115284, 2-nd Botkinsky proezd, 5, Moscow, Russia, Tel 7 499 728 8291
Received: March 28, 2018 | Published: April 12, 2018
Citation: Zakharova EV, Makarova TA, Sheikh ZV, et al. Two cases of anti-glomerular basement membrane (Goodpasture’s) disease in female adolescents. Urol Nephrol Open Access J. 2018;6(2):74-75. DOI: 10.15406/unoaj.2018.06.00207
Anti-glomerular basement membrane disease, commonly termed Goodpasture’s disease, is a rare immune complex small vessel vasculitis, affecting glomerular and/or pulmonary capillaries with basement membrane deposition of antibodies against noncollagenous-1 domain of type IV collagen α3 chain, also known as the Goodpasture antigen. Patients may present with isolated renal failure, lung hemorrhage, or both. The most important clinical feature of renal involvement is anuria. The characteristic pathology feature is crescentic glomerulonephritis, with linear immunoglobulin G deposition. Lung involvement generally presents as a hemoptysis or lung hemorrhage, with radiological examination demonstrating diffuse alveolar airspace shadowing. There is bimodal age distribution with peaks at third and sixths decades with higher prevalence in males. Here we present two unusual cases of anti-glomerular basement membrane disease with normal renal function and torpid lung damage in female teenagers.
Keywords: small vessel vasculitis, anti-GBM antibodies, pulmonary-renal syndrome, kidney biopsy, crescentic glomerulonephritis, hemoptysis
aCL, anticardiolipin; H&E, Haematoxylin-Eosin; AFB, acid-fast bacilli; HEENT, head, eyes, ears, nose, throat; ANA, antinuclear antibodies; HIV, human immunodeficiency virus; ANCA, antineutrophil cytoplasm antibodies; hpf, high power field; BP, blood pressure; IgA, immunoglobulin A; C1q, C1q complement component; IgG, immunoglobulin G; C3, C3 complement component; IgM, immunoglobulin M; C4, C4 complement component; i.v, intravenous; CRP, C-reactive protein; LA, lupus anticoagulant; CT, computer tomography; LDH, lactate dehydrogenase; DNA, deoxyribonucleic acid; PAS, periodic acid Shiff; ECG, electrocardiogram; Plt, platelets; ECHO-CG, echocardiography; PNH, paroxysmal nocturnal hemoglobinuria; EGDS, esophagogastroduodenoscopy; RBC, red blood cells; ELISA, enzyme-linked immunosorbent assay; ROM, range of motion; ESR, erythrocytes sedimentation rate; RPR-test, rapid plasma regain test; GBM, glomerular basement membrane; RR, respiratory rate; GN, glomerulonephritis; SG, specific gravity; Hb, hemoglobin; TB, tuberculosis; HBsAg, hepatitis B serum antigen; TBC, total blood count; HCV, hepatitis C virus; WBC, white blood cells
Anti-glomerular basement membrane (GBM) disease, commonly termed Goodpasture’s disease, is a rare immune complex small vessel vasculitis, affecting glomerular and/or pulmonary capillaries with basement membrane deposition of antibodies against noncollagenous-1 domain of type IV collagen α3 chain, also known as the Goodpasture antigen.1,2 Patients may present with isolated renal failure, lung hemorrhage, or both. The most important clinical feature of renal involvement is anuria, however some patients may present with macroscopic hematuria or loin pain. Cases of anti-GBM disease with normal renal function, even though rare, have been described. The characteristic pathology feature is crescentic glomerulonephritis (GN), with linear immunoglobulin deposition, generally IgG and C3. Fibrinoid necrosis may also be present. Lung hemorrhage presents as a hemoptysis with radiological examination demonstrating diffuse alveolar airspace shadowing, but also may be subclinical, presenting as a breathless with cough or as an iron deficiency anemia. There is bimodal age distribution with peaks at third and sixths decades with men presenting at a younger median age than women. The diagnosis relies on the demonstration of linear immunoglobulin deposition along the GBM in the context of crescentic GN, serum anti-GBM antibodies detected by ELISA, have high sensitivity and specificity for disease.3−9 Here we present two cases of anti-GBM disease with high titers of anti-GBM antibodies and moderate pulmonary-renal syndrome in female teenagers.
16 years old Caucasian girl, admitted March 2, 2010.
Main complains
General weakness, dizziness, mild cough with occasional blood streaked sputum, mild breath shortage.
