eISSN: 2378-3176


Clinical Report Volume 12 Issue 1
1Veltischev research and clinical institute for pediatrics and pediatric surgery of the Pirogov Russian National research medical university, Moscow, Russia
2The State education institution of higher professional training the first Sechenov Moscow State medical University under ministry of health of the Russian Federation, Moscow, Russia
Correspondence: Natalia M Zaikova, Veltischev research and clinical institute for pediatrics and pediatric surgery of the Pirogov Russian National research medical university, Moscow, Russia, Tel +79645299049
Received: December 18, 2023 | Published: January 15, 2024
Citation: Zaikova NM, Mikhalkova DY, Dlin VV, et al. Development of steroid-resistant nephrotic syndrome in a child with CAKUT. Urol Nephrol Open Access J. 2024;12(1):1-5. DOI: 10.15406/unoaj.2024.12.00345
Introduction: One of the congenital anomalies of the kidneys and urinary tracts (CAKUT) is renal hypodysplasia/aplasia type 3 (PHDA3), caused by pathogenic variants in the GREB1L gene not associated with steroid-resistant nephrotic syndrome (SRNS). PGDA3 leads to chronic kidney disease (CKD). Variants in the UMOD gene associated with autosomal dominant tubulointerstitial kidney disease (ATKD-UMOD) also lead to CKD. The association of the GREB1L/UMOD genes with SRNS has not been previously described.
Purpose of the article: To demonstrate a rare clinical case of SRNS in a child with CAKUT.
Patients and methods: A patient with CAKUT in the form of PGDA3 and ADTBP-UMOD is observed in the department of nephrology for 2 years. Post-infectious development of SRNS required a revision of the genetic screening.
Results: On the whole-genome sequencing were found a variability in the genes that cause CAKUT, with no candidate genes for SRNS.
Conclusion: The described case stands out with clinical polymorphism of CAKUT and the variability of UMOD and GREB1L gene variants not associated with the development of SRNS. Infectious etiology of the development of SRNS is assumed. The patient has an intensive development of CKD stage 4, requiring a long-term follow-up in dynamics.
Keywords: children, renal failure, GREB-1L, renal aplasia, CAKUT syndrome, renal developmental anomalies, autosomal dominant tubular renal disease; BP, blood pressure
CAUT, congenital anomalies kidney and urinary tract; RA, renal agenesis; CKD, chronic kidney disease; ADTKD1, autosomal dominant tubulointerstitial kidney disease type 1; SRNS, steroid-resistant nephrotic syndrome; RHDA3, renal hypodysplasia/aplasia, type 3; Er, erythrocytes; PS, prednisolone; SRNS, steroid-resistant nephrotic syndrome; MMF; mycophenolate mofetil; CRF, chronic renal failure; AIM, anterior intermediate mesoderm; WD, wolffian duct; UB, ureteric bud; CD, collecting duct; PIM, posterior intermediate mesoderm; MM, metanephric mesenchyme; CM, cap mesenchyme; PTA, pre-tubular aggregate; RV, renal vesicle; CSB, comma shaped body; SSB, S shaped body; RHDA3, renal hypodysplasia/aplasia-3; RAR, retinoic acid coactivator; AH, arterial hypertension; URA, unilateral renal aplasia; FSGS, focal segmental glomerulosclerosis
Congenital anomalies kidney and urinary tract (CAUT) are leading among other developmental anomalies in the world. One of the most severe manifestations of CAKUT is renal agenesis (RA).1 It is known that pathogenic variants in the GREB1L gene can lead to renal hypodysplasia/aplasia, type 3 (RHDA3), however, this disease may be characterized by incomplete penetrance. Pathogenic variants of the UMOD gene are a common cause of chronic kidney disease (CKD) and are associated with the development of autosomal dominant tubulointerstitial kidney disease type 1 (ADTKD1), familial hyperuricemic nephropathy and cystic kidney disease. However, the association of these genes with steroid-resistant nephrotic syndrome (SRNS) has not been previously reported.
Objective: To present a rare clinical case of steroid-resistant nephrotic syndrome development in child with CAKUT.
