eISSN: 2378-3176


Case Report Volume 3 Issue 5
Department of Urology, Colchester University Hospitals NHS Trust, UK
Correspondence: Pandian SS, Department of Urology, Colchester University Hospitals NHS Trust, UK
Received: July 14, 2016 | Published: September 13, 2016
Citation: Pandian SS, Rix GH, Jayasooriya N, Conn P, Cano D (2016) Melanosis of the Urinary Bladder – A Case Report and Review of the Literature. Urol Nephrol Open Access J 3(5): 00093. DOI: 10.15406/unoaj.2016.03.00093
This is a rare case report of Melanosis of the urinary bladder and review of the literature around it. The case is a male patient with a history of visible haematuria who at cystoscopy revealed several small, evenly pigmented, flat, brown/black lesions, which on biopsy proved to be melanosis of the urinary bladder. Representative cystoscopy and histopathology images are included. Melanosis of the bladder is a distinct benign histopathological finding and is not a premalignant condition for malignant melanoma of the bladder. There is little evidence in the literature to guide its specific management. Review of literature searched through medline, pubmed and Cochrane library, using key words melanosis, urinary bladder, melanin, melanoma, melanuria and malignancy, form part of the discussion.
Keywords: Melanosis; Melanin; Urinary bladder; Melanocytes; Melanoma; Melanuria; Malignancy
Melanosis of the urinary bladder is very rare. It is characterized by the deposition of melanin within the vesical urothelium and/or lamina propria without the presence of melanocytes [1]. It is a distinct pathological entity in its own right and is not directly related to other melanotic lesions such as melanocytic naevus, lentigo maligna or malignant melanoma. At present, melanosis of the bladder is of uncertain clinical significance and there are no clear guidelines for its management. To our knowledge, so far only 7 such cases are reported in the world literature [2-6]. We report the first case from the United Kingdom.
A 75 year old Caucasian male presented with a history of 3 episodes of painless, frank haematuria. There were no other lower urinary tract symptoms. He was a known systemic hypertensive on treatment, with a concomitant giant right middle cerebral artery aneurysm under conservative management. There was no history of malignant melanoma at any site. He had undergone excision of a benign melanocytic naevus from his glabella 10 years previously. He was a non-smoker and there was no history of any urinary tract malignancy in him or his family. He was pale-skinned and had no abnormalities of pigmentation such as vitiligo or excessive numbers of skin naevi.
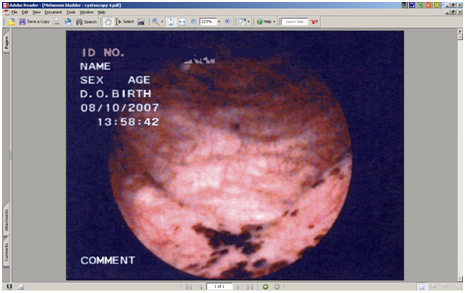
Clinical examination and radiological investigations including and ultrasound scan and a computerised axial tomogram scan (with intravenous contrast) of his urinary system were unremarkable. Routine blood tests including full blood count, urea, electrolytes and prostate specific antigen were normal. Urinalysis had revealed microscopic haematuria. There was no evidence of infection on urinalysis, mid-stream urine microscopy and culture. Urine cytology x 3 were normal. Flexible cystoscopy revealed several small, evenly pigmented, flat, brown/black lesions, measuring between 3 and 5mm in diameter, scattered throughout the bladder mucosa, with the greatest density and size of the lesions at the bladder base (Figure 1). Cold cup and subsequent resection biopsies were undertaken. There was no suggestion that the prostate could have been the source of his haematuria. Histopathology of both specimens showed many granules of golden brown pigment of varying size in the urothelial cells and within histiocytes in the underlying lamina propria (Figures 2&3).
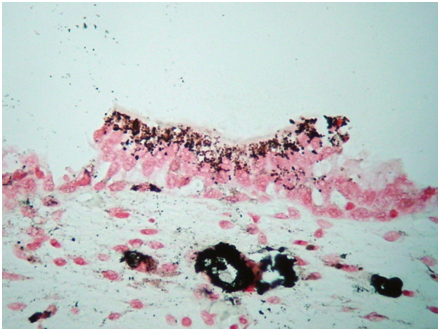
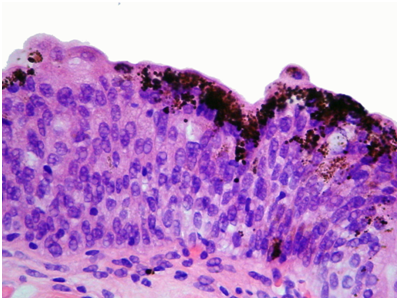
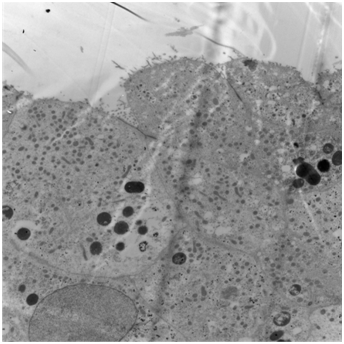
No melanocytes were visible on routine staining with haematoxylin and eosin or with the immunoperoxidase stain S100 or with electron microscopy. The urothelium was not dysplastic. Some areas had metaplastic changes of cystitis cystica. The pigment was negative with Perl’s and with periodic acid Schiff (PAS) stains, excluding haemosiderin and lipofuscin respectively. Masson stain was positive, and bleaching removed the pigment, together indicating that the pigment was melanin. Electron microscopy showed that the pigment was bound in lysosomes and that there were no melanosomes (Figure 4). The final histopathological diagnosis was melanosis of the urinary bladder.
