eISSN: 2378-3176


Case Report Volume 1 Issue 1
1Department of Urology, Sultan Qaboos Hospital, Salalah, Oman
2Radiologist, Sultan Qaboos Hospital, Salalah, Oman
Correspondence: Logesan Dhinakar, Department of Urology, Sultan Qaboos Hospital, Salalah, Oman, Tel 00968-99484157, Fax 00968-23216040
Received: August 10, 2014 | Published: October 30, 2014
Citation: Dhinakar L, Dhinakar M. Modified anatrophic nephrolithotomy “a salalah experience”. Urol Nephrol Open Access J. 2014;1(1):33-36. DOI: 10.15406/unoaj.2014.01.00008
Anatrophic Nephrolithotomy is a major open Transrenal surgery of the Kidney to extract a Complete Staghorn Calculus of the Kidney in selected situations. The original procedure described by Boyce involved complex dissection of the renal vasculature with selective cannulation and perfusion of the posterior segmental artery with methylene blue. We are presenting our experience of a modified approach of the same procedure, thereby reducing the ischemic time and the morbidity of the original procedure. These modifications have been described in literature and we are presenting our experience of the same with comparable results. It is a highly skilled procedure and a proper case selection, knowledge of the Renal vascular anatomy, adequate surface cooling, is absolutely essential to have a successful outcome devoid of major immediate complications like gross bleeding and hematuria, and delayed complications like Ischemic necrosis with fistula formation and renal Ischemic atrophy. Our complications were easily manageable adopting conservative methods.
Keywords: anatrophic, staghorn, nephrolithotomy
ESWL, extracorporeal shockwave lithotripsy; PCNL, percutaneous nephrolithotomy; PDS, polydioxanone (synthetic absorbable suture material); VUJ, vesico ureteric junction; KUB, kidney, ureter, bladder; RGP, retrograde pyelogram; IVU, intravenous urogram; PO, post operative; USG, ultra sonogram
Anatrophic Nephrolithotomy is a major open trans renal surgery not too infrequently performed for a large branched stag horn calculus of the Kidney. The procedure involves adequate dissection of the kidney and its vascular supply, clamping the renal artery, surface cooling of the kidney with ice slush and performing a posterior capsulotomy and a blunt nephrotomy in a relatively a vascular plane directly leading to the collecting system, opening the collecting system, delivering the calculus, closing the collecting system and capsule and finally re-establishing the arterial flow. This is a case report of one such patient with a complete Staghorn calculus who underwent a modified Anatrophic Nephrolithotomy at our hospital with a successful outcome in the form of complete stone clearance and a normally functioning kidney post operatively with no complications.
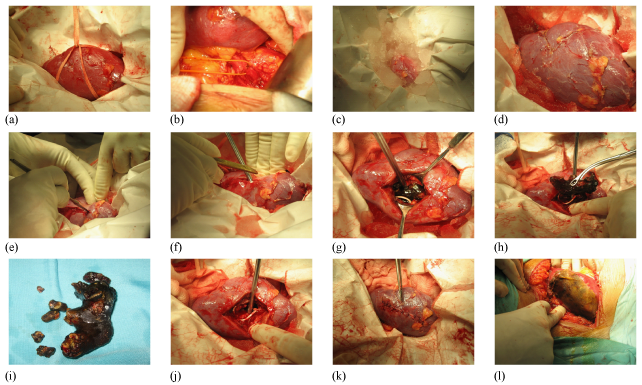
A 40year old male patient was admitted with symptoms of Bi lateral loin pain. Radiological investigations revealed a 1.2cm calculus in the left lower ureter with hydroureteronephrosis and a complete branched Staghorn calculus occupying the entire collecting system with moderate hydronephrosis in the right kidney (Figure 1a & 1b). Routine pre operative investigations including Renal function test and metabolic work up for stone disease was normal. Urine routine showed microscopic haematuria and culture was negative. The patient was first taken up for Ureteroscopy for the left lower Ureteric calculus. The stone was fragmented using Lithoclast and removed and a Double ‘J’ stent was inserted. Two weeks later he was taken up for a Modified Anatrophic Nephrolithotomy for the Right Staghorn Calculus. A preliminary Cystoscopy, RGP and a double J stent insertion was done on the right side. The left side stent previously placed during Ureteroscopy was removed. The patient was placed in the left lateral position and a Rt. loin incision made through the bed of 11th rib excising the terminal segment of the rib. The Gerota’s fascia was opened and the Right Kidney was mobilized completely (Figure 2a). The Renal artery was carefully dissected well away from the hilum to avoid arterial spasm that may occur during dissection close to hilum of the kidney and taped with Vesiloop (Figure 2b). Ice slush was prepared from frozen Ringer lactate solution. A water proof sterile sheet was taken and a central opening made to allow only the kidney to pass through. 