A girl G.Z. 3 years old (born in 2019) from healthy unrelated parents is observed in the Department of Nephrology at the Veltischev Research and Clinical Institute for Pediatrics and Рediatric surgery of the Pirogov Russian National Research Medical University (hereinafter the Institute) from 1 year 4 months. From the anamnesis of life, it is known that the child from the 4th pregnancy (in vitro fertilization), which took place against the background of toxicosis, suffered ARVI in the first trimester. At the 20th week of gestation, during antenatal screening, hypoplasia of both kidneys was detected for the first time, and already at the 30th week, according to fetal ultrasound examination, agenesis of the left kidney was confirmed. The first urgent delivery at 38 weeks of gestation. At birth, body weight deficit (weight – 2430 g, height – 49 cm), APGAR 6-7. On the 5th day of life, according to ultrasound examination of the kidneys, agenesis of the left kidney was confirmed, single cysts in the right kidney were identified. Laboratory tests were not carried out.
For the first time, at the age of 1 year 4 months, the girl was hospitalized in the nephrology department of the Institute. On examination, the weight is 10 kg (less than 3%), height 79 cm (50-75%), increased blood pressure (BP) by one-time measurements (above 95%). The examination revealed a glomerular function decrease (creatinine 65 mmol/l; eGFR 50 ml/min / 1.73 m2), hypercalcemia (Ca – 2.76 mmol/L), alkaline phosphatase in normal (alkaline phosphatase - 365 IU/L), signs of moderate secondary hyperparathyroidism (PTH – 76.5 pg/ml) and normal level of vitamin 25 (OH) D in the blood; no thyroid disorders were detected; according to the acid-base status, there are no metabolic disorders Table 1.
Urinary syndrome is represented by low molecular weight proteinuria (β2-microglobulin - 890 mcg/s); phosphorus excretion is normal (Trm 1.87, EFP 4%), urate excretion is reduced to 0.58 (N 0.8-1.6), and there is no hypercalciuria and glucosuria. According to the radiography of the hands and shins, signs of moderate osteoporosis were revealed. By ultrasound of the kidneys, the volume of the single right kidney is 50%, a cyst (30x40 mm) was found in the middle third along the posterior surface. Considering congenital kidney abnormality (agenesis of the left kidney, ultrasound signs of solitary cyst of the right kidney), moderate osteoporosis, unstable hypercalcemia without hypercalciuria, absence of polyuria and polydipsia, low molecular weight proteinuria, a disease with damage to the renal tubular system, manifested by selective dysfunction of the renal tubules and transient hypercalcemia of unclear etiology (primary, iatrogenic?), is assumed. In order to exclude hereditary tubulopathy, the child's blood is directed to molecular genetic research (full-exome sequencing).
At 1 year 8 months after varicella-zoster infection, the child had "meat slops" color urine. In the urine, erythrocytes (Er) up to 15 in hpf and proteinuria - 1 g/l were detected. The girl was admitted to the nephrology department of the Institute again. Edematous syndrome (edema of the eyelids, pasty anterior abdominal wall, increased abdominal volume), oliguria (1.5 ml/kg/24h), proteinuria of a mixed nature (β2-microglobulin – 1800 mcg/day, urine protein - 6 g/l; daily protein loss - 1.34 g/24h), microerythrocyturia (19-145 bp), hypoproteinemia and hypoalbuminemia (total protein - 43 g/l and albumin – 18 g/l) were noted on examination. We also diagnosed an increase of blood creatinine 86 mmol/ l; with a decrease in eGFR - 41.8 ml/min (CKD 3B st), acceleration of ESR 31 mm/h; according to the acid–base status- sub compensated metabolic acidosis (BE -3.4; pH 7.40) Table 1. Signs of hypercoagulation (D-dimer - 2167 ng/ml) were revealed, positive IgG to CMV and EB virus were detected. By the kidneys ultrasound, the volume of the right kidney is more than 97% with diffuse depletion of blood flow.
