eISSN: 2378-3176


Research Article Volume 12 Issue 2
Secretaria do Estado de Saúde, Serviço de Urologia do Hospital Regional da Asa Norte - Brasília - DF – Brasil
Correspondence: Wellington Alves Epaminondas, Secretaria do Estado de Saúde, Serviço de Urologia do Hospital Regional da Asa Norte - Brasília - DF – Brasil, Tel 55 61 98348 8878
Received: April 22, 2024 | Published: June 14, 2024
Citation: Epaminondas WA, Reis CMS, Novaes MRCG. Prevalence of lower tract urinary symptoms in a urology outpatient in the single health system of the federal district - Brazil. Urol Nephrol Open Access J. 2024;12(2):36-39. DOI: 10.15406/unoaj.2024.12.00353
Objective: To evaluate the prevalence of LUTS and it’s association with comorbidities such as hypertension, diabetes and smoking in individuals seen at a referral clinic in Urology in the Federal District.
Methods: Descriptive, cross-sectional and analytical study, conducted in 410 individuals aged 40 years or older, attended at the Urology outpatient clinic of the North Wing Regional Hospital, in Brasília, Brazil, on December 1 from 2018 to April 1, 2019. The questionnaires were applied to assess urinary symptoms.
Results: 64.15% had LUTS. In diabetics, the prevalence of LUTS had no statistical difference between the groups. HAS and LUTS were not associated, for this sample. The prevalence of LUTS increased in parallel with advancing age. 7.25% of the individuals were smokers.
Conclusion: The prevalence and severity LUTS increase with advancing age. LUTS has not a been associated with DM and SAH in this study.
Keywords: prostatic hyperplasia, noctury, diabetes, arterial hypertension, tabagism
LUTS, lower urinary tract symptoms; IPSS, international prostate score symptoms values; BPH, benign prostatic hyperplasia; QoL, quality of life; ED, erectile dysfunction; ICS, international continence society; ICF, informed consent form
Benign Prostatic Hyperplasia (BPH), defined as an abnormal and involuntary growth of the prostate gland, particularly the proliferation of epithelial cells and smooth muscle, is closely related to senility, being common in individuals over 50 years of age. With increasing age, in the age group between 80 and 90 years old, this probability increases to 90%.1,2 Lower Urinary Tract Symptoms, commonly referred to as LUTS (Lower Urinary Tract Symptons), is a well-established term that encompasses a variety of storage, emptying and post-voiding symptoms, with BPH being its main etiopathogenic factor in man.3 A The prevalence of LUTS/BPH increases with age, as does its degree of severity.4 The International Prostate Score Symptoms (IPSS) is a validated questionnaire for clinical assessment of subjects with BPH that assesses LUTS, with 7 questions quantified from 0 to 5, according to the frequency of symptoms and a question related to quality of life (QoL) of the subject. According to the points, symptoms are classified as mild (0 to 7), moderate (8 to 19) and severe (20 to 35). The IPSS/QL scores are used to plan and monitor the individual's treatment.5–8 Several conditions have been associated with LUTS/BPH, among the main ones, sleep disorders,9 DM10 and Erectile Dysfunction (ED).11
Nocturia, as defined by the International Continence Society (ICS), refers to the need to wake up at night to urinate. When this occurs more than 2 to 3 times a night, it becomes a factor that has a major impact on quality of life and sleep. Studies12 have shown that it is a common condition, with an incidence that increases in parallel with increasing age. Sleep interruption due to nocturia leads to a reduction in the number of hours of uninterrupted sleep, with a deterioration in quality of life. Reducing this time and slow wave sleep can lead to tiredness and discomfort. Masushita et al.,13 analyzed the sleep quality of patients over 65 years old, with nocturia, using the IPSS to assess urinary symptoms and uroflowmetry to measure urinary flow objectively. To analyze sleep quality, they used the electroencephalogram for three consecutive nights for each participant. They concluded that, in the elderly, sleep quality is related to the function of the lower urinary tract; Less severe LUTS, greater urinary flow and longer slow wave sleep time are associated with better sleep quality. In the REDUCE study, Branche et al.,9 showed that the worst results regarding sleep quality were related to greater development of LUTS in asymptomatic individuals and greater progression of LUTS in individuals who already had it. Such findings may also be related to the development of other comorbidities, such as obesity and DM.