100ml of 20% Mannitol was infused quickly. The kidney was turgid and there was a good urine flow. The artery was clamped with an traumatic bulldog clamp. The water proof sheet was placed immediately in the wound and the kidney brought out through the central opening made previously. The prepared ice slush was placed on the water proof sheet covering the entire kidney (Figure 2c). The kidney was cooled externally for 10minutes. After removing part of the ice slush the convex surface of the kidney was exposed. The Renal capsule was incised along the long axis of the kidney 2cm posterior to the convex border of the kidney (Figure 2d & 2e). The renal cortex was bluntly dissected with the handle of the knife towards the collecting system. One small vein that was encountered was suture ligated. The collecting system was opened along its long axis and extended at right angles into the anterior and posterior calyces to completely free the stone. The Staghorn calculus was gently dissected free and removed (Figure 2f & 2g). A small bit of the stone was sent for culture which subsequently was reported as sterile. C-Arm image intensifier was used to assess completeness of stone removal. It showed residual stones in a few calyces. These small calculi were washed out with cold saline with the help of a catheter. Completeness of removal was checked again by C- Arm and also by intra operative Flexible Nephroscopy. The upper coil of the DJ Stent was seen in position in the R Renal pelvis. After ensuring complete stone clearance the renal cortex was loosely approximated with three, 3‘O’ PDS sutures and the capsule closed with interrupted 3‘O’ Vicryl sutures (Figure 2h). The artery clamp was released. The kidney perfused immediately, became pink and turgid with a brisk urine flow seen in the ureter (Figure 2i). There was minimal ooze from the surface which stopped on placing a strip of Surgicel. There was no urine leak from the Nephrotomy site. The total renal ischemia time was 52minutes. The wound was closed with a tube drain after securing haemostasis. In the post operative period there was mild haematuria which lasted for two days. The patient recovered well without any immediate or delayed complications of the procedure. Sutures were removed on the 10th PO day. On the 14th PO day a plain X-ray KUB and an IVU was done. IVU showed bilaterally normally functioning kidneys. There was no distortion, obstruction or contrast leakage on the Right side and the double J stent was in situ (Figure 2J, 2k & 2l). USG confirmed no residual stone in the Right kidney. The patient was subsequently taken up 3weeks later for Flexi Cystoscopy under Local Anesthesia and the Right Double J stent was removed. Patient was asymptomatic and had another USG a week later to confirm that all was well. Patient was stone free. Subsequently a total of Nine Anatrophic Nephrolithotomy has been done so far with comparable results. Complete stone clearance was achieved in 7 cases. Complications in our series-: One patient developed haematuria on the 2nd post operative day which required blood transfusion, but settled with conservative management. All other patients were managed without any transfusion. One patient developed urine leak from the wound in spite of the DJ stent being in situ on the 5th post operative day. Ultrasound revealed a Urinoma posterior to the Kidney. A tube drain was placed into the collection using Ultrasound guidance, for controlled drainage and left in situ for 2weeks. The leak settled without any further intervention and the drain and the DJ stent were subsequently removed. One patient developed wound infection. Cultures were performed and patient treated with appropriate parenteral antibiotics. The wound infection settled and secondary suturing of the wound was performed subsequently. Two patients had small residual calculi which were missed during the initial procedure. These two patients had Flexi Ureteroscopy after 3months and stone clearance achieved (Figure 3).