Considering the debut of NS, steroid therapy with prednisolone (PS) at a dose of 60 mg/m2, albumin replacement therapy, diuretics, anticoagulants, antiviral therapy (vanciclovir) was started. On the 5th day of taking PS and infusion therapy with albumin and diuretics (furosemide, veroshpiron), edematous syndrome was resolved, but signs of acute renal damage were increasing: urea – 12.6 mmol/l, creatinine 113 mmol/l; eGFR 31.8 ml/min /1.73 m2) Table 1. After 6 weeks of PS-therapy (60 mg / m2), due to the lack of effect from steroid therapy, we diagnosed steroid-resistant nephrotic syndrome (SRNS). Mycophenolate mofetil (MMF) therapy was initiated at a dose of 900 mg / m2 and methylprednisolone pulse therapy at a dose of 30 mg/ kg / 24h (No. 10) 2 times a week with continued use of PS in an alternating mode. During treatment, we observed positive dynamics (total protein – 50 g /l and albumin – 27 g / l, creatinine decrease – 110 mmol / l; eGFR 33.1 ml/min / 1.73 m2) Table 1. After 7 months, MMF was canceled due to frequent acute infectious diseases. Nephroprotective and antiviral therapy was prescribed. At this time, we obtained the results of a molecular genetic study. Full-exome sequencing revealed a previously undescribed missense variant in the GREB1L gene in the heterozygous form p.Val347Leu Table 2 in proband.
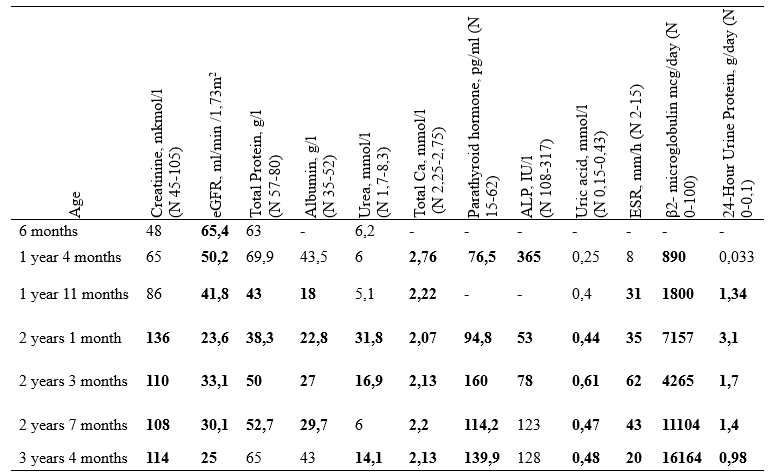
Table 1 The results of laboratory studies in the dynamics of observation (2020-2022) of the patient G.Z
|
Gene |
Associated disease (OMIM) |
DNA alteration (HG38) (protein alteration) |
Zygosity (type of inheritance) |
Frequency (gnomAD v3.1.1) |
|
GREB1L |
Renal hypodysplasia/aplasia 3 (617805) |
18;g21440358G>C ENST00000424526.7: C.1039G>C ENSP00000412060.1: p.Val347Leu |
Heterozygote (Dominant) |
0 |
Table 2 Molecular genetic study (whole exome sequencing) of patient G.Z
According to the results of sequencing using the Sanger (trio) method, this variant was also detected in the proband's father (signs of microlithiasis by ultrasound, while creatinine and eGFR were normal). When reviewing the genetic study in search of pathogenic variants of genes responsible for the development of SRNS, we found in proband an additional heterozygous variant in the EP300 gene associated with autosomal dominant Rubinstein-Tabey syndrome, characterized by kidney abnormality, specific phenotype and podocytopathy. This genetic variant was also detected in proband's mother using Sanger sequencing (right-sided nephroptosis by kidney ultrasound). However, there is no data on the association of EP300 and SRNS.
In the absence of causative genetic variants in the genes responsible for the development of SRNS, a full-genome sequencing was additionally performed, according to the results of which, in addition to the previously identified variant in the GREB1L gene, a previously undescribed variant was found in the UMOD gene in the splicing region (c.1332-16C>G) Table 3, associated with the development of autosomal dominant tubular kidney disease, which is characterized by low molecular weight proteinuria, microerythrocyturia, glomerular proteinuria, hyperuricemia and decreased renal function observed in proband. Validation of the variant using Sanger sequencing (trio) is in progress. Currently, the patient retains proteinuria of a mixed nature (β2-microglobulinuria - 16161 mcg/day, daily proteinuria 0.98 g/24h) without biochemical signs of nephrotic syndrome, decreased renal function to CKD 4 stage (creatinine 168 mmol/l; eGFR Bedside - 21 ml/min / 1.73 m2; cystatin C - 3.67 mg / l; eGFR for cystatin C – 16 ml / min / 1.73 m2), intermittent hyperuricemia and hypocalcemia, there is no hypertension while taking enalapril. Thus, in this clinical case, we present the development of SRNS due to CAKUT, which led to a rapid progression of the disease and a kidney function decrease to CKD 4 stage.
