eISSN: 2378-3176


Review Article Volume 3 Issue 3
1Department of Urology, Huazhong University of Science and Technology, China
2Institute of Urology, Huazhong University of Science and Technology, China
Correspondence: Shaogang WANG, Department of Urology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, No. 1095 Jiefang Avenue, Wuhan, China, Tel 86-27-83663460, Fax 86-27-83663460
Received: January 06, 2016 | Published: June 15, 2016
Citation: DIRIE NI, MALE M, LU Y, et al. The novel use of flexible ureteroscopy and holmium: YAG laser in the management of parapelvic renal cysts. Urol Nephrol Open Access J. 2016;3(3):89-93. DOI: 10.15406/unoaj.2016.03.00081
Kidneys are very common sites of cysts in the human body, prevalence of renal cysts was estimated to be about 10% in the general population and the incidence increases with age. Parapelvic and peripelvic cysts grow near renal collecting system; these types of cysts are most likely to be symptomatic. There are a number of reports describing successful laser incision drainage of parapelvic cysts into the renal pelvis using flexible ureteroscopy transurethrally. This review focuses on specific aspects of clinical usage and novelty of flexible ureteroscopy and holmium laser in the management of parapelvic cysts. A systematic review of articles written in the English language on the subject appearing in the medical journals was conducted using Medline database. Cysts that grow near and inside renal pelvis almost always present with symptoms and require treatment intervention. The intervention is guided by the size of the cyst and severity of the symptoms. Flexible ureteroscopic holmium laser marsupialization of parapelvic cysts is less morbid and complications when compared to laparoscopic decortication approach which is technically very challenging due to the locations of these types of cysts. Retrograde marsupialization of parapelvic cysts is a novel technique which does not need any skin incision at all, thus improving cosmesis after surgery. This approach is a pure and of classical natural orifice transluminal endoscopic surgery (NOTES), it reduces morbidity, mortality, and surgical complications.
Keywords: retrograde, flexible ureteroscopy, parapelvic renal cyst, laser
NOTES, natural orifice transluminal endoscopic surgery; CT, computed tomography; IVU, intravenous urography; UPJ, ureteropelvic junction.
The Kidneys are very common sites of cysts in the human body, prevalence of renal cysts was estimated to be about 10% in the general population and incidence increases with the increase of age.1 Most renal cysts are simple, peripherally located, and asymptomatic of unknown etiology. Many of these lesions are incidentally found during the routine physical checkup, however, some patients might present with hematuria, flank pain, hypertension and pelvicalyceal obstruction. Parapelvic cysts are originated from parenchyma and protrude to the renal sinus while peripelvic cysts are dilated lymphatic vessels, both of these types are grouped in one and are often used interchangeably; generally they are confused with hydronephrosis but rarely can cause true obstruction.2 These types of cysts are most likely to be symptomatic because of their locations; they compress renal hilar structures and pelvicalyceal system.3 The diagnosis of renal cysts is confirmed by abdominal ultrasonography or abdominopelvic computed tomography (CT).4 Intravenous urography (IVU) shows filling defect in the renal pelvis in which the differential diagnosis could be hemorrhage, transitional renal cell carcinoma and radiolucent stones.3 In class I category according to Bosniak renal cyst classification, CT shows sharp margination and demarcation from surrounding renal parenchyma, the cystic wall is smooth, thin and the water density content shows homogeneity throughout (0-20 HU) without enhancement after intravenous injection of contrast media5 see Table 1. As medical and technology advanced, the management of renal cysts changed from major to minimal and to pure natural orifice transluminal endoscopic surgery (NOTES) approach. In the medical literature, we found many different treatment approaches for managing renal cysts including open or laparoscopic unroofing, percutaneous aspiration with or without instillation of sclerosing agents, retrograde marsupialization, and percutaneous resection of the cystic wall.