In the study called LUTS Brasil, Soler et al.,14 evaluated the incidence of various urinary symptoms in men and women and showed that urinary frequency and nocturia were the most prevalent symptoms. Therefore, the investigation and treatment of ED and LUTS becomes very important and relevant. Despite the association proven in studies between these conditions, ED can have a low prevalence (underdiagnosed disease), when specifically it is not questioned during a consultation, whether in primary care or with a specialist. Baldwin, Ginsberg and Harkaway15 in a study of 500 men who sought a urologist for problems unrelated to erection, showed that 44% of them also suffered from this problem, but did not report it to the professional. Furthermore, of the men who did not complain of ED during their consultation with the urologist, 78% had also not discussed the problem with their general practitioners. The study demonstrates the prevalence of ED among men with other urological complaints.15 Given the lack of epidemiological data on the topic in the national territory (in Brazil), especially in the central-west region, it is imperative to know the profile of individuals treated in our region. Knowledge of these data will enable the identification and quantification of a problem that has not yet been directly addressed in our population and will assist in the implementation of specific actions to implement an outpatient clinic in Men's Health, aiming to provide better care for these individuals. The objective of the present study is to analyze the prevalence of LUTS and identify whether there is a correlation between LUTS symptoms and epidemiological variables such as age and comorbidities (SAH, DM and smoking) in individuals treated at the Urology outpatient clinic of the Hospital Regional da Asa Norte in the period from February 1, 2019 to June 1, 2019.16,17
Method
Observational cross-sectional study in which validated questionnaires for LUTS (International Prostate Symptons Score - IPSS) was applied to individuals aged 40 years or over, at the Urology outpatient clinic of the Hospital Regional da Asa Norte (HRAN) on December 1 from 2018 to April 1, 2019, according to the inclusion and exclusion criteria and evaluated according to clinical criteria. The study was analyzed and approved by the Research Ethics Committee of ESCS/FEPECS/SES/DF.
Inclusion criteria
Male individuals aged 40 years or over attended an outpatient consultation in the Urology sector - HRAN who signed the informed consent form (ICF) and responded to the questionnaires applied in the study.
Exclusion criteria
Patients with prostate adenocarcinoma (PCA) undergoing some therapeutic modality with the possibility of affecting the erection mechanism (surgery, radiotherapy treatment, brachytherapy treatment or hormone therapy); patients with benign prostatic hyperplasia (BPH) previously submitted to drug or surgical treatments; and/or those who refused to respond to the questionnaire administered and consent to the study by signing the ICF.
The validated questionnaire27,28,29,30,41,42 IPSS (International Prostate Symptons Score) for urinary symptoms were applied to 410 individuals who answered the data collection questionnaires applied sequentially in an outpatient consultation at the Urology unit of North Wing Regional Hospital.
Lower urinary tract symptoms (LUTS) were classified into three levels according to the IPSS, where:
0 to 7: Mild;
8 to 19: Moderate;
20 or more: Severe.
To facilitate understanding and data analysis, cases classified as “Mild” symptoms were considered normal. In clinical practice, given that the IPSS questionnaire does not include the “normal” category, individuals classified as “mild” are considered as such, due to the fact that the complaints do not cause changes in quality of life, and do not require therapeutic intervention.