Previous medical history
Varicella and rubella as a child.
History of current disease
In October 2009 she had a cough with just few episodes of blood streaked sputum, resolved on oral antibiotics. Outpatient work-up revealed mild anemia (Hb 11.9 g/dL), urinalysis were normal.
In January 2010 she developed weakness, breath shortage, palpitations and dark urine, and was admitted to the local children’s hospital. Her Hb was now 3.9 g/dL (RBC 1.55 4x1012/L, serum iron 6.5 µmol/L), she had macroscopic hematuria and proteinuria 4.6 g/L. Her serum creatinine was 68 µmol/L; WBC, Plt, ESR, bilirubin, total protein, albumin, LDH, C3, C4, CRP - within normal range. Kidney ultrasound found normal sized kidneys with hypo-echoic parenchyma; abdomen ultrasound and CT, EGDS and ECG were unremarkable. She was diagnosed with iron deficient anemia, treated with blood transfusions and i.v. iron, her anemia improved (Hb 8.9 g/dl) and she was referred to out hospital.
At admission
Alert, oriented; Body temperature 36.2°C, RR 20 per minute, pulse regular 90 per minute, BP 110/75 mm Hg. Undernourished. Skin pale, no peripheral oedema. HEENT and neck otherwise normal. No palpable peripheral lymph nodes. Joints: no swelling, ROM normal. Lungs: clear. Heart: rhythm regular, no murmurs. Abdomen soft, bowel sounds normal. Liver +2 cm below costal margin, non-painful, spleen and kidneys not felt. Urine output - 950 mL/day of dark-yellow urine.
Work up
Final diagnosis and treatment
Based on the pathology and serology findings, patient was diagnosed with anti-GBM disease and started on methylprednisolone i.v. “pulses” 500 mg 3 consecutive days followed by oral prednisone 50 mg/day, cyclophosphamide i.v. “pulses” 1000 mg monthly, and oral iron supplementation.
Treatment results and follow-up
Her condition rapidly improved, cough resolved, Hb level raised to 11.7g/dL, urinalysis showed 50-70 RBC hpf, and serum creatinine became normal (88µmol/L). She was discharged and followed in our hospital outpatient unit. 2 month later her Hb was 12.2g/dL and anti-GBM antibodies were now 3.0U/mL. Cyclophosphamide “pulses” continued (500mg monthly), oral prednisone was slowly tapered. After 8 month of treatment she was doing well, no complains, Hb 13.1g/dL, urinalysis normal, serum creatinine 83µmol/L, anti-GBM antibodies 0.3U/mL Cyclophosphamide was discontinued (total dose 5000mg), and oral prednisone tapered to 20 mg every other day. After 1 year of treatment she was in complete remission on oral prednisone 5 mg every other day, with Hb 14.6g/dL and serum creatinine 76µmol/L. Prednisone was discontinued, and she was followed in outpatient setting. In March 2015 (5 years after the diagnosis) she was doing well, without any signs and symptoms, with Hb 14.4g/dL, normal urinalysis and serum creatinine 84µmol/L. At the latest evaluation, December 2017 (almost 7 years after the diagnosis and 6 year off-treatment) she is doing well, without any signs or symptoms, her routine labs are normal, her anti-GBM antibodies are 5.8U/mL (Table 1).
Time of detection |
Anti-GBM antibodies titers U/mL |
|
Case 1 |
Case 2 |
|
Pre-treatment |
64 |
136 |
2 months under treatment |
3 |
- |
6 months under treatment |
- |
2.8 |
6 month off-treatment |
- |
3.5 |
8 month off-treatment |
0.3 |
- |
6 years off-treatment |
5.8 |
- |
Table 1 Anti-GBM antibodies titers in patients 1 and 2
15 years old Caucasian girl, admitted October 24, 2016.
Main complains
General weakness, weight loss, cough with blood streaked sputum, breath shortage.
Previous medical history
Unremarkable.
History of current disease
In May 2016 she developed dry cough and breath shortage, followed in 2 weeks by blood streaked sputum, and received oral antibiotics without effect. Next month she presented with fever, dyspnea and general weakness, was admitted to the local hospital and diagnosed with pneumonia. She received i.v. antibiotics, fever and dyspnea resolved, but she still was coughing.