Stage |
Cyst wall |
Septa |
Calcification/enhancement |
I |
Hairline thin |
No |
No/No |
II |
Minimal regular |
Few, hairline thin |
Smooth, hairline |
Thickening |
Thin/No |
||
IIF* |
Minimal regular |
Multiple, minimal |
Thick, nodular/No |
Thickening |
Smooth thickening |
||
III |
Irregular |
Measurably thick, |
Thick, nodular, |
Thickening |
Irregular |
Irregular/Yes |
|
IV |
Gross irregular |
Irregular gross |
Thick, nodular, |
Thickening |
Thickening |
Irregular/Yes, tissue and cyst |
|
Table 1 Bosniak renal cyst classification
*F in IIF is for follow-up.
Laparoscopic renal cyst unroofing is the preferred treatment approach in many medical centers including ours. Laparoscopic unroofing is an effective approach when treating peripheral cysts. To expose the cyst, extensive tissue dissection is needed particularly when treating overweight and obese patients during laparoscopic surgery. Laparoscopic parapelvic cyst unroofing remains very challenging compared to the peripheral renal cysts because of the close relation to the renal pelvis and renal hilar structures and also due to their deep-seated location in the renal pelvis.6 Modern flexible ureteroscope allows access to the entire intrarenal collecting system in about 94-100%, likewise, the introduction of very small holmium lasers permitted more deflection of flexible ureteroscopy, and these developments have dramatically improved urological intraluminal surgeries.7–9 Retrograde intrarenal marsupialization of parapelvic cysts is considered to be a novel technique, this approach reduces morbidity and complications; it improves cosmesis by leaving no scar at all at the end of the surgery.10 Knowing all the different treatment modalities in the management of renal cysts, decisions must be based on whether the cyst needs intervention at first place and which management approach will be appropriate to use.
A PubMed search was performed using keywords ‘peripelvic’, parapelvic renal cyst’, ‘flexible ureteroscopy’, and ‘holmium laser’, we only reviewed articles published in the English language. We selected original papers reporting safety and feasibility of retrograde flexible ureteroscopic marsupialization of parapelvic cysts using holmium laser. We excluded procedures other than the transurethral approach in the management of these cysts such as percutaneous and laparoscopic approaches.
Transurethral marsupialization of parapelvic renal cysts
Over the last three decades, urologic medical instrumentations have rapidly advanced in the collaboration of medical technologists and surgeons, these developments have dramatically changed the way of diagnosing and treating patients. It allowed clinicians to think of any possible approach for managing one particular disease to minimize morbidity and mortality. This is particularly true in urological diseases, in which, it’s possible to approach one particular disease in many different routes. Minimal invasive management of renal cysts has completely replaced the traditional open approach. Kavoussi et al.,11 first described a case of a patient presented with a large parapelvic renal cyst compressing ureteropelvic junction (UPJ), they managed it transurethrally using ureteroscope by incising the cystic wall and created a permanent connection between the renal pelvis and the cyst thus allowing cyst fluid to continuously drain into the renal pelvis.
Since 1991 no other authors have reported using this approach until later in 2007 O’Connor et al.,12 reported a similar case of a 37 years old female patient presenting with a 4 months history of intermittent right flank pain in which her CT scan showed 4.5x5.5cm parapelvic renal cyst, they reported that percutaneous aspiration of the cyst was not possible because of the cysts’ location and as a result decided to do transurethral ureteroscopic marsupialization of the parapelvic cyst using holmium laser. Although randomized controlled trials with long-term follow-up and outcomes are not available, but there are many studies that assessed the feasibility and safety of flexible ureteroscopy and holmium laser in the treatment of parapelvic renal cysts,10,13-17 a summary of results of these studies are shown in Table 2.