Statistical analysis
Microsoft Excel software was used to tabulate data, produce figures and tables containing frequencies and percentages whenever possible. For data analysis, the program R version 3.5.1 was used, and RStudio version 1.1.456 was used for descriptive statistics of the variables of interest (mean, minimum, maximum and standard deviation). To analyze the association between categorical variables (LUTS, DM and SAH), the Chi-Square test was used. The phi coefficient measured the association between two binary variables and ranges from 0 (absence of association) to 1 (strong association), and was used to complement the result of the Chi-Square test. To analyze the correlation between Age and IPSS score, Pearson's correlation coefficient, also called linear correlation, was used. To verify the association between smoking and LUTS, Fisher's exact test was used. In the research analyses, the significance of the results and rejection of the null hypothesis were considered: a confidence interval (CI = 95%) and p ≤ 0.05.
The average age found was 59.7 years, with a higher prevalence of individuals aged between 60 and 69 years Figure 1. Of the 410 research participants, 263 (64.15%) had LUTS Table 1.
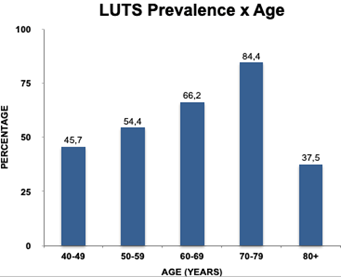
Figure 1 Distribution of the prevalence of Lower Urinary Tract Symptoms (LUTS) in each age group in the studied sample. Brasília, DF, 2020. p<0.05.
Source: Epaminondas, 2020.
|
Variables of the studied population |
(%) |
|
Lower Urinary Tract Symptoms |
64.15 |
|
Systemic Arterial Hypertension |
41.15 |
|
Diabetes Melitus |
16.31 |
|
Smoking |
7.25 |
|
LUTS** |
16.59 |
|
None# |
17.56 |
Table 1 Variables of the studied population
*ED: ED alone
**LUTS: LUTS alone
#None: Asymptomatic individuals
Source: Epaminondas, 2020.
To determine whether there is a correlation between the age variable and the IPSS variable, Pearson's linear correlation test was used. This test presented a value of p = 0.033, demonstrating that there is a linear correlation between age and IPSS. In Figure 1, an increase in the prevalence of LUTS of any degree with advancing age is observed. Figure 2 demonstrates the reduction in cases classified as Mild and an increase in Moderate cases. Severe cases rise after the age of 60, maintaining stable levels. The age group from 80 years old presented disparate data, probably due to the small number of individuals in this group. The Chi-Square test tested the association between diabetes and hyperplasia and obtained a p-value = 0.8586, corroborating what is shown in Figure 3 that the variables are not associated.
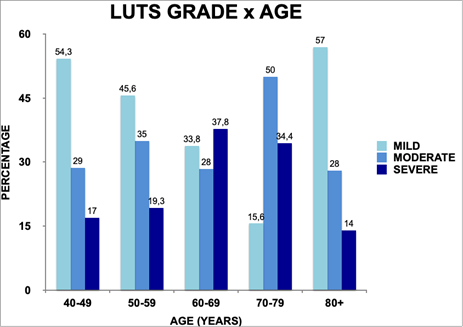
Figure 2 Distribution of prevalence and degree of LUTS in each age group in the studied sample. Brasília, DF, 2020.
Source: Epaminondas, 2020.
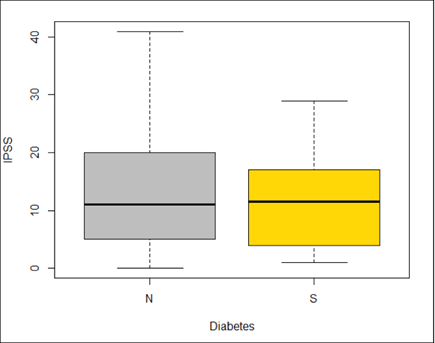
Figure 3 International Prostate Score Symptoms values (IPSS) in non-diabetic (N) and diabetic (S) individuals. p>0.05. Brasília, DF, 2020.
Source: Epaminondas, 2020.
Subtitle: N – non-diabetics; S – diabetics.