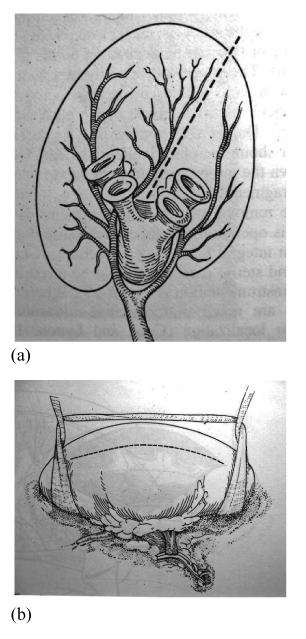
The management of large renal stones occupying the entire collecting system of a Kidney (Staghorn calculus) is a difficult proposition. In the modern era of stone management methods like ESWL and PCNL predominate and are also welcome by patients due to lesser morbidity and quicker recovery. Though these procedures are good and should be the first line of treatment in majority of patients, there are some limitations to these procedures. In cases of multiple large renal calculi and staghorn calculus, ESWL and PCNL may both be necessary to give stone clearance. The patients will require multiple sittings of ESWL with or without PCNL and a protracted convalescence with less than complete stone clearance and the attendant morbidity of passing the stone fragments per via naturalis, in cases where ESWL is used alone. Also anatomical abnormalities like infundibular stenosis cannot be corrected and this leads incomplete removal and early recurrence in such a circumstance open surgical removal of the calculus still has a role to play in selected cases.1 Patients with Staghorn calculus of the kidney commonly present with loin pain, haematuria, fever or in some cases may be asymptomatic. Chronic Urinary tract infection is common in these patients and the typical organisms grown are the urea splitting organisms like Proteus, Klebsiella, Providencia and Pseudomonas. The diagnosis is established by Plain and Contrast radiography and in cases of a Large and almost Radiolucent Staghorn calculus, a spiral Non Contrast CT scan may be necessary to establish the diagnosis. A complete metabolic work up is necessary in the form of Serum and urine Calcium, Phosphorus, Uric acid, Creatinine, Liver function tests including Serum Alkaline Phosphatase and electrolytes and in suspected cases of Hyperoxaluria, Hyperuricaemia or Cystinuria, a serum as well as 24hour urine excretion of Oxalate, Uric acid and Cystine is done. If Hyper Parathyroidism is suspected then a Serum Parathormone and an Ultrasound examination of the neck is done. Anatrophic Nephrolithotomy is a procedure which is done for a complete Staghorn Calculus of the Kidney. It was first described by Smith and Boyce.2 The operation they described was based on the principle of placing the Nephrotomy incision through a plane of the kidney that is relatively a vascular. Thus this approach would avoid damage to the renal vasculature and thereby prevent atrophy of the Kidney, hence the term ‘Anatrophic’. The operation makes use of the fact that the anterior and posterior segments of the kidney is supplied separately by the anterior (apical, upper, middle & lower) and posterior segmental arteries with practically no cross anastomosis between the two segments of the kidney (Figure 4a).Thus the nephrotomy is placed in a plane between the anterior and posterior segmental arteries of the main Renal artery. This a vascular plane was described by Brodel and the surface marking on the kidney is a line drawn on the long axis of the kidney 2cms posterior to the convex border of the kidney not encroaching on to the poles of the kidney (Figure 4b). An Intra operative Doppler probe has been found to be useful during nephrotomy to identify the vessels and prevent injury. The operation also involves reconstruction of the distorted and narrowed part of the collecting system like Calycoplasty, Calyorrhaphy, Infundibuloplasty, Calicocalicostomy etc, thus improving drainage, reducing the likelihood of recurrent infection and stone recurrence.3 An important part of the procedure involves cooling the kidney to reduce the core temperature to 5-10degrees Celsius. This is absolutely necessary as the maximum warm ischemia time of the kidney is only 20minutes. By surface cooling and thereby reducing the core temperature, the allowed ischemia time is increased to 60-75minutes which is adequate to do the procedure without causing permanent ischemic damage to the kidney.4 The ischemic insult is further reduced by infusing 25gms of Mannitol, prior to clamping the renal artery. Mannitol infusion protects the ischemic kidney by promoting post ischemic diuresis and prevents formation of intra tubular ice crystals by increasing the osmolarity of the glomerular filtrate. The immediate complications of the procedure described are bleeding, both intra and post operative, urinary leak, and pulmonary complications like pulmonary embolism and atelectasis. The delayed complications include infection, secondary hemorrhage and recurrence of calculus. Rarely Intrarenal Arteriovenous fistulae formation presenting as delayed haematuria has been observed. In our series there were some minor complications which were managed conservatively. The procedure adopted in our case is a modified one as compared to the original description of Smith and Boyce. These modifications have been described in the literature,5 and were adopted in our cases to reduce the operating time and thereby reducing the ischemia time and subsequent renal injury, and also to reduce complications.