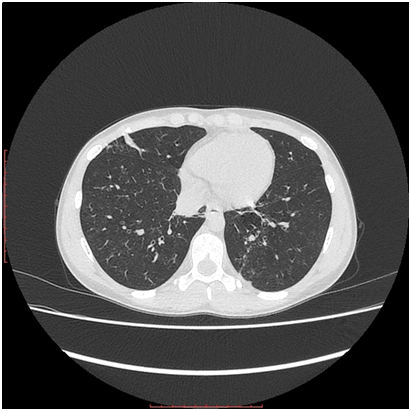
In July 2016 fever recurred, and she was re-admitted to the local hospital. Work-up found mild leukocytosis, microhematuria, chest CT revealed dissemination, and she was started on antituberculotics and referred to the TB hospital. T-spot TB was negative (twice), bronchoscopy revealed nothing but sanious secret. Cytology was negative for AFB, transbronchial lung biopsy found exudative changes without any features of granulomas or neoplasm, Ziehl-Neelsen staining for AFB was also negative. However, respiratory function test showed decreased vital capacity and ventilator lung capacity; and repeated chest CT found multiple bilateral “ground glass” focal consolidation. Tuberculosis was ruled out and she was referred to our hospital.
At admission
Alert, oriented; Body temperature 36.5°C, RR 19 per minute, pulse regular 60 per minute, BP110/70mm Hg. Undernourished. Skin normal, no peripheral oedema. HEENT and neck otherwise normal. No palpable peripheral lymph nodes. Joints: no swelling, ROM normal. Lungs: clear. Heart: rhythm regular, no murmurs. Abdomen soft, bowel sounds normal. Liver +1 cm below costal margin, non-painful, spleen and kidneys not felt. Urine output - 1200 mL/day of normally coloured urine.
Final diagnosis and treatment
Based on CT features and serology findings, patient was diagnosed with anti-GBM disease and started on methylprednisolone i.v. “pulses” 500 mg 3 consecutive days followed by oral prednisone 60 mg/day, and cyclophosphamide i.v. “pulse” 500 mg.
Treatment results and follow-up
Her condition rapidly improved, cough and hemoptysis resolved. She was discharged and further followed in the children’s hospital. She was continued on oral prednisone and cyclophocphamide i.v. “pulses” 400-500 mg every 3 weeks. After 2 months of this treatment she was doing well, and oral prednisone was slowly tapered. After 6 month of the treatment she was doing well, no complains, Hb 14.3g/dL, urinalysis normal, serum creatinine 52µmol/L, anti-GBM antibodies 2.8U/mL, and chest CT now did not reveal any focal changes. Cyclophosphamide was discontinued (total dose 4800 mg), and oral prednisone tapered to 15 mg every other day. After 8 months of treatment she was in complete remission on oral prednisone 5 mg every other day, with Hb 13.9g/dL and serum creatinine 69µmol/L. Prednisone was discontinued in May 2017. At the last evaluation in December 2017 (1 year and 2 months after the diagnosis and 6 month off-treatment) she was doing well, without any signs and symptoms of the disease activity. Her Hb was 12.94g/dL, serum creatinine 76µmol/L, urinalysis were normal, and anti-GBM antibodies 3.5 U/mL (Table 1). Her chest CT was unremarkable, except linear bridle in the middle lobe of the right lung.
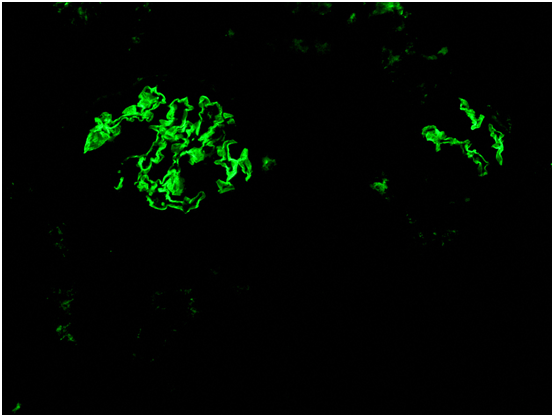
The diagnosis of anti-GBM disease in both cases is unquestioned. Case 1 demonstrates severe anemia, hemoptysis, macroscopic hematuria, necrotizing and crescentic GN with linear IgG deposition along GBM, and high titers of anti-GBM antibodies; case 2, with even higher anti-GBM antibodies titers, presented with hemoptysis, “ground glass” changes by chest CT, and microscopic hematuria. However, our patients show some unusual for anti-GBM disease features.
