eISSN: 2378-3176


Review Article Volume 5 Issue 3
Department of urology, Military Hospital Avicenne, Morocco
Correspondence: Youness El Harrech, Department of urology, Military Hospital Avicenne, Marrakech, Morocco, Tel 00212-6-61326160
Received: June 29, 2017 | Published: September 18, 2017
Citation: Harrech YE, Ghoundale O, Touiti D (2017) Percutaneous Ureteral Dilations for Management of Uretero-Intestinal Anastomosis Stricture following Bricker Urinary Diversion. Urol Nephrol Open Access J 5(3): 00170. DOI: 10.15406/unoaj.2017.05.00170
Strictures of the uretero-intestinal anastomosis after urinary diversion following radical cystectomy are usually difficult to manage for both urologists and radiologists. Traditional surgery is the gold standard treatment. However, these strictures occur in oncologic patients, often old with concomitant morbidity. This makes less invasive option suitable. In this article we describe a mini invasive percutaneous option, safe and feasible under local anaesthesia, in an outpatient basis.\
Keywords: percutaneous surgery, endourology, ureterointestinal anastomosis, urinary diversion, radical cystectomy
Radical cystectomy is the standard treatment for muscle-invasive urothelial carcinoma of the bladder. After this procedure, urinary diversion is needed. Ileal conduit after anastomosis of the ureters in the bowel is considered the technique of choice of urinary diversion since its first description by Bricker in 1950.1 However, one of the most frequent complications to occur in these patients is the stricture of the uretero-intestinal anastomosis (UIA). Globally, the incidence of UIA stricture is up to 13%.2 It is usually asymptomatic and may lead to hydronephrosis, deterioration in renal function, urinary infection and kidney loss.
Management of strictures represents a big challenge for urologists and radiologists and both open approaches and endourological techniques were described. Open surgical revision remains the treatment of choice with a success rate of around 80%.3 However, the difficulty due to extensive intra-abdominal adhesions, the significant operative and post-operative morbidity (vascular injury, wound infection).4,5 leads to look for less invasive procedure with shorter hospital stay, especially that the patients are generally old with concomitant morbidity. Alternative options include endoscopic techniques such as balloon dilatation, endoscopic incision, stricture stenting, and endoscopic stricture incision combined with balloon dilatation. The aim of the present article is to describe a mini invasive percutaneous option, feasible under local anaesthesia, in an outpatient basis.
Operative technique
The patient is in a strict lateral position. After administration of 10 ml xylocaine, a kidney puncture is made under fluoroscopic guidance using a 22G Chiba needle (Figure 1A). Opacification of the collecting system permits to localise and observe the severity and length of the stricture. A second puncture is made using an 18G Chiba needle directly in the upper calyceal group, sometimes above the 12th rib. A hydrophilic 0.35-mm guide wire is introduced through the needle into the renal pelvis and ureter in antegrade fashion until it reaches and passes through the stricture (Figure 1B). The guide wire exits then through the ileostomy (Figure 1C). A 5F, 6F, 7F, and 8F ureteral stents are inserted on the guide in retrograde fashion to dilate the stenosis. Finally, a 7F single-J stent was placed and left in place (Figure 2). The patient remains under observation for 4hours and is then discharged. The stent is replaced every 9months in a retrograde manner through the ileostomy and under fluorescence guidance, on an outpatient basis.

Figure 1 A: Antegrade pyelography after kidney picture in a patient with solitary kidney; B: Guide wire through the ureterointestinal stricture passes through the stricture; C: the guidewire exits through the ileostomy.
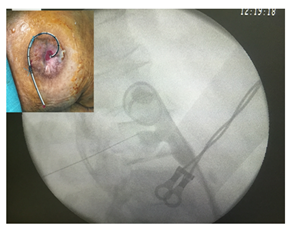
Figure 2 7F single-J stent placed in retrograde fashion through the ileal conduit and left in place.
Some tips are important. The initial use of a 22G needle is because it is less traumatic and allows only to opacify the pyleon. The guidewire in inserted through the 18G one. The puncture of the upper calyx is important to have a direct access to the ureter since they are usually aligned, so no use of “cobra” catheter is needed. Sometimes the stricture is very tight and it is impossible to cross it with the guidewire. In these cases, a 6Fr ureteral stent is inserted on the guide through the kidney until the stenosis, then injection of saline serum under pressure allows in some patients to dilate slightly the ureter and then to pass the guide. If it is impossible to cross the stricture, the other percutaneous or endoscopic procedures are not possible either and then open surgery is the only issue.
We operated in the last 3years 11 patients (17 kidneys) with UIA stricture after radical cystectomy. All of them underwent percutaneous repermeabilisation according to the technique described. All the procedures were successful with release of the symptoms and hydronephrosis. The creatinine levels in the patient with a solitary kidney decreased significantly. Peri-operative complications consisted of two cases of febrile urinary tract infection (Grade II of the Clavien Classification of Surgical Complications.6) managed with IV antibiotic. Even with the periodic replacement of the single J stent, all patients stated that their quality of life was not compromised. Percutaneous and endoscopic approaches were associated in different series with a 50% to 70% success rate.7–9
The techniques with incision of the anastomosis need general anaesthesia, the hospital stay is longer and the cost is higher than simple dilation. Furthermore, there is a risk of recurrence if a stent is not let in place. There are several advantages to managing UIA stricture with percutaneous repermeablisation. The procedure is minimally invasive, safe and feasible under local anaesthesia. Additionally, it offers the advantage of keeping a patent ureteral lumen. We think that our approach is appropriate as first-line treatment for ureterointestinal strictures following the Bricker technique.
None.
All authors declared there are no conflicts of interest.
None.

©2017 Harrech, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.