Investigator |
Publication year |
Patients (n) |
Male/Female (n) |
Mean age (Yrs) |
Preoperative cyst mean-size(mm) |
Operative time (Min) |
Hospital stay (Days) |
Postoperative cyst size(mm) |
Kavoussi et al.11 |
1991 |
1 |
NA |
NA |
NA |
NA |
NA |
NA |
O’Connor et al.12 |
2008 |
1 |
0/1 |
37 |
45 |
NA |
NA |
NA |
Bassiri et al.13 |
2010 |
2 |
Feb-00 |
54.5 |
62.5 |
32.5 |
NA |
NA |
Li et al.14 |
2011 |
16 |
9-Jul |
49.8 |
68 |
35 |
3.4 |
13 |
Luo et al.15 |
2014 |
15 |
6-Sep |
53 |
61 |
31 |
3 |
12 |
Mao et al.16 |
2015 |
21 |
9-Dec |
49 |
45 |
27 |
2.6 |
10 |
Yu et al.10 |
2015 |
35 |
18/17 |
48.6 |
NA |
25 |
3 |
NA |
Zhao et al.17 |
2015 |
28 |
17-Nov |
NA |
NA |
26 |
6-Mar |
NA |
Table 2 Summary of pre & postoperative parameters from published series on Retrograde Marsupialization of Parapelvic Cysts
*NA, not available.
Preoperative management
Patients who have parapelvic renal cysts are diagnosed either by ultrasound, computed tomography (CT) or IVU (intravenous urography) as shown in Figure 1. After confirmation of parapelvic renal cysts, and then urinalysis, urine culture, serum electrolytes, blood coagulation tests are evaluated prior to the treatment intervention. Patients with coagulopathy, cardiopulmonary insufficiencies or with active infections are excluded from undergoing this type of procedure. In all the studies, patients receiving transurethral marsupialization of parapelvic cysts were selected with strict selection criteria including; 1) Symptomatic patients such as flank pain, hypertension or hydronephrosis, 2) Patients with single parapelvic renal cyst compressing renal collecting system, 3) Patients with previous failed treatments 4) Patients without ureteral stricture, 5) Bosniak class I cysts on CT scan, 6) Cysts greater than 3cm and close to the pelvic wall.15,16 Some authors10,16 carried out ureteral stenting prior to the surgery about 1-2 weeks to passively dilate the ureter in order to attain smooth ureteral passage during the surgery, while other authors performed the procedure without prior stenting. According to Mahajan et al.,18 during RIRS (retrograde intrarenal surgery) reported that first setting flexible ureteroscope can reach to the kidney without prior ureter stenting, they have found that 94.5% success can be achieved when ureter access sheath is used. To prevent possible infections, prophylaxis antibiotics should be given to the patients before the surgery undertaken. Some investigators reported giving patients ceftriaxone (1.0g) 30 minutes prior to the surgery.16
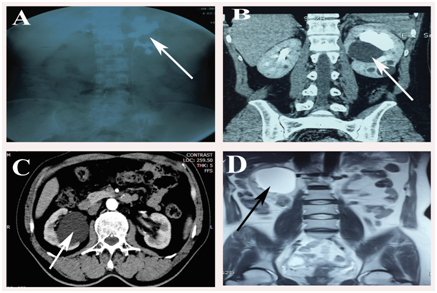
Figure 1 A) Intravenous urography showing left kidney parapelvic cyst (Arrow pointing filling defect). B) and C) Examples of parapelvic cysts on computer tomography (CT) scan. D) Example of magnetic resonance image (MRI) showing parapelvic cyst of right kidney.
Intraoperative management
Patients undergoing retrograde flexible ureteroscopic parapelvic cyst marsupialization were placed in the lithotomy position under general anesthesia. Most of the investigators routinely first introduce rigid ureteroscope to identify the target ureter orifice and then the Zebra guide wire is inserted, ureteroscope is advanced until it reaches renal pelvis, then rigid ureteroscope is removed, and ureter access sheath is introduced. Some investigators used semi rigid ureteroscope13,14 while others used flexible ureteroscope to perform this procedure. Flexible ureteroscopy was passed inside the 12.5F access sheath to reach renal pelvis and the parapelvic renal cyst visualized. Investigators described parapelvic cyst as grey-blue or dark blue in color, thin semitransparent or transparent, bulging into the renal collecting system when viewed from renal pelvis.