Figure 4 shows the distribution of hypertensive and non-hypertensive individuals in relation to the IPSS. Both groups have a median of 11, but hypertensive patients have an average IPSS of 14.45, while non-hypertensive patients have an average IPSS of 12.41. In order to find out whether there is an association between the variables, the Chi-Square test was used, which presented a p value = 0.1644, showing that HAS and LUTS are not associated, for this sample. Regarding smoking, it was observed that, in the studied sample, only 7.25% of individuals were smokers Table 2.
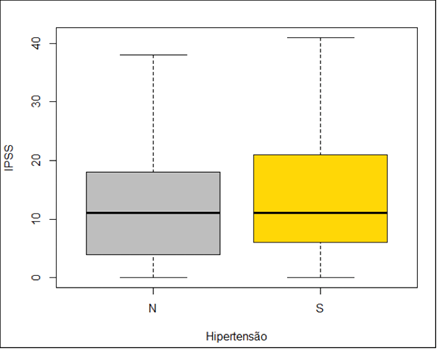
Figure 4 International Prostate Symptoms Score (IPSS) values in non-hypertensive (N) and hypertensive (S) individuals. Brasília, DF, 2020. p>0.05.
Source: Epaminondas, 2020.
Subtitle: N – non-hypertensive; S – hypertensive.
|
Tabagism |
Average |
Standard deviation |
Minimum |
First quartile |
Second quartile |
Third quartile |
Maximum |
|
Yes |
12.14 |
11.16 |
0 |
5 |
7.5 |
20.5 |
34 |
|
No |
12.12 |
9.8 |
0 |
4 |
10 |
18 |
41 |
Table 2 International Prostate Symptoms Score (IPSS) values in non-smokers (N) and smokers (S). Brasília, DF, 2020. p>0.05
Source: Epaminondas, 2020.
To check whether or not the variables are associated, Fisher's Exact test was applied. For the variables LUTS and smoking, the value of p = 0.5645 was highlighted, demonstrating that, for this sample, smoking is not associated with LUTS Figure 5.
The main cause of LUTS in men is BPH. This, in turn, has a histological diagnosis, characterized by the non-malignant proliferation of smooth muscle tissue and prostate epithelial cells. This proliferation can cause an increase in prostate volume, to the point of leading to obstruction in the prostatic urethra and bladder neck, leading to symptoms of LUTS. However, other mechanisms have been implicated in the process. Alpha-1 adrenergic receptors increase the tone of smooth muscle cells in the prostate capsule and bladder neck, which may contribute to the obstructive process.18,19 An increase in the incidence of LUTS and ED with advancing age has been reported. This was the scope of another study, to be published. This increase occurs in parallel with the degree of severity of both conditions. A study called “Multinational Survey of the Aging Male (MSAM – 7)” showed that the frequency of sexual activity is inversely proportional to age and degree of LUTS. They also found that LUTS was a stronger predictor of male sexual dysfunction than other risk factors.1,20 Kardasevic et al.,21 concluded that the IIEF-5 results are inversely proportional to prostate volume and, the larger the prostate, the higher the degree of ED. In the present study, 74% of LUTS patients concomitantly presented ED, which was corroborated by other studies.1,2,4,14
In this study, the low prevalence of LUTS in men aged 80 or more, occurred due to the small number of individuals in this group that completed the research. As mentioned before, the knowledge of these data will enable the identification and quantification of a problem that has not yet been directly addressed in our population and will assist in the implementation of specific actions to implement an outpatient clinic in Men's Health, aiming to provide better care for these individuals. In fact, the results of the research of this team resulted in the creation of a specific public department for Men’s Health in Brasília, Brazil. This is an independent department, associated to the Urology clinic.
The analysis of the results obtained allowed us to conclude that the population analyzed, users of the Unified Health System of the Federal District treated at the Urology outpatient clinic of the Hospital Regional da Asa Norte, presented the following characteristics:
None.
The authors declares that there are no conflicts of interest.

©2024 Epaminondas, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.