First of all, anti-GBM disease with prevalence estimated as 0.5-1 per 1 million of inhabitants with higher incidence in the third and sixth decades is even rarer in children and adolescents, and in the younger population males are more susceptible, than females.4,7,10,11 In the contrary, both our patients are female teenagers, which do not match common age and sex general predominance, even though cases of anti GBM disease were recently described in 8 years old and 2 years old girls.8,12
Secondly, the most characteristic for anti-GBM disease clinical feature of renal damage is hematuria with mild-to-moderate proteinuria, rapidly progressive renal failure and anuria.5 However, patient 1, who presented with macroscopic hematuria, had only slightly impaired kidney function, which was revealed almost 3 month after the onset of the disease. That is quite surprising, taking into consideration high titers of serum anti-GBM antibodies, clear linear IgG deposition along GBM, fibrinoid necrosis and crescents, confirmed by renal pathology. The only explanation might be the focal pattern of the renal injury with 2/3 of normal glomeruli, which, again, is unusual - commonly, the majority of glomeruli show crescents of similar age.6 Patient 2, even though she had extremely high titers of serum anti-GBM antibodies, demonstrated only microscopic hematuria and well preserved kidney function. We did not perform kidney biopsy in case 2 because of very modest renal involvement, but based on microscopic hematuria one can speculate, that mild focal anti-GBM antibodies deposits could be seen in the renal tissue. Of note, only 60% of patients with anti-GBM disease demonstrate pulmonary-renal syndrome, and isolated lung hemorrhage in the absence of GN may be the only clinical presentation.7 Worthy to mention that in both cases circulating anti-GBM antibodies were detected using ELISA method, while the study, comparing ELISA with the indirect immunofluorescence showed ELISA sensitivity 94.7-100.0% depending on the kits. Same study confirmed specificity vs normal controls 100.0%, and specificity vs disease controls 90.9-100.0%; false-positive results were found only in the patients with ANCA-associated vasculitis.12 Both our patients were ANCA-negative, therefore we rely on the anti-GBM test results and consider them to be highly positive indeed.
And the last but not least, lung involvement in both cases was also relatively modest and torpid. In case 2 only chest CT demonstrated micro-focal “ground-glass” changes, characteristic for the early stage of the disease, or for the torpid course,13-17 while the plain chest X-ray examination failed to reveal any pathology features, even though the latest studies (both X-ray and CT) were performed 6 months after the disease onset. Such discrepancy between CT and Chest X-ray data is well described in the literature.13 In case 1 plain chest X-Ray also did not show any changes, despite severe iron deficient anemia, suggesting subclinical hemorrhage into alveolar spaces. Unfortunately we were not able to perform chest CT in that particular case, but we presume that diffuse “ground-glass” foci might be confirmed by CT, if it would be done.
The initial treatment for anti-GBM disease, according to current International Guidelines, includes immunosuppression with cyclophosphamide and corticosteroids plus plasmapheresis in all patients with anti-GBM GN except those who are dialysis-dependent at presentation and have 100% crescents in an adequate biopsy, and do not have pulmonary hemorrhage.18 The reason why we avoided plasmapheresis and used only cyclophosphamide and corticosteroids is that in both cases the disease was not that severe and we considered the risk of infectious complications versus benefits of plasmapheresis unacceptable. However, the titers of anti-GBM antibodies in both cases rapidly decreased to normal range in both cases, almost simultaneous with clinical improvement. International Guidelines do not recommend maintenance therapy for anti-GBM disease, and we discontinued cyclophosphamide when cumulative dose of 5000 mg was reached, and slowly tapered and discontinued prednisone after 1 year in case 1 and after 8 months in case 2. No relapses during the follow-up period 6 years off-treatment in case 1 and 6 months off-treatment in case 2 developed so far, which one might expect. The relapses are uncommon in anti-GBM disease except the patients with double positivity (presence of both ANCA and anti-GBM antibodies) with poorer prognosis.19
We conclude that anti-GBM disease may occur in adolescents, and this diagnosis should be considered even in the absence of full-blown pulmonary-renal syndrome. Unexplained anemia and/or blood streaked sputum in combination with macroscopic or microscopic hematuria are suggestive for anti-GBM disease even if they are not accompanied by X-ray examination characteristic features. Detection of elevated serum anti-GBM antibodies, linear expression of IgG and crescents by kidney pathology, and chest CT finding of “ground-glass” focal changes are confirmative for the diagnosis.
None.
Authors declare there is no conflict of interest in publishing the article.

©2018 Zakharova, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.