eISSN: 2378-3176


Case Report Volume 6 Issue 2
1Radiology, WEBIMAGEM, S
2Radiology, PREVENT SENIOR, Santos, S
3Radiology, Hospital Irm
4Radiology, BRASIL IMAGEM MEDICINA DIAGN
Correspondence: Marcio Luis Duarte, WEBIMAGEM, Avenida Marques de Sao Vicente 446, Sao Paulo, Brazil, Tel 55xx13981112799
Received: December 03, 2017 | Published: March 29, 2018
Citation: Duarte ML, Gelmini AYP, Souza GM, et al. Neuroblastoma: A correlation between radiologic methods. Urol Nephrol Open Access J. 2018;6(2):65–67. DOI: 10.15406/unoaj.2018.06.00205
Neuroblastoma is the most frequent solid extracranial neoplasia in children and is responsible for about 15% of all pediatric cancer deaths. It is an embryonal malignancy of the postganglionic sympathetic nervous system, which generally arises in the adrenal gland. 96% of cases occurs below 10 years age group and is slightly more common in Caucasian boys.
The primary renal neuroblastoma is rare, corresponding to 30-35% of all neuroblastomas. The diagnosis of neuroblastoma by imaging (ultrasound, CT scan, and MRI) features high accuracy and turns the medicine´s comprehension completely possible, and effective. Neuroblastoma signs and symptoms vary widely, depending on the size of the tumor, where it is, how far it has spread, and if the tumor cells secrete hormones. Here we report a case of a two-years-old male patient, who was hospitalized at first with a right hip pain and proceed the treatment of arthritis. After that, some suggestive symptoms started to be presented in addition to the radiology methods, turning the diagnosis possible and making the correct procedures.
Keywords: neuroblastoma/pathology, ultrasonography, adrenal tumors, raccoon eye
NBL, neuroblastoma; MRI, magnetic resonance imaging; CT scan, computed tomography; VIP, vasoactive intestinal peptide
Neuroblastoma (NBL) is the most frequent solid extracranial neoplasia in children and is responsible for about 15% of all pediatric cancer deaths.1 Ninety-six percent of cases occur before the age of 10 years and is slightly more common in Caucasian boys.1 The tumor arises from primitive neuroectodermal cells, which are derived from neural crest cells and can develop anywhere along the sympathetic chain, wherever sympathetic nervous tissue is found.1,2 Most cases are sporadic, but in 1 or 2% of cases there is a familial component and these tend to present even earlier, at a mean age of 9 months.2
Mostly arise from the abdomen – adrenal gland 48%; extra-adrenal – retroperitoneum 25% –, less frequently from the chest (16%) and rarely from the pelvis (3%) or the neck (3%).3 Childhood cancers, in general, are uncommon but are still the major disease-related death in children.4 The symptoms are vague and occasionally insidious like fever and weight loss, which are more common in patients with neuroblastoma – early diagnosis is critical for patient prognosis.4 The median age of presentation is approximately 18 months, 50% of cases are diagnosed before 1 year of age, and 80% are diagnosed before 5 years.5
Abdominal masses usually cause pain due to their mass effect, as well as abdominal distension.5 They often grow to a large size before causing problems, so a palpable mass on presentation is common.5 Abdominal masses can also compress renal vessels resulting in hypertension being a presenting feature.5 Thoracic NBL may present with airway compromise, scoliosis or as an incidental finding on chest x-ray.5 The biology of thoracic NBL tends to be less aggressive than abdominal disease and as such the prognosis tends to be more favorable.5
Paraneoplastic syndromes may be associated with the non-metastatic disease. One of these syndromes is opsomyoclonus, complicating 2-4% of presentations.5 The other is the excessive production of the vasoactive intestinal peptide (VIP) resulting in watery diarrhea.5 In addition to local disease, metastatic disease complicates 50% of all presentations. Common sites of metastases include liver, lymph nodes, and bone marrow.5 NBL can metastasize to the skull base and orbital floor resulting in periorbital ecchymosis and a so-called “raccoon eye” appearance.5
The diagnosis of NBL by imaging (ultrasound, CT scan, and MRI) features high accuracy and turns the medicine´s comprehension completely possible and effective.6 We report a case of adrenal neuroblastoma in a 2 years-old child with the description of imaging tests.
A two years-old male patient hospitalized for pain in the right hip for 4 months with lameness, worsening since then, until stop walking with orthopedic follow-up, being treated for arthritis. During hospitalization, his mother reported episodes of vomiting, diarrhea, abdominal distention, prostration, and tachycardia, denying abdominal pain. Denies previous medication pregnancy or postnatal complications.
At physical examination, appeared pale 2+/4+, mitral systolic murmur, abdominal distention with liver palpable to 4 cm from the right costal margin, spleen palpable to 3 cm from the left costal margin, painful deep palpation in the upper quadrants. Knees and left elbow enlarged without signs of inflammation with atrophy of the lower limbs, weighing about 11kg (moderate-severe malnutrition). There was a palpable lymph node in the right groin.
Blood count analysis showed leukocytosis (12800) and 153000 platelets. 7.6g/dl hemoglobin and 24.1% hematocrit. PCR: 34.32mg/L and ESR 76. Albumin: 3.45. Radiographic examination of the lower limbs visualized bone rarefaction of femurs, tibias, and fibulas (Figure 1).
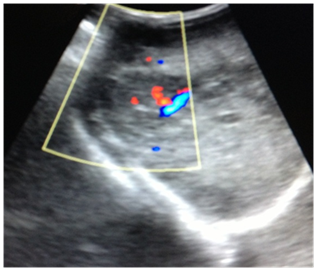
At abdominal ultrasonography, it was noted heterogeneous image, irregular, ill-defined, with Doppler vascularity in the right hepatic lobe (Figure 2). It is also visualized, at the right adrenal region a rounded image of imprecise limits, predominantly hypoechoic, with calcifications and Doppler vascularization, measuring about 3.7x2.1 cm in its largest axis (Figure 3).

Abdominal CT scan demonstrates multiple rounded formations, predominantly hypodense, well delineated, showing heterogeneous impregnation after the infusion of intravenous contrast, especially one in the right hepatic lobe measuring approximately 11.0x8.3x6.4cm. It was also noted left perihilar para-aortic lymphadenopathy and interaortocaval lymphadenopathy with a confluent aspect and an expansive formation, ovoid, heterogeneous, predominantly hypodense with calcifications inside, measuring about 3.7x2.2 cm in its major axis in the right adrenal (Figures 4A) (Figure 4B).
Myelogram shows infiltration by rosette tumor cells, suggesting neuroblastoma. After those tests, the chemotherapy started.

Ultrasonography is a method of choice in the assessment of the adrenal glands in neonates and young children.7 It is often the first line investigation in pediatrics, particularly for those presenting with an abdominal mass.5 Approximately half of the patients present with the localized or regional disease and 35% have regional lymph node spread at the time of diagnosis. Distant metastases are detected in 50% of patients at diagnosis and occur through both lymphatic and hematogenous routes. The most common sites include bone, bone marrow, and liver.8
The clinical presentation and symptoms of NBL depend on location. Symptoms of abdomen or pelvis location can be, constipation, distension, urinary retention, hypertension.8 If it is on presacral and paraspinal (includes abdominal and thoracic masses), symptoms of cord compression (urinary retention, paraplegia/paraparesis, clonus).8 The aim is to obtain a precise description of a primary tumor and its local spread, as soon as possible.9CT scans have been used in children since the mid-1970s, first for intracranial processes but soon after for thoracic and abdominal tumors as well.9 MRI was introduced for children in the early 1980s, again first for studies of the brain and soon after for chest, abdomen, and extremities.9 These techniques have been compared and their pros and cons well described in different clinical situations.9
The choice of techniques will depend on local conditions such as availability of MRI expertise and of general anesthesia for MRI, the site of the primary tumor and whether a chest CT scan is necessary for lung metastases. You also need to plan for tumor evaluation under treatment, and this is best done using the same technique. Due to the availability, cost, and non-invasiveness, ultrasound is often used for the assessment of the suprarenal areas in adolescents and adults with extra-adrenal tumors.8 Moreover, it is recommended in patients with arterial hypertension or hyperadrenalism or adrenal insufficiency, and in the monitoring of adrenal tumors diagnosed in computed tomography or magnetic resonance imaging as benign adenoma-like neoplasms. This examination enables the differentiation between a solid tumor and adrenal cysts, which are rarely encountered.8
Magnetic Resonance Imaging (MRI) should now be the cornerstone imaging modality for all primary neuroblastomas, whether in the neck, chest, abdomen or pelvis. MRI can easily assess the extent of disease, being superior to CT scan in assessing metastatic marrow disease, chest wall invasion and spinal canal involvement.5 On MRI, the tumor tends to have low signal on T1-weighted sequences with high signal on T2. Areas of calcification and hemorrhage can also be detected.5
NBL can demonstrate extension across the midline and into adjacent body cavities.5 One of the key defining features is the presence of calcifications, seen in 80-90% of CT scan studies.5 Despite their size and sometimes-aggressive nature, neuroblastoma tend to encase and displace structures rather than invade them. Vascular invasion is not a classic feature demonstrated on cross-sectional imaging.5
In situations where the abdominal CT scan demonstrates intratumoral calcifications, entrapment vessels in the tumor and/or tumor extension beyond the midline, large vessels and/or kidney displacement – the use of contrast is mandatory if there are no contraindications (Table 1). The tumor response to treatment is evaluated from preoperative therapy using similar methods to those who made the diagnosis, often in combination, to evaluate even the respectability of the tumor, until the postoperative period.9
|
Neuroblastoma |
X-RAY |
Plain films are non-specific for NBL and are largely unhelpful in the diagnostic pathway.5 |
Ultrasound |
NBL appear as solid, heterogeneous masses with calcification, but are rarely cystic on US.5 |
CT Scan |
Presents like a heterogeneous poorly delineated masses, with calcification seen in 80-90%.5 |
MRI |
NBL tends to have low signal on T1-weighted sequences with high signal on T2.5 |
Table 1 Radiologic findings of Neuroblastoma tumor
The written informed consent of the patient was obtained, for the publication of her case.
Not applicable.
The authors declare that there is no conflict of interests regarding the publication of this paper.

©2018 Duarte, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.