eISSN: 2378-3176


Case Report Volume 12 Issue 2
1Urologist, Universidad de Antioquia, Colombia
2Urologist, Universidad Militar Nueva Granada, Colombia
3Urology department, Hospital Manuel Uribe Ángel, Colombia
4M.D., Universidad CES, Colombia
Correspondence: Camilo Girado-Villegas, Urology department, Hospital Manuel Uribe Ángel, Colombia, Tel 5581792
Received: July 08, 2024 | Published: August 16, 2024
Citation: Aristizabal HD, Aristizabal AF, Girado-Villegas C, et al. Bladder fungoma (fungal bezoar) by two Candida species in Medellín, Colombia: a case report and review of the literature. Urol Nephrol Open Access J. 2024;12(2):41-43. DOI: 10.15406/unoaj.2024.12.00354
The presence of fungal infections in the urinary bladder is rare; there are no extensive reviews on this subject in current literature, even less with the presence of two different types of fungi in the same culture. We present a case of an 82-years-old male patient with a history of benign prostatic hyperplasia (BPH) and type 2 diabetes mellitus (DM2) who underwent a simple suprapubic prostatectomy. Shortly thereafter, he was readmitted to the emergency room with symptoms of fever and urinary distress, eventually diagnosed with a fungal infection caused by Candida tropicalis and Candida glabrata in the urinary bladder, secondary to prostatic hyperplasia. He was admitted for assessment and multidisciplinary management. Guided treatment with caspofungin 50mg every 12 hours for 14 days resulted in clinical improvement. Proper diagnostic approaches are crucial for effective management of bladder fungomas, ensuring optimal patient outcomes.
Keywords: urinary bladder, infections, urogenital surgical procedures, candida glabrata, candida tropicalis
Although fungal infections in the urinary tract are increasing, the presence of fungal bezoar is extremely rare, approximately 20 cases have been reported medical literature1 since the first one reported in 1961 by Chisholm & Hutch,2 none of then involving more than 1 fungal organism. We report a case of a patient with a bladder infection by Candida tropicalis + Candida glabrata after an open prostatectomy for treatment of BPH, accompanied by a review of the literature.
An 82-years-old male patient with history of BPH and on-insulin-requiring DM2 who was under pharmacological management with tamsulosin due to the presence of long-standing lower urinary tract symptoms (LUTS), with a prostate volume of 120cc by ultrasound (US), prostate-specific antigen (PSA) of 4.3 ng/dl, and transurethral cystoscopy showing a healthy anterior urethra and no urethral stricture, but poor patient tolerance. Due to poor improvement with medical management, he underwent an open suprapubic prostatectomy, showing a clinical adenomatous prostate of approximately 100 grams and abundant cerebriform intravesical tissue, confirmed pathologically as nodular glandular hyperplasia with vesical fungal ball formation (Figure 1 & 2). Postoperatively, he was readmitted due to progressive deterioration of his functional class, hyporexia, asthenia, pain at surgical site, fluctuation of consciousness and chills. Laboratory tests revealed C-reactive protein (CRP) 19,8 mg/dl, white cell count 15.040 with 70,1% being polymorphonuclear neutrophils (PMN), urinalysis with pyuria, hematuria and yeast in average amount. A contrast abdominal CT scan was performed (Figures 3–5) reporting bilateral pyelonephritis without abscess, prevesical fluid and emphysema, and periprostatic emphysema, making diagnosis of a deep surgical site infection (SSI) plus an urinary tract infection (UTI). Empirical antibiotic plus antifungal management was started with piperacillin/tazobactam 4,5gr every 8 hours + vancomycin 1g every 12 hours + fluconazole intravenous (IV). A urine culture reported the presence of Candida glabrata + Candida tropicalis confirming the diagnosis, antibiotics were suspended and guided treatment was started with Caspofungin 50mg IV every 12 hours for 14 days, resulting in significant clinical improvement.
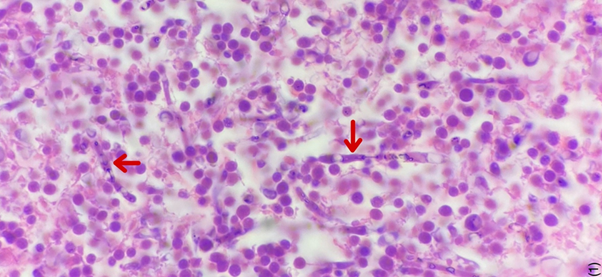
Figure 1 Pathology of transurethral bladder resection with hematoxylin eosin staining.
Red arrow: multiple hyphae