|
Gene |
Associated disease (OMIM) |
DNA alteration (HG38) (protein alteration) |
Zygosity (type of inheritance) |
Frequency (gnomAD v3.1.1) |
|
UMOD |
Tubulointerstitial kidney disease, autosomal dominant (162000) |
16:g.20341352G>C ENST00000396138.9: c.1332-16C>G |
Heterozygote (Dominant) |
0 |
Table 3 Molecular genetic study (whole genome sequencing) of patient G.Z
CAKUT is one of the severe congenital developmental defects in children, which includes a wide range of anomalies of varying severity resulting from genetic and environmental changes, as well as molecular signals disorders during the development of the urinary tract Table 4.1–3 Prenatally, CAKUT is detected in 20-30% of cases among all fetal abnormalities, its prevalence in the world is estimated as 4-60:10,000 births.4,5 CAKUT increases the mortality rate and morbidity rate with the development of chronic renal failure (CRF) in 40-50% of cases.3,5 Most CAKUT are asymptomatic, which prolongs the diagnosis of the defect.5 There are syndromic and non-syndromic, familial and sporadic forms of CAKUT, in infancy CAKUT is often accompanied by lesions of other organs and systems.4,5 According to the literature, about 75 genes associated with the development of isolated or syndromic forms of CAKUT have been recorded Figure 1.1
|
Kidney |
Urinary Tract |
|
Renal agenesis |
Bladder exstrophy |
|
Renal tissue hypoplasia |
Ectopia of the mouth of the ureters |
|
Renal tissue aplasia |
Ureterocele |
|
Renal tissue dysplasia |
Doubling of the ureters |
|
Cystic Kidney |
Megaureter |
|
Anomalies of the kidneys interposition |
Uretero-prepelvic stenosis |
|
Kidney dystopia |
Stenosis of the pelvic-ureteral segment |
|
- |
Duplex collecting system |
|
- |
Valves of the posterior urethra |
|
- |
Vesicoureteral reflux |
Table 4 CAKUT structure1
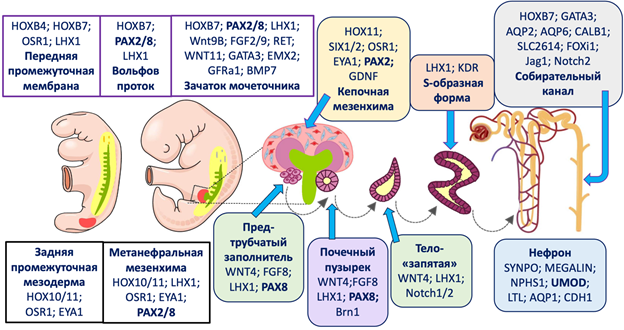
Figure 1 Major candidate genes involved in CAKUT development.6
Jordan P et al.,6 during screening a large panel of genes in 100 fetuses (98 families) affected by severe renal defects, revealed monogenic variants in 22% of cases, in 9 patients (out of 78 families) with bilateral renal agenesis GREB1L was detected.7 In the presented clinical case, pathogenic variants in the GREB1L and UMOD genes were found in a patient with CAKUT. Renal hypodysplasia/aplasia-3 (RHDA3) is an autosomal dominant disease, which is one of the most severe manifestations of CAKUT, mainly caused by pathogenic variants of the GREB1L gene (OMIM:617805) localized on chromosome 18q11, Figure 2.8

Figure 2 Three-dimensional predictive structure of the GREB1L gene.9
At the same time, the proportion of RHDA3 in the phenotypic spectrum is about 0.5% of detected cases of CAKUT.9 RHDA3 is characterized by unilateral or bilateral renal agenesis, and in 32% the disease is accompanied by other CAKUT (congenital hydronephrosis, aplasia of the ureters and bladder, vesicoureteral reflux), rarely – by malformations of the inner ear and deafness, ovarian and uterine agenesis.8,10,11 It is known that the GREB1L gene is a retinoic acid coactivator (RAR) located in chromatin complex near genes encoding α- and γ-RAR receptors.1 It i's considered to be that the signaling role of RAR is the main factor in the development of pronephros, the germination of the ureteral germ in metanephros and the early development of the genitals.1,12 According to the results of a foreign study, during RNA sequencing as a result of GREB1L knockdown in vitro, a sharp decrease in the activity of key PAX2 and PTH1R molecules involved in kidney development was detected, which confirms the important role of the GREB1L gene in the development of metanephros Figure 1.8
