eISSN: 2378-3176


Case Report Volume 8 Issue 1
1Diagnostic Center Lucilo Ávila Júnior, Recife, PE, Brazil
2Bacchi Pathology Consultancy, Botucatu, SP, Brazil
3Pathology, AC Camargo Cancer Center, Brazil
Correspondence: , Tel + 55 (81) 996978135
Received: January 31, 2020 | Published: February 14, 2020
Citation: Machado CC, Gurgel FV, Alves HTDC, et al. Angiomyofibroblastoma of ischiorectal fossa: a case report. Urol Nephrol Open Access J. 2020;8(1):21-24 . DOI: 10.15406/unoaj.2020.08.00268
Introduction: The differential diagnosis of female pelvic tumors is broad and most frequently arises from the reproductive organs. This paper reports an uncommon benign pelvic tumor of mesenquimal origin.
Case report: A 71-year-old woman with cellulitis at the right gluteal region underwent transvaginal pelvic ultrasound, which showed a large solid and cystic pelvic tumor. Diagnostic investigation through magnetic resonance imaging played a fundamental role in determining the origin of the lesion in the right ischiorectal fossa. Histopathological and immunohistochemical studies of the specimen defined a benign genital stromal tumor: angiomyofibroblastoma.
Conclusion: Defining the origin of pelvic lesions at imaging exams and, mainly, histopathological analysis is decisive to make the correct diagnosis. Although vulva and vagina are the most common sites of angiomyofibroblastoma, this neoplasm can rarely occur in the pelvic and extrapelvic tissues.
Keywords: pelvic tumors, pelvis neoplasms, pelvic cancer
There are a variety of lesions in the differential diagnosis of female pelvic tumors and they mostly arise from the reproductive organs. However, some other organs and tissues can also produce pelvic masses as gastrointestinal and urinary tumors, lesions arising from adjacent soft tissues, peritoneum, retroperitoneum or metastatic dissemination. The patient’s clinical history, the exact site of origin, and imaging characteristics may help to narrow the diagnosis. This paper reports a case of an extensive pelvic solid and cystic angiomyofibroblastoma with extrapelvic origin in the right ischiorectal fossa.
A 71-year-old woman developed clinically gluteal cellulitis. During the diagnostic investigation by transvaginal pelvic ultrasonography, a multiloculated pelvic solid and cystic lesion was detected, with septations and scarce blood flow to color Doppler (Figure 1). This exam couldn’t define the original site of this lesion. Pelvic magnetic resonance imaging (MRI) revealed a large pelvic solid and cystic formation with well-defined limits and an important cranial and anterior dislocation of the uterus and bladder (Figure 2). Retraction of the right ischiorectal fossa fat through the lesion and towards the pelvic cavity was detected (Figure 3) and represented a decisive information in the diagnostic investigation. Patient underwent surgical resection with complete excision of the tumor and evolved well in the postoperative (Figure 4). The histopathological examination revealed a neoplasm characterized by a densely collagenized stroma with alternating zones of cellularity, consisting of small spindled or ovoid cells with moderate amounts of eosinophilic cytoplasm and nuclei with fine chromatin and inconspicuous nucleoli, clustered around thin-walled capillaries (Figure 5). The immunohistochemical study revealed diffuse expression of desmin as well as estrogen and progesterone receptors, corroborating the diagnosis of angiomyofibroblastoma. There is no sign of tumor recurrence in periodic imaging exam less than one year after surgery.

