eISSN: 2378-3176


Research Article Volume 2 Issue 3
1Department of Nephrology, Urology and Nephrology Center, Egypt
2Department of Urology, Urology and Nephrology Center, Egypt
Correspondence: Ahmed I Akl, Urology and Nephrology center, Mansoura, Egypt, Tel 20502262222, Fax 2050223717
Received: January 03, 2015 | Published: April 9, 2015
Citation: Akl A, Neamatalla AH, Nagib AM, et al. Comparative analysis of long term survival of pediatric and adult living donor renal transplantation: single center 10years experience. Urol Nephrol Open Access J. 2015;2(3):85-90. DOI: 10.15406/unoaj.2015.02.00040
Our objective was to highlight the results of comparative analysis of pediatric and adults living donor renal transplantation in a single center experience extended for more than 30years. The study comprised of 1902 adults and 338 children aging 18years or younger. Male sex was dominant among recipients of both groups in contrary to female sex that constituted for 75.9% for adults and 63.6% for pediatrics. No statistical difference was encountered for patient survival at 5 and 10years for both groups. A significant difference was observed between pediatrics and adults 10years graft survival. Moreover comparable patients are living enjoying good graft function for both groups at last follow up. The significant outcome predictors for graft survival for pediatrics were primary immunosuppression, acute rejection and post transplant hypertension while the corresponding factors for adults included donor age >40years, primary immunosuppression, acute rejection, and post transplant hypertension. Multivariate analysis revealed that acute rejection sustained its impact for pediatrics while donor age >40years, primary immunosuppression, acute rejection and post transplant hypertension still had a significant effect on outcome for the adults.
Keywords: living donor transplantation, pediatrics transplantation, adult transplantation, long term graft survival
ATN, acute tubular necrosis; Aza, azathioprine; CsA, cyclosporine a; MMF, mycophenolate mofeti
Renal transplantation is the treatment option of choice for children suffering from end stage renal diseases.1 Children have a unique situation that differs from the adults. Compliance on dialysis, school attendance, growth and puberty beside surgical, immunologic and psychological aspects are contributing factors for that difference between children and adults.2
Numerous reports all over the world highlighted aspects and results of adult transplantation. However pediatric transplantation outcome was published at a lesser extent. Scare comparative studies between the two population groups are reviewed in the literature. Herein, we highlighted the results of comparative analysis of pediatric and adult living donor kidney transplantation in a single center experience extended from more than 30years.
Between March 1976 and June 2011, 2240 consecutive living donor renal transplantation were carried out at Mansoura urology and nephrology center, Egypt, 1902 were above 18years (adult group 84.9%) while 338 were, aged 18years or below (pediatric recipients, 15.1%). Demographic characteristics, primary immunosuppression plan, original kidney diseases, causes of death either with functioning graft or with failed one, rejection episodes, complications beside condition and clinical grading at last follow up.
For recipients, our exclusion criteria for transplantation included sensitization with a Positive lymphocytotoxic cross match, recent malignancy, addiction, psychiatric disorders, type I diabetes mellitus, active infection and significant extra-renal organ disease (pulmonary, hepatic and cardiac). Contraindications to donation included: age above 60years or below 21years, active infections, diabetes, any minimal renal functional impairment, proteinuria or hematuria. Hypertension and serology test results positive for HIV, HBV or HCV.
The graft function was monitored by periodic estimation of serum creatinine and creatinine clearance. Data were organized to provide analyses of patient and graft survival rates and the predictors for 10-year graft survival. Evaluation of the possible variables that may affect the graft survival was carried out using univariate analysis and multivariate analysis. Studies factors included age, sex, original kidney disease, relationship of donor and recipient, ABO blood group equality, pre-transplant blood transfusion, HLA and DR matching, pre-transplant dialysis, cold ischemia time, number of renal arteries, urinary re-continuity, time to diuresis, time of transplantation, occurrence of acute tubular necrosis (ATN), primary and secondary immunosuppression, total dose of steroids in the first 3months, development of acute rejection and post-transplant hypertension. ATN was defined by the need for dialysis during the first week after transplantation. Hemodialysis was the comments form of dialysis before transplantation (92%).
Most patients that received transplants before 1988 were treated with daily oral administration of 7.5-15mg prednisolone (the mean daily dose at 6months post-transplantation was 0.3mg/kg and was reduced thereafter) and 2.5mg/kg azathioprine (Aza) as combined therapy. From 1988 to 1998 a triple-therapy regimen comprising daily prednisolone between 5mg and 10mg (the mean daily dose at 6months post-transplant was 0.25mg/kg and was reduced thereafter), azathioprine 2mg/kg and cyclosporine A (CsA) was administered. Alternate-day prednisolone was used in 48 patients (22%). Cyclosporine whole-blood trough levels were maintained between 100ng/ml and 150ng/ml. Tacrolimus and mycophenolate mofetil (MMF) have been introduced as a primary therapy since 1998, and sirolimus has been used since 2002, in addition to prednisolone. No induction therapy was used. Acute rejection episodes (requiring confirmation of renal pathology by biopsy prior to anti-rejection treatment) were treated with intravenous bolus doses of methylprednisolone (250-500mg/day) for three to five consecutive days. Steroid-resistant patients were treated with plasmapheresis (15 patients) on alternate days for up to 10days and/ or ATG (six patients) or OKT3 (two patients). Plasmapheresis was performed with Gambro AK 10 and AK 100 machines.
A 1.4 volume pheresis was performed with replacement of plasma by 5% albumin. The duration of pheresis and blood flow rate was determined according to patient height, weight, hematocrit, and tolerance to anticoagulation. TB was diagnosed by one or more of the following methods:
Kaplan–Meier curves and log-rank tests were used to describe and compare the graft survival rates in stratified univariate analyses. Tests of significance were carried out using the chi-square method, with a P value of <0.05 taken to indicate statistical significance. All P values were two-sided. A multivariate analysis of graft survival was performed using Cox proportional hazards regression models to adjust for potentially confounding variables that could influence outcomes. The SPSS statistics package (SPSS V11.0, SPSS Inc., USA) was used for these analyses.3
Our overall experience of living donor renal transplantation constituted 15.1% pediatrics and 84.9% adults. The male sex was dominant among both groups (63.6% vs 75.9%), as regard the donor female sex it was 68.3% in the pediatrics versus 50.2% in adults. The mean age of recipients was 13.7+3.9years and 32.3+ 9.1years for both groups and the corresponding figures for donor age was 37.7+8.2years and 35.6+10.5years respectively (Table 1A) chronic GN and PN represented 19.5%, 11.5% as original kidney disease for pediatrics and 9%, 12.4% for adults. Majority of donors were related (83% vs 17%), with same blood group (80.3% vs 19.6%) and 50% HLA matching was (80.6% vs 74.9%). Hypertensive recipients were 42.3% vs 61.1% while pre-emptive transplantation was carried out in 9.2% in pediatric group and 3.9% of adult group. Concerning immunosuppression, induction therapy was utilized in 52.1% and 50.3% for both groups. The CsA based immunosuppression protocols adapted for pediatrics 59.2% and for 60.7% adults were comparable, similarly the pre transplant blood transfusion (39.1% vs 43.4%) (Table 1B).
Pediatrics No. (%) |
Adults No. (%) |
P- value |
|
Recipient Male sex |
215 (63.6) |
1443 (75.9) |
<0.001 |
Donors female sex |
231 (68.3) |
955 (50.2) |
<0.001 |
|
Age of donors >50
|
67(19.8) 20 (5.9) |
774 (40.7) |
<0.001 |
|
Original kidney disease -ESK |
66 (37.1) 71 (27.7) |
171 (23) |
<0.001 |
|
Consanguinity -Unrelated |
306 (90.5) 32 (9.5) |
1554 (81.7) |
<0.001 |
Same Blood group |
262 (77.5) |
1537 (80.9) |
0.155 |
Pre-Tx dialysis |
307 (90.8) |
1827 (96.1) |
<0.001 |
Pre-Tx HTN |
143(42.3) |
1162 (61.1) |
<0.001 |
Bilharziasis |
29 (8.6) |
502 (26.4) |
<0.001 |
50% HLA Matching |
233 (80.6) |
1291 (74.9) |
0.037 |
Induction therapy |
176 (52.1) |
956 (50.3) |
0.540 |
Primary plan IS -Steroid free |
23 (6.8) 82 (24.3) |
286 (15.2) |
<0.001 |
|
Blood transfusion - yes |
132 (39.1) |
826 (43.4) |
0.097 |
|
Primary Ur. Continuity - U-U |
326 (96.4) 10 (3) |
1877 (98.6) |
0.020 |
Immediate diuresis |
299 (88.5) |
1769 (93) |
0.004 |
Table 1A Demographic characteristics.
|
Pediatrics No. |
Adults No. |
P-value |
Re-Transplantation |
4 (1.2) |
79 (4.2) |
0.022 |
P.O. Mortality (10 years) |
43(12.7) |
323 (17) |
0.105 |
Post transplant hypertension |
171 (50.6) |
1163 (61.1) |
<0.001 |
Post transplant DM |
17 (5) |
413 (21.7) |
<0.001 |
Post transplant malignancy |
7 (2.1) |
96 (5) |
0.016 |
Secondary IS |
147 (43.5) |
884 (46.5) |
0.310 |
Secondary IS |
4 (1.2) |
35 (1.8) |
0.656 |
Urologic complications |
25 (7.4) |
132 (6.9) |
0.417 |
Bacterial infection |
49 (14.5) |
389 (20.5) |
0.006 |
Viral infection |
30 (8.9) |
209 (11) |
0.143 |
11-ATN |
22 (6.5) |
97 (5.1) |
0.287 |
Rejection (yes) |
127 (41.1) |
745 (41.6) |
0.870 |
Rejection frequency (>2) |
108 (32) |
491 (25.8) |
0.024 |
Rejection type |
115 (34) |
663 (34.9) |
0.035 |
Serum creatinine |
1.28+0.77 |
1.40+0.66 |
0.006 |
Table 1B Demographic characteristics.
The post-transplant results outlined in Table 1B revealed comparable mortality at 10years (12.7% vs 17%), post transplant hypertension (50.6% vs 61.1%), secondary immunosuppression (43.5% vs 46.5%), urologic complications (7.4% vs 6.9%), acute cellular rejection (34% vs 34.9%), acute vascular rejection (3% vs 3.7%). While pediatric recipients experienced higher ATN (6.5% vs 5.1%), chronic rejection (25.1% vs 20.1%). On the other hand, adults had increased post transplant DM 21.75% vs 5% in pediatric group, Malignancy (2.1% in pediatrics vs 5% in adults), re-transplantation (1.2% vs 4.2%) immediate diuresis ( 88.5% vs 93%), bacterial infections ( 14.5% vs 20.5% ) and viral infection (8.9% vs 11%). The leading causes of death with functioning grafts in pediatric group are trauma and bleeding, CV and respiratory, while the causes of mortality with failed graft included CV, GIT and liver dysfunction, respiratory. On the other hand the causes of death with functioning grafts in adults are CV, respiratory, GIT, hepatic and malignancy. The prominent causes of death with failed graft in adults CV, GIT, hepatic (Table 2).
With functioning graft |
Pediatrics No. |
Adults No. |
C.V. |
3 (21.4) |
46 (18.3) |
Resp. |
1 (7.1) |
28 (11.1) |
Blood + Trauma |
3 (21.4) |
3 (1.2) |
Malignancy |
2 (14.3) |
25 (9.9) |
GIT + liver |
-- |
31 (8.7) |
Infection |
-- |
27 (10.7) |
Cerebral |
-- |
17 (6.7) |
Unknown |
-- |
1 (0.4) |
With failed graft |
Pediatrics No. |
Adults No. |
C.V. |
10 (31.3) |
40 (24.4) |
Resp. |
2 (6.3) |
22 (13.4) |
GIT + liver |
2 (6.2) |
21 (12.8) |
Infection |
2 (6.3) |
12 (7.3) |
Malignancy |
-- |
9 (5.5) |
Unknown |
16 (50) |
55 (33.5) |
Table 2 Demographic characteristics
At last follow up more or less patients are living enjoying graft function (57.1% vs 53.5%). Serum creatinine was significantly lower (1.28+0.77mg/dl) in pediatric group compared to Adult group (1.40+0.66mg/dl) in the first year but later it become comparable (Table 1B). The actuarial patient survival at 5 and 10years were 91.6+1.74 and 81.63+2.92 for pediatrics and 89.51+0.76, 77.36+1.25 for adults. The corresponding figures for the graft survival were 83.9+2.28 , 58.34+3.53 for pediatrics and 87.24+0.84 , 66.78+1.38 for adults respectively, p<0.001 (Figure 1) (Figure 2).
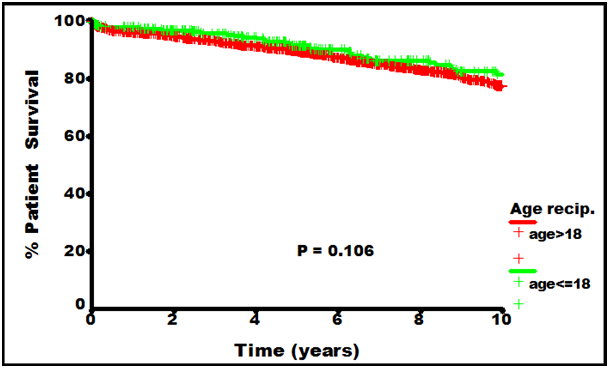
The actuarial patient survival at 5 and 10 years were 91.6+1.74 and 81.63+2.92 for pediatrics and 89.51+0.76 , 77.36+1.25 for adults p=0.106.

The actuarial graft survival were 83.9+2.28 , 58.34+3.53 pediatrics and 87.24+0.84 , 66.78+1.38 for adults respectively, p=0.0002.
Outcome predictors of graft survival for pediatrics were Donor age ≥40years, type of primary immuno suppression, acute rejection and post transplant hypertension by univariate analysis for both groups. While those who act independently in multivariate analysis were only acute rejection for pediatrics. While for adults were Donor age ≥40years, steroid free based primary immunosuppression, acute rejection and post transplant hypertension (Table 3) (Table 4).
|
Pediatric group |
Adults group |
||
|---|---|---|---|---|
10 years survival |
P value |
10 years |
P value |
|
Recipient age |
78.4/71.2 |
0.162 |
----------- |
------- |
Donor age |
77.5 / 66.4 |
0.190 |
83.1/70.2 |
<0.001 |
Recipient sex |
68.7 / 83.5 |
0.352 |
79.7/79.9 |
0.897 |
Donor Male/ |
70.3 |
|
81.2 |
|
Recipient female |
81.3 |
|
84.3 |
|
Donor female/ |
63.2 |
0.254 |
77.9 |
0.400 |
Original kidney disease |
||||
GN |
64.6 |
|
76.7 |
|
Ch. Pyeloneph. |
76.5 |
|
82.3 |
|
Hereditary GN |
70.7 |
|
80.8 |
|
End stage |
73.9 |
0.747 |
79 |
0.096 |
Prior blood transfusion (No/yes) |
73.7/72.4 |
0.436 |
77.3/81.8 |
0.503 |
Pre-emptive Tx |
||||
Yes |
85.3 |
|
70.7 |
|
Dialysis |
73.4 |
0.726 |
80 |
0.447 |
Donor source |
73.2/74 |
0.897 |
80.3/76.7 |
0.509 |
Primary IS |
||||
Aza based |
58.6 |
|
85.5 |
|
Calcineurine based |
73.4 |
|
78.6 |
|
Steroid free |
94.1 |
0.017 |
81.3 |
0.064 |
Time to diuresis |
74/67.1 |
0.320 |
79.8/79.1 |
0.745 |
ATN |
74.7/63 |
0.164 |
79.8/78.4 |
0.854 |
Acute Rejection |
80.3/66 |
0.023 |
83.5/70.8 |
<0.001 |
Post transplant hypertension |
76.9/71.9 |
0.374 |
85/77.4 |
<0.001 |
Post transplant DM |
74/73.3 |
0.780 |
79.8/78.8 |
0.726 |
Table 3 Univariate analysis of risk factors of graft survival.
|
Pediatric group |
Adults group |
||
|---|---|---|---|---|
Exp (B) |
P value |
Exp (B) |
P value |
|
Donor age |
1.34 (0.82-2.20) |
0.241 |
1.61 (1.28-2.03) |
<0.001 |
Primary IS |
0.65 (0.31-1.36) |
0.249 |
1.21 (0.90-1.63) |
0.206 |
Acute rejection |
1.72 (1.06-2.81) |
0.030 |
2.01 (1.61-2.51) |
<0.001 |
Post transplant HTN |
1.05 (0.62-1.80) |
0.853 |
1.44 (1.11-1.87) |
0.007 |
Table 4 Multivariate analysis of risk factors of graft survival.
Transplantation is the ideal treatment for pediatrics and young adults. Higher academic qualifications, normal marital life and job recruitments were associated with transplantation compared to regular haemodialysis.2
In our results long term graft outcome was to be superior in adults compared to pediatrics as was reported by other groups.4 The actuarial graft survival at 5 and 10years were 87.24+0.84 , 66.78+1.38 for adults and 83.9+2.28, 58.34+3.53 for pediatrics (p<0.001). Numerous factors share in this long term inferiority in graft survival among pediatrics, the most important is poor compliance and recurrence of original kidney disease.3,5
Donor age was between 30-50years in pediatrics as the majority of donors were parents while in adults were younger as majority was either siblings or spouses. Pediatrics was encouraged for pre-emptive transplantation to avoid dialysis complications and rapid restoration of normal social life. While pre-emptive transplantation carries many advantages, it was reported that it may be associated with higher incidence of graft thrombosis. In our series we noticed higher incidence of graft thrombosis in pre-emptive group.6
We report better graft outcome in our series compared to other reports as all transplantation were done from living donor source. Deceased transplantation is not feasible yet in Egypt. It was believed that religion and cultural factors were behind the difficulties of starting the Deceased program in Egypt. After the success of deceased program in Islamic countries like Iran and Saudi Arabia. Egypt has launched new regulation and national law to regulate transplantation including the initiation of a national deceased program.
Initially, steroid avoidance was adopted for pediatrics in favor to avoid steroid related stunted growth, currently steroid avoidance is the standard immunosuppression protocol for both pediatrics and adults. In our series pediatrics tolerated well steroids avoidance with no impact on long term graft survival, our results in parallel with what have been published from other reports.7 No significant impact of immunosuppression was noted on long term graft survival in pediatrics. In adults steroid avoidance carried 1.7 independent risks on long term graft survival which can be explained by higher incidence of rejection compared to steroid based group; as well it was noticed high levels of tacrolimus after withdrawal of steroids with higher incidence of nephrotoxicity.8 The prevalence of post transplant hypertension in pediatric group was 50.6% and comparable to previously reported from other studies.9
Acute rejection was an independent risk factor of graft failure. One acute rejection increases the risk of long term graft failure 1.7times in pediatrics. While 2.01times the risk of lower graft survival following acute rejection in adults compared to those did not suffer acute rejection. As well donor age and post-transplant hypertension were independent risk factors in adults but have no impact in pediatric recipients.
In conclusion in spite of improved long term results more efforts must be directed toward management of risk factors that hinder further achievements.
None.
The author declares no conflict of interest.

©2015 Akl, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.