Preliminary Cystoscopy, and stent placement was done. It was done to have a patent ureter always and even if small stone fragments migrate down it may not obstruct the kidney leading to disruption of the collecting system and the nephrotomy wound. In the Boyce procedure antegrade stenting is done following stone removal. A preliminary Cystoscopy and placement of stent greatly improves the outcome as a patent ureter is ensured. Though at times it may be difficult to pass the stent into the renal pelvis in a snuggly fitting staghorn calculus, positioning the stent just below the PUJ is adequate as it can be easily manipulated into the renal pelvis after removing the calculus. Though the total operating time is a little prolonged it still gives the surgeon the confidence to open the kidney as post operatively an uninterrupted urine flow down the ureter is ensured and the risk of Nephrotomy dehiscence is negligible. Ante-grade placement of the stent intra operatively as done in the Boyce procedure can be fraught with difficulties as sometimes it is difficult to negotiate the VUJ.
Dissection of the main renal artery was done away from the hilum thus preventing arterial spasm and ischemic insult to the kidney.6 In the Boyce procedure the posterior segmental vessel is dissected and preliminary temporary clamping of posterior segmental artery and giving intravenous methylene blue to delineate the a vascular plane between the blanched posterior segment and the blue anterior segment due to methylene blue coloration of that segment was adopted. This extended procedure was found to be unnecessary and dangerous as it may lead to arterial dissection and subsequent thrombosis. It also increases the ischemic time and morbidity.
As there was no infundibular stenosis and complete stone removal, the collecting system was not closed formally except for a few loosely placed sutures in the renal parenchyma just to approximate the cortex. The Renal capsule was closed securely. This was done to reduce the overall ischemic time of the kidney. In the Boyce procedure meticulous closure of the collecting system is employed.7 In our case there was no post operative urinary leak as demonstrated by the post operative IVU which showed a normally appearing pelvicalyceal system with no leakage of contrast. This method can be adopted in selected situations especially when no abnormality has been detected preoperatively in the pelvicalyceal system of the affected kidney, with overall reduction of the ischemic time. The stone clearance rate described in literature in a series of 26 cases from the Armed forces Hospital, Muscat5 in which this procedure was done was around 85-88%. Another series comparing the results of PCNL and Open surgery had a stone clearance rate of 82% in 45 cases for whom open surgery was done for complete staghorn calculus.8 We had complete stone clearance in 7 out of the 9 cases as demonstrated by X-ray and Ultrasound. The post operative renal function as assessed by IVU had done 2weeks after surgery was normal in 6 cases that IVU was performed. The other three cases refused further evaluation as they were well. In the series at the Armed forces Hospital, Muscat, the post operative renal function was assessed by Radio isotope scan5 done pre operatively and 6months after surgery. Their results were, 55% of the cases had no change in renal function, 32% improved and a small percentage worsened.
Anatrophic Nephrolithotomy is a major open renal surgery and if done, adopting the standard precautions and with a sound knowledge of renal vascular anatomy, can serve as an alternate to the modern methods in selected situations. It can give complete stone clearance and also can be used to correct anatomical deformities in the collecting system of the kidney like infundibular stenosis which if not corrected may lead to early recurrence of stone formation.9 Also lurking infection due to urea splitting organism like Proteus which are invariable seen in a Struvite calculus ( commonly presents as a staghorn calculus), can be better eradicated during open surgery than other methods because of adequate flushing of the collecting system that is done during open surgery and complete stone clearance. The morbidity of a loin incision and a somewhat delayed recovery must be weighed against the need for multiple procedures with a similar delayed recovery, if the modern methods are adopted. In centers where ESWL or PCNL is not available resorting to this procedure by an experienced Urologist yields very good results. Hence with adequate training to perform this intricate open surgery, complete stone clearance with reduced recurrence rates have been possible in a number of centers which still perform this surgery.
None.

©2014 Dhinakar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.