Figure 1 Transvaginal pelvic ultrasound. Solid and cystic expansive formation (A). Scarce blood flow to color Doppler (B).
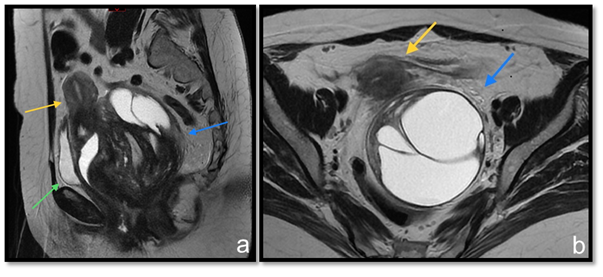
Figure 2 T2 weighted MRI sequences at sagittal (A) and axial (B) planes. Pelvic expansive formation (blue arrow) promotes uterus (yellow arrow) and bladder (green arrow) displacement from their usual topography.
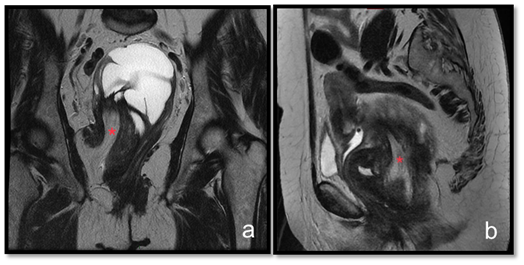
Figure 3 T2 weighted MRI sequences at coronal (A) and sagittal (B) planes. Fat from the right ischiorectal region insinuates along the lesion to the pelvic region (red asteristic).
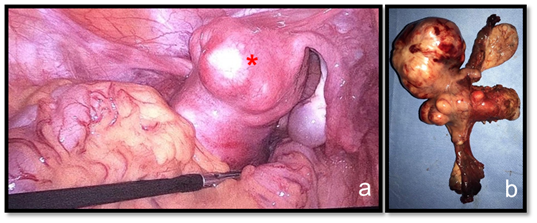
Figure 4 Videolaparoscopic view of the tumor indicated by a red asterisk (A). Surgical specimen (B).
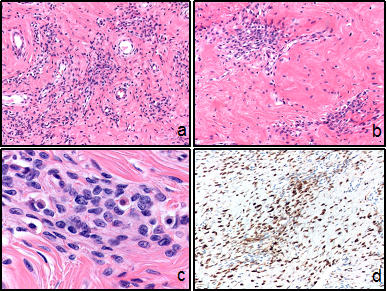
Figure 5 Microscopic features.
Low-power appearance of angiomyofibroblastoma with alternating zones of cellularity in which the stromal cells are clustered around small vessels in 100x amplification (A;B).
Tumor cells, observed in 400x amplification, are predominantly spindled, although in some areas more epithelioid or ovoid-shaped (C).
Diffuse expression of desmin (D).
First described in 1992, angiomyofibroblastoma is an unusual benign tumor of mesenchymal origin that may or not be clinically accompanied by local pain.1–4 Its real incidence has not been known.5 Affecting almost exclusively women at menacme and early menopause periods, justified by estrogen and progestin receptors in tumor cells, angiomyofibroblastoma is most frequently found at the external female genitalia (vulva, vagina, pelvis and perineum).6 There are reports of cases at fallopian tubes and urethra either.7,6 The term "angiomyofibroblastoma-like tumor of the male genital tract” is a misnomer since it refers to a similar, but not identical tumor (cellular angiofibroma), which can occur in both sexes.8 Angiomyofibroblastoma is generally a slow-growing, typically small (<5 cm), well circumscribed lesion and may be mistaken for a cyst on clinical examination.9 Radiologically, they appear as a single soft-tissue lesion with well-circumscribed edges and mixed echogenicity.10 Macroscopically, the tumor is usually tan to pink soft tissue mass that has a soft or rubbery consistency without necrosis or hemorrhage.11,12 The neoplasm shows, histopathologically, numerous delicate thin-walled capillary-sized vessels surrounded by plump, round to spindle-shaped cells. These stromal cells are set within a variably edematous to the collagenous matrix with alternating zones of cellularity.13 The major characteristic of this myofibroblastic tumor is prominent vascularization with perivascular fibrinoid hyalinization.6 Interestingly, in postmenopausal patients, as in the present case, angiomyofibroblastoma shows a drop in cellularity and increased stromal collagen as well as a tendency for the tumor cells to be more spindled and less epithelioid.14
Immunohistochemically, the stromal cells are typically strong and diffusely positive for vimentin and desmin, estrogen and progesterone receptors. The cells shows variable reactivity for smooth muscle actin and CD34, although they are usually negative for those markers.8 Deep (aggressive) angiomyxoma represents the main differential diagnosis of angiomyofibroblastoma due to its equal preference for the female pelvic and perineal tissues, although, should be distinguished by its recurrent potential.8 In contrast to angiomyofibroblastoma, deep angiomyxoma is uniformly paucicellular. Both tumors have a similar immunophenotype, therefore distinction is based solely on the morphologic differences and clinical and radiological features.14,15 The recommended treatment of angiomyofibroblastoma is simple local surgical excision as recurrences are very rare. However, when there is doubt about the diagnosis, especially because of its similarity with deep angiomyxoma, resection with wide margins might be indicated with both short and long-term postoperative follow up.16
Most cystic tumors of the female pelvis originate from reproductive organs, especially from the ovaries. However, in imaging, it is important to consider the other lesions that can mimic ovary tumors as they affect the patient's treatment. Defining the origin of the lesion on imaging exams is decisive to orientate the differential diagnosis and to aid the pathologists for the correct diagnosis. Due to its rarity in non-vulvar and vaginal tissues, angiomyofibroblastoma can become a diagnostic challenge when occurring in pelvic and extra pelvic tissues. In these cases, clinical, radiological, surgical and pathological correlation is very important for the final diagnosis and treatment definition.
None.
The author declares there is no conflict of interest.
None.

©2020 Machado, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.