In a study by Mao et al.,16 which reported that injecting methylene blue percutaneously into the cyst through an ultrasound guided puncture prior to the transurethral procedure can help to identify the cystic wall, thus reducing risks of renal pelvis injury. Cystic fluid can either be collected by percutaneous puncture or transurethrally using an open-end ureter catheter for cytological and/or bacteriological analysis.14,16 A renal cyst is incised with either 360µm holmium laser12 or 200µm holmium laser.10,15 Some authors used electrocautery hook13 or 3F needle electrode14 to incise the cystic wall. As the main purpose of this surgery is to create a permanent communication between cysts and collecting system, after achieving clear visualization of the cyst, the most important step of this novel technique is to make a proper incision of the cystic wall tissue. A very large incision can result in damaging the collecting system and too small incision may cause insufficient cystic drainage and/or auto-closure of the cystic wall after the surgery. To avoid bleeding and/or closure of the incision, holmium laser can be used to coagulate the margins of the cystic wall. For instance, O’Connor and colleagues12 made a 4cm long incision, while other authors reported of having a 2-4cm long incision,14,15 but Zhao and colleagues carved the cyst wall only about 1 cm. Using ureteroscopic biopsy forceps or holmium laser, the cystic wall tissue can be harvested for histopathological examination.
At the end of the procedure 5F or 6F double J stent can be left in place with the proximal end coil inserted into the unroofed cystic cavity. Double J Stent can be removed 1-3 months after the surgery. According to Bassiri et al.,13ureteral catheter is inserted into the unroofed cyst, and then retrograde pyelography is performed hours after the surgery to examine the patency of the cyst into the renal pelvis. Patients concurrent with renal stones can have their procedure performed simultaneously by dusting or fragmenting the stones with the same holmium laser, and patients with bilateral parapelvic cyst can also have their cyst incised in one stage procedure, while those with polycystic kidney disease can undergo a 2 stage procedure.10 No severe or minor complications related to this technique such as bleeding, adjacent organ injury or infections were reported. An operative time ranging between 25min to 40min is reported with patient’s hospital stay ranged between 2 to 4 days while laparoscopic decortication is reported having mean operative time of 159 min (range: 113-189), blood loss of 55ml (range: 20-78) and mean hospital stay of 3.5days (range: 3-5).6,19,20
Radiologic success was considered to be the key parameter determining the success of this novel technique, which is defined as having no recurrence or >50% reduction of the cystic size after the operation. Radiologic success ranging between 74-93% is reported in the literature.10,14,17 Hypertension is being associated to be a major finding of patients with renal cyst, in a study by Kim and colleagues, they found hypertension prevalence rate of 15.5% in the patient with simple renal cyst, they also noted that larger and bilateral cysts are related with higher risk of hypertension development.21 Bassiri and colleagues operated a patient presented with parapelvic renal cyst accompanied by high blood pressure (165/95 mmHg), and they observed a significance decrease in blood pressure decrease (135/85 mmHg) after the surgery,13 while Zhao and colleagues also observed normalization of the blood pressure in three out of four patients in their study after receiving transurethral ureteroscopic laser cystic marsupialization.17
Mild to moderate hydronephrosis is a common finding in the patients of parapelvic cysts due to the cystic location in the renal pelvis which can cause obstruction of urine outflow. Transurethral ureteroscopic cyst marsupialization results in the disappearance of the hydronephrosis either partially or completely. Yu and colleagues found 15 out of 35 patients with mild to moderate hydronephrosis, after the surgery all 15 patients with hydronephrosis resolved completely (100%). In the same study (Yu and colleagues), 5 patients with polycystic kidney preoperative renal volume were measured 512-865mL, after the procedure significant volume reduction measuring 93.76±7.38mL per side has been achieved. They also observed an increase in the glomerular filtration rate in some of their patients while serum creatinine level significantly decreased after the surgery.10
The symptoms caused by renal cyst are related to the location and size of the cyst, symptoms are the result of compression of nearby structures by the cyst. Parapelvic and peripelvic cysts are most likely to be symptomatic while peripheral cysts are commonly asymptomatic. Flank pain with various degrees is the predominant symptom, thus, postoperative pain relief is also used as successful parameter, Li and colleagues reported 87% (13/15 patients) symptomatic success in their study after the surgery.14 Laparoscopic unroofing of peripheral renal cyst is relatively less technically challenging compared to the other major urological procedures, it is even very common to be performed by a junior urologist in many medical centers, but parapelvic and peripelvic renal cysts are quite a different story because of their close proximity to the renal pelvis and hilar structures, in reality, it’s very challenging to operate laparoscopically, they demand more laparoscopic skills than simple peripheral cysts, particularly if obese or overweight patient is to be operated.