Figure 2 Pathology of transurethral bladder resection with methenamine silver staining.
Red arrow: multiple hyphae. Blue arrow: yeasts
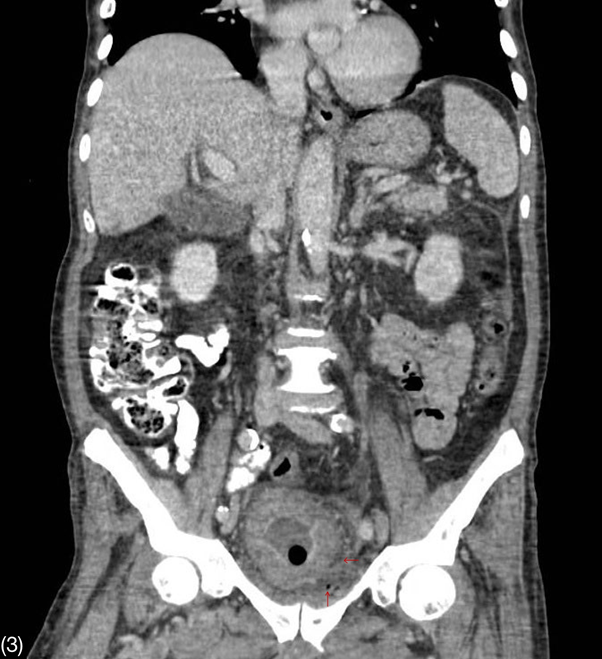
Figure 3 Contrast-enhanced CT scan of the abdomen in coronal view.
Thickening of bladder walls and emphysema in the prevesical space.
Fungal infections in the urinary tract are rare, accounting for less than 1% of cases in patients without predisposing factors but up to 5-10% in hospitalized and catheterized patients.3 Bladder fungomas are even rarer; the first case report dates back to 1961 when Chisholm and Hutch published a series of cases with two patients presenting Candida albicans balls in the bladder.1 Since then, just over 20 case reports have been reported in the literature, most of them caused by Candida albicans in 50-70% of the cases. Other organisms described are other Candida species, Aspergillus, Penicillium, and Mucorales.2
The main risk factor is the coexistence of diabetes mellitus, not only because the patients are immunosuppressed, but also because of the presence of glycosuria which forms an ideal growth medium. Other risk factors are the presence of permanent urinary catheters, bedridden patients and recent antibiotic management.1,4
Fungal infection can reach the urinary tract by two paths: bloodstream (antegrade infection) or ascending through the urinary tract from a focus of Candida colonization in or near the urethra (retrograde infection), with the latter being more widely accepted.3
The Candida species have different virulence factors that allows them to infect different tissues; among them, the best know are adherence, dimorphism, galvanotropism and thigmotropism, phenotypic change, hydrolytic enzymes, biofilm formation, and evasion of immune response.3 Initially, they poorly adhere to the mucosa of the urinary tract, but under certain conditions such as urinary tract obstruction, concomitant bacteriuria, and immunosuppression, invasion of the bladder walls, urethra, ureter and kidney can occur.3,5 However there is relatively limited information on how these virulence factors are regulated and then orchestrated to produce the many clinical forms of Candida UTI.6,7
When fungal organisms are discovered in the urine, the first question to ask is whether we are dealing with a urinary tract infection, colonization, or contamination of the urine sample, so empirical management is not recommended, and a second urine sample should be taken to confirm the fungi.3,8
Symptoms are indistinguishable from those of bacterial cystitis or pyelonephritis. Oliguria, strangury, and pneumaturia suggest a more unusual problem.3 The presence of air in the bladder lumen is typically described due to the different reactions that occur in the metabolism of fungi, which ends in the production of CO2, which can aid to the diagnosis of fungal infection, in addition to the production of lactic and butyric acid, which causes acidification of the urine.9 Ultrasonography is the preferred initial study in patients admitted in the intensive care unit (ICU) or in those with altered renal function. Computerized tomography (CT) urogram is a better exam in suspected cases of pyelonephritis and peripheral abscesses, as it allows for better visualization of perinephric fluid, gas in renal tissue, and presence of fungal bezoars causing obstrution of the urinary tract.10
Fluconazole is the drug of choice for cystitis and pyelonephritis in most Candida species (except for resistant species such as Candida glabrata, Candida Krusei, and other described in the literature) because it is water-soluble and eliminated mainly through urine as an active drug. For cystitis, the dose is 200-400 mg orally every day for two weeks. An alternative is the use of flucytosine at a dose of 25mg/kg orally every 6 hours for 2-4 weeks (renal adjustment is required), generally used 7-10 days to reduce fungal resistance which, can quickly develop if used as monotherapy for extended period.7,10
Several experimental studies have demonstrated the elimination of Candida in cases of pyelonephritis with the use of echinocandins.7 These have been primarily studied for systemic candidiasis and have shown to be effective in Candida infections. The IV regimens used are caspofungin with a loading dose of 70 mg followed by 50 mg per day, anidulafungin with a loading dose of 200 mg followed by 100 mg per day, and micafungin 100 mg per day.11 In most patients with fungal bezoars in the urinary tract, systemic treatment with amphotericin B (with or without flucytosine of fluconazole) is used7 at a dose of 0.5-0.7 mg/kg IV as a single dose or until symptoms resolve and urine cultures do no longer show Candida species.11
According to the medical literature, fungal infection in the urinary tract is a very rare cause of presentation in the etiological spectrum of the disease. In this case, in addition to the microbiological findings, there was an intraoperative finding of an atypical lesion within the bladder that makes the clinical diagnosis indisputable. Finally, there is corroboration of pathological anatomy of the surgical specimen with the presence of fungi in the bladder.
Fungal infections in the urinary tract, particularly bladder fungomas, present significant challenges in diagnosis and management. This case emphasizes the need for comprehensive diagnostic strategies, multidisciplinary management, and timely intervention to improve patient outcomes, given the association with prolonged hospitalization and concurrent bacterial infections.
None.
Study concept and design: Hernan D. Aristizabal, Andrés F. Aristizabal.
Data acquisition: Hernan D. Aristizabal, Camilo Girado-Villegas.
Data analysis: Camilo Girado-Villegas, Daniel Aristizabal.
Drafting of manuscript: Hernan D. Aristizabal, Andrés F. Aristizabal, Camilo Girado-Villegas, Daniel Aristizabal.
Critical revision of the manuscript: Hernan D. Aristizabal.
The authors declare no conflict of interest.

©2024 Aristizabal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.