However, the mechanism of regulation of renal function by the GREB1L gene and variants of its interactions with key regulators remain unknown.11 Studies in mice have proved that CRISPR/Cas9 mutagenesis involving the GREB1L gene can cause the development of a phenotype of kidneys hypodysplasia/agenesis in conjunction with serious malformations in the form of craniofacial abnormalities, growth retardation, CAKUT, hearing aid development disorders.8,13 It is known that women carrying variants in the GREB1L gene had stillborn children or had a medical abortion because of severe fetus malformations detection.8,13 It has been confirmed that pathogenic variants in the GREB1L gene with reading frame shift, with changing in the splicing sites or with the most common missense variant, can lead to the development of RHDA3, however, these variants are not the only cause of the development of RHDA3.8,14
In the Chinese study, a 3-year-old boy, based on the results of full-exome sequencing, was identified a new missense variant in the GREB1L gene (c.4507C>T,p.R1503W), also found in the mother and grandmother proband, while the grandmother RHDA3 was accompanied by the development of chronic kidney disease (CKD), the mother without signs of urinary system organs damage. The identified missense variant was evaluated as highly conservative, as a result it may be a genetic cause of RHDA3 development in this family.8 It is believed that the missense variant in the GREB1L gene is associated with the intrafamily expressiveness of the gene.14 In families with RHDA3 from Denmark and Iowa, detected heterozygous variants in the GREB1L gene are characterized by incomplete penetrance, the case of a girl with RHDA3 with a heterozygous variant in the GREB1L gene identified de novo is also described.3,14–18
Autosomal dominant tubulointerstitial kidney disease type 1 (ADTKD) is a rare genetically determined disease, mainly caused by pathogenic variants in the UMOD gene (chromosomal locus 16p2, encodes uromodulin protein), which lead to the development of familial juvenile hyperuricemic nephropathy type 1 (OMIM:162000), medullary cystic kidney disease type 2 (OMIM:603860) and glomerular cystic kidney disease (OMIM:609886).12 The listed conditions have been combined into the term ADTKD-UMOD since 2015 Figure 3. ADTKD-UMOD is more often detected among Chinese patients than European population, and among all patients with CRF occurs in 0.9% of cases.12 It is assumed that pathogenic variants inherited by autosomal dominant type in the UMOD gene disrupt the maturation and intraepithelial uromodulin transport, resulting in reduced protein excretion into the lumen of the tubule.12
At an early stage, ADTKD-UMOD is manifested by hypouricosuric hyperuricemia (with fractional uric acid excretion decrease <5%), however, in 20% of patients, persistent hyperuricemia and severe arterial hypertension (AH) are not observed. In the presence of the ADTKD-UMOD, the concentration of uromodulin in the urine decreases, renal function decreasing progresses, joint syndrome of the type of gout with thumb and ankle lesions joins in adolescence, tubulointerstitial lesions are detected with nephrobiopsy.12,19 Urinary syndrome is presented in the form of an "empty" urinary sediment (single Er., daily proteinuria <500 mg), as well as nocturia and enuresis.12,19 Cases of gout have been described in patients with pathogenic variants in the UMOD gene, while among patients with ADTKD-UMOD with impaired concentration function, gout is more common and begins much earlier.20 A reduction in plasma volume and a higher reabsorption activity of the proximal tubules may explain the phenotype of hyperuricemia in ADTKD-UMOD.20 Considering the previously described effect of the GREB1L gene on the action of PAX2, it is possible that the development of tubular disorders in the patient is associated not only with a pathogenic variant in the UMOD gene, but also with a mutation in the GREB1L gene.8