The natural history of genito-urinary melanosis is uncertain because of the rarity of such lesions. The cases of reported melanosis of the urinary bladder have been predominantly in Caucasians. They have been reported in both men and women aged between 43-86 years. They have all been found incidentally during cystoscopy performed for diverse indications including haematuria, cystitis and other lower urinary tract symptoms. Their appearances have been generally described as multiple scattered brown or black irregularly shaped spots in the bladder mucosa. One case described concomitant white areas, which on biopsy revealed the presence of squamous metaplasia [4]. The specks of pigmentation have been often noted to have a wide distribution within the bladder including the lateral walls and base. The final diagnosis has been based on histochemical identification of the presence of melanin pigment within the urothelial cells using stains such as Masson, Lillie (4), Dopa (9) and Fontana Silver (3). It has also been reported that the melanin pigment disappears upon bleaching with potassium permanganate (3). Perl’s stain can be used to exclude hemosiderin pigment and PAS stain to exclude lipofuscin pigment, both of which can easily mimic melanin.
However, the presence of melanocytes, usually characterized by positivity to immunoperoxidase stains such as S-100 and / or HMB-45 was not consistently observed in all the reported cases. No concurrent dysplasia or malignancy was seen in any of these cases. The demonstration of melanosis in the absence of melanocytes is the key feature in this case report. It appears that the urothelial cells have taken up melanin within lysosomes, rather than having it delivered to them via dendritic melanocytes, which is the usual process in normal skin, for example. The source of the pigment is unknown. The principal question raised in previous reports is whether melanosis of the bladder is essentially a benign condition or whether it is a pre-malignant harbinger of vesical malignant melanoma. The lack of melanocytes would suggest that this is a benign condition.
In the epithelium of the oral cavity, oesophagus, vulva and penis it is normal to find melanocytes, from which malignant melanomas arise in occasional patients [7,8]. However, in the genitourinary tract, malignant melanoma is very rarely a primary disease and deposits of melanoma in these organs are usually considered to be metastatic until proven otherwise, with or without a previously known history of primary melanoma at its usual sites such as the skin. Metastatic malignant melanoma within the genitourinary tract is relatively common and the lesions are usually asymptomatic being discovered most frequently post mortem [9]. Four cases of primary malignant melanoma of the urinary bladder have been described. In three, the tumours found were not associated with widespread melanosis [10-12]. In one [13] melanosis of the bladder was associated with multiple melanomas, each arising within a melanotic area. Melanocytes were present. Of the other 6 cases of melanosis in the literature, 5 are reports on presentation with no long-term follow-up. One case (5) was followed for 10 years without malignant progression.
Diffuse melanosis with melanuria is a rare complication of metastatic malignant melanoma that is associated with a very poor prognosis. A patient suffering from a metastasizing malignant melanoma of the skin developed diffuse melanosis of the skin and melanuria a few weeks before death occurred [14] One can speculate that melanin in the urine of this origin could be taken up secondarily by the urothelial cells and mucosal macrophages. The melanin load would presumably have to be fairly high and uptake would presumably be homogenous, so this would not explain the focal melanocytic patches in our case.
Given the paucity of evidence in the literature regarding melanosis of the bladder, it is difficult to make suggestions regarding the best way to clinically manage this condition. As there is no evidence in our case of melanocytic proliferation in the bladder there is nothing to suggest that surveillance with cystoscopic follow-up would be of any benefit (other than to confirm that nothing has changed), nor is there likely to be any benefit from transurethral resection/ablation of these lesions. The case that was followed-up for 10 years (5) has also not suggested the need for long-term cystoscopy surveillance. There is certainly nothing to indicate a radical procedure such as cystectomy. The source of the melanin in the urothelial cells remains mysterious but there is nothing in this case to suggest a sinister process.
The demonstration of melanosis, which is deposition of melanin pigment in the vesical epithelium/laminapropria, in the absence of melanocytes is the key feature in this case report. The source of the pigment is unknown. The principal question raised in previous reports is whether melanosis of the bladder is essentially a benign condition or whether it is a pre-malignant condition for vesical malignant melanoma? The lack of melanocytes would suggest that this is a benign condition. Given the limited evidence in the current literature regarding melanosis of the bladder, it is difficult to make suggestions regarding the best way to clinically manage this condition.

©2016 Pandian, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.