The obese and overweight population is increasing globally.22 66.3% of American adult population are being categorized as obese or overweight , this is not only a risk to population’s general wellbeing but also related increasing technical challenges during surgical procedures by fighting with bulky fatty tissues before reaching the target organ.23 Transurethral flexible ureteroscopic parapelvic cyst marsupialization is a natural orifice transluminal endoscopic surgery (NOTES) and could be an alternative option or arguably better choice to laparoscopic decortication.
Patients with previous renal surgery can benefit from this novel technique, knowing the challenges of fibrotic tissues during second operations, going through transurethral route will escape the need of facing these difficult challenges during laparoscopic and open surgeries. This procedure carries less risk of damaging renal hilar structures except the lower pole cysts which are considered as high risk according to some of the investigators. Lack of extensive tissue dissection and reduced risk of injuring major blood vessels will lead to less bleeding, thus, patients with other comorbidities and bleeding tendencies such as patients with liver disease, diabetics, chronic renal insufficiency or taking anticoagulant therapy can benefit from this approach. Transurethral flexible ureteroscopic parapelvic cyst marsupialization approach is related to reduce technical challenges, morbidities, operative time and hospital stay and also improves cosmesis. A major advantage of this technique is when patients with parapelvic renal cysts are complicated with ipsilateral or contralateral intrarenal or ureteral diseases such as urinary stones then simultaneous management of both cysts and other diseases can be carried out in one stage fashion without the need of another anesthesia and surgery, in this way it can be a cost effective approach.
Limitations
This technique is limited to parapelvic cysts which are small fractions of simple renal cysts. On the other hand, flexible ureteroscopy and holmium laser are very fragile and of high cost to purchase and in addition to their relative short lifespan they require an extra cost for maintenance. These are the major drawbacks of worldwide usage of this equipment. There is a high possibility of equipment failure to reach in the renal collecting system if used patients with ureteral stenosis, severe ureter kinking and ureteral strictures. And if using semi rigid ureteroscope, reaching the lower pole of the renal cyst is very challenging if not impossible. Lack of full thickness incision of the cystic wall to achieve satisfactory unroofing in order to prevent auto-closure and lack of enough tissue specimens for histopathologic analysis involving in this technique is considered to be another limitation. The pathologic analysis is particularly important in the patients suspected to have higher Bosniak renal cyst classification; these patients may later need partial nephrectomy as definitive treatment. Some authors reported15 a good outcome by using holmium for coagulation, but harmonic scalpels used during laparoscopic decortication have better coagulation effect to stop bleeding than holmium lasers which are used in this technique. Thus, in the cases of extensive intraoperative bleeding could be troublesome during this approach.
Treatment of parapelvic/peripelvic renal cysts using flexible ureteroscopy and Holmium: YAG laser is a novel technique which does not need any skin incision at all. This approach is an effective, minimally invasive and smart way to manage this disease with fewer complication rates and acceptable procedure-related outcomes. This technique reduces morbidity, mortality, and complications, it also improves surgical cosmesis.
Author declares that there is no conflicts of interest.

©2016 DIRIE, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.