eISSN: 2377-4304


Research Article Volume 15 Issue 5
1Ricardo Palma University, Faculty of Human Medicine, Biomedical Sciences Research Institute (INICIB). Lima, Peru
2General Surgeon, Master in Medicine, with mention in Health Administration Doctor in Medicine, Ricardo Palma University, Faculty of Human Medicine, Biomedical Sciences Research Institute (INICIB). Lima, Peru
3Medical Oncologist, Oncology and Prevention Unit, San Juan de Lurigancho. Mg. in Health Services Management, Ricardo Palma University, Faculty of Human Medicine, Biomedical Sciences Research Institute (INICIB). Lima, Peru
Correspondence: Dr. Fabricio Ceferino Alvarez Pérez, MD, Ricardo Palma University, Faculty of Human Medicine, Biomedical Sciences Research Institute (INICIB). Lima, Peru
Received: September 13, 2024 | Published: September 24, 2024
Citation: Casanova AMP, Pérez FCA, Conde GN, et al. The covid-19 pandemic and its effect on maternal health indicators in Latin American countries. Obstet Gynecol Int J. 2024;15(5):207-215. DOI: 10.15406/ogij.2024.15.00760
Introduction: Maternal mortality constitutes one of the most important indicators of public health, and also reflects the response capacity of health systems to the healths needs of one of the most vulnerable groups, such a pregnant women.
Objective: Conduct a bibliographic review of the maternal mortality indicators used by health management teams, before and during the COVID-19 pandemic in Latin American countries.
Methodology: A bibliographic review was carried out by searching for scientific articles related to the topic. In addition, information was collected from epidemiological bulletins updated as of the review date. The PEO question was used (Population: pregnant women. Exposure: before and during the COVID-19 pandemic Result: maternal mortality in the context before and during the pandemic): What are the maternal mortality indicators before and during the COVID-19 pandemic? The search sources were PubMed, Scielo and Google Scholar. The key words were: "Maternal mortality" "Morbidity and mortality indicators" "COVID-19". Articles published from January 1, 2021 to May 30, 2023 were selected.
Results: Of the 5670 articles found, 5654 articles were discarded because they did not meet our criteria for keyword combinations in the title or abstract. Of the 16 articles selected, 12 had research results. Of the total number of articles, there were 4 prospective articles and 8 retrospecitve articles, 4 were considered for conceptual theoretical aspects that are related to the objective of the study.
Conclusion: an increase in the maternal mortality ratio was evident in the pre-pandemic period and during the pandemic compared to the figures from previous years, this was associated with the presence of comorbidities and maternal risk factors as well as the limited supply of health services, lack of intra-and extramural organization.
Keywords: maternal mortality, morbidity and mortality indicators, COVID-19
Maternal mortality is a medical, social, economic, political, cultural and multisectoral problem. It is estimated that 585,000 women die every year due to complications related to pregnancy, childbirth or puerperium in the world, constituting the main causes of death among women of reproductive age in the world. The average maternal mortality rate in Latin America and the Caribbean is 190 deaths per 100,000 live births. Pooled estimates of all-cause mortality for 24 European countries/federal states participating in the European Network on Excess Mortality Surveillance for Public Health Action have shown excess mortality in all groups over 14 years of age, including women of childbearing age and especially pregnant women. The Latin American Center for Perinatology, Women's Health and Reproductive Health (CLAP) of the Pan American Health Organization (PAHO) conducted a study of 447 pregnant women in Bolivia, Colombia, Costa Rica, Honduras, Ecuador, Paraguay, Peru and the Dominican Republic, where 35% died from causes associated with COVID-19, due to lack of admission to the intensive care unit (ICU). The mean maternal age was 31 years and about half of them were obese. Of the women studied, 86.4% were infected before delivery and most cases (60.3%) were detected in the third trimester of pregnancy.1–3
In low- and middle-income countries (LMICs), pregnant women and newborns with COVID-19 are more vulnerable to adverse outcomes. However, to date, there is information.
The data on the epidemiological and clinical characteristics of COVID-19 in pregnant women in Latin America are limited. In the case of Venezuela, data have not yet been integrated into a national surveillance system, so it is not possible to identify maternal-fetal characteristics or hospital admissions of pregnant women for COVID-19. Impact of the COVID-19 pandemic on mortality in Peru.