According to research by Westland R et al.,21 in 21% of patients with unilateral renal aplasia (URA), microalbuminuria is detected, and in 10% - renal function decrease (eGFR <60 ml/min /1.73 m2).21 According to the authors, the presence of URA is a potential risk of developing CKD, and the risk of developing renal failure in children with a single functioning kidney increases in case of association with CAKUT.21 SRNS ranks second after CAKUT among the causes of CKD progressing to the terminal stage of CRF, while in 30% of cases in children it is caused by the presence of genetic disorders.22,23 It is known that the NPHS1, PLCE1, NPHS2 and SMARCAL genes are often involved in the development of SRNS, and the UMOD, GREB1L and EP300 genes are not included in the groups of candidate genes or genes causing SRNS phenocopy.22,24 It is proved that that pathogenic variants of the PAX2 gene, which can be influenced by RAR signaling molecules, are the cause of the development of NS secondary to focal segmental glomerulosclerosis (FSGS) in the adult population.26 PAX2 is a transcription factor that plays a central role in the early embryonic development of the kidneys and ensures the correct connection between the ureteral rudiment and the surrounding metanephral mesenchyma, which epithelizes with the formation of podocytes. It is proved that the nephron progenitor cells, deprived of PAX2, cannot differentiate into nephron cells, which eventually leads to a violation of the function of the glomeruli Figure 4.25–28 The literature describes a case of SRNS with a histological picture of FSGS, in which a pathogenic variant in the PAX2 gene was detected de novo.26 In the Vivante A et al.,26 cohort study (2019) according to the results of full-exome sequencing of 215 patients with familial SRNS, were identified pathogenic variants in the PAX2 gene (5.2%), which allowed expanding the phenotypic spectrum of heterozygous forms of the PAX2 gene, including autosomal dominant FSGS.26 In all patients of the study, the CAKUT phenotype and the presence of pathogenic variants associated with SRNS were excluded.26 Considering complex interactions of genes in the embryonic development of the kidneys, it can be assumed that the development of SRNS during an infectious disease in our patient with RHDA3 and ADTKD may probably be due to the influence of the GREB1L gene on the action of the PAX2 gene, which has not been previously reported Figure 5
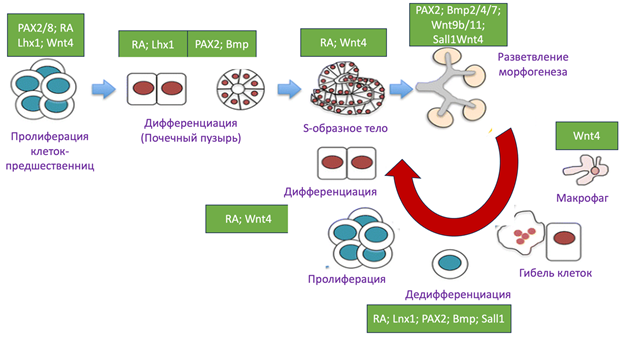
Figure 4 Interaction between PAX2 and retinoic acid (RAR) in embryonic kidney development.28
The presented clinical case with severe CAKUT in the form of agenesis of the left kidney is characterized by polymorphism of the clinical picture (solitary cyst in the single right kidney, β2-microglobulinuria, unstable hyperuricemia) and variability of variants of the UMOD and GREB1L genes not associated with the development of SRNS. The progressive decrease in renal function with the development of CKD at 4 stage is probably because of the development of SRNS against the background of ADTKD and RHDA3. At the moment, the girl has unstable minor hyperuricemia, however, considering the age and progressive CKD, it should be remembered about the risk of developing gout in future. Constant monitoring of laboratory parameters of uric acid can allow us to suspect the onset of this disease in time and start pathogenetic therapy in a timely manner. Special attention is drawn to the development of the SRNS, which required revision of the genetic studies results. However, mutations in the genes associated with the development of SRNS, including the PAX2 gene, were not detected in the patient, which most likely indicates the importance of a viral infection (varicella-zoster) in the development of SRNS in the child with CAKUT.
Thus, CAKUT is an urgent problem in the modern clinical practice of nephrologists, pediatricians, urologists and geneticists, as it is the leading cause of terminal CRF in children. Early diagnosis and proper treatment tactics are of great importance, because of rate of CKD progression effective decreasing.
None.
The authors declares that there is no conflict of interest.

©2024 Zaikova, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.