The number of maternal deaths was significant in 2020 increased by 47.1 % compared to the previous year, with a total of 439 deaths; the main cause is preeclampsia, uterine hemorrhage and COVID-19, being the first cause of indirect maternal death. Subsequently, in 2021, the situation has not changed; according to the Peruvian Ministry of Health (MINSA), there have been 493 maternal deaths due to direct and indirect causes; that is, 12% more than in 2020, not counting late maternal deaths. Since the early 1990s, Peru had been experiencing a significant decline in the maternal mortality rate. In fact, the country was already on track to meet the 3.1 target of Sustainable Development Goal 3 (SDG 3), which aims to reduce the overall maternal mortality ratio to less than 70 per 100,000 live births by 2030, but the epidemic of EVID-19 has generated significant delays.3,4
In many women pregnancy has been affected during the pandemic by COVID-19, as the figures in Peru are clear, it is clear that Peruvian pregnant women have become a vulnerable population and this is represented in the MINSA report, which makes available figures showing an increase in maternal deaths in 2020 to 439 cases, consequently maternal deaths have increased by 42% in relation to the year 2019, thus being a setback for Peru of 10 years.5
Considering the importance of maternal mortality as a public health indicator, as well as a parameter to measure the response capacity and protection of the health system in contingencies to vulnerable populations, the present study aims to conduct a literature review of maternal mortality indicators used by health management teams before and during the COVID-19 pandemic in Latin American countries.
For the present literature review, we used articles in English and Spanish published from January 1, 2021 to May 30, 2023 in the PubMed, Scielo, and Google Scholar search sites. In addition, information was collected from epidemiological bulletins updated to the review date. The clinical question: What are the indicators of maternal mortality before and during the COVID-19 pandemic? PEO question: Population: pregnant women; Exposure: before and during the COVID-19 pandemic; Outcome: maternal mortality in the context before and during the pandemic. The keywords were: "Maternal Mortality" (MeSH Term), "Health Status Indicators" (MeSH Term), "COVID-19" (MeSH Term). The present work is in health priorities "Maternal, perinatal and neonatal health", according to the "Health Research Priorities 2019-2023 of the National Institute of Health.6
Inclusion criteria
Exclusion criteria
Of the 5670 articles found, 5654 articles were discarded because they did not meet our criteria for keyword combinations in the title or abstract. Of the 16 articles selected, 12 had research results. Of the total number of articles, 4 were prospective articles and 8 retrospective articles, 4 were considered for conceptual theoretical aspects that are related to the objective, to carry out a bibliographic review of the maternal mortality indicators used by health management teams before and during the COVID-19 pandemic in Latin American countries.
Table 1 shows the main characteristics of the selected studies, with a publication period of 2021- 2023. The studies were developed in pregnant women from different Latin American countries, ages and levels of education, occupations. The samples were heterogeneous, showing a population of between participants.
|
Authors |
Title |
Year |
Country |
Population |
Design |
|
White A11 |
Maternal mortality as a problem of human rights: the Venezuelan case |
2021 |
Venezuela |
Deaths maternal during period 2000 - 2020 |
Retrospective, Descriptive |
|
González, R. et al.7 |
Increase in maternal mortality and prematurity during the COVID-19 pandemic in Chile |
2023 |
Chile |
All the born, deaths general and fetal since January 1900 to September 2022 |
Prospective |
|
Mendoza MF12 |
Maternal Mortality and the COVID-19 Pandemic in Mexico: A Critical Epidemiological Analysis |
2023 |
Mexico |
Deaths maternal and live births from 1998 to 2020 |
Analytical, Retrospective |
|
Mercedes, K13 |
Impact of the COVID-19 pandemic on maternal morbidity and mortality in the Dominican Republic. |
2023 |
Republic Dominican |
Deaths maternal from 2020 to 2021 |
Analytical, observational, cross-cutting and retrospective |
|
Ortiz S.8 |
Health Status Maternal in Nicaragua, prospects post COVID-19 |
2022 |
Nicaragua |
Mortality Maternal between 2019 y 2021. |
Study Prospective |
|
Sotomayor Valdiviezo, et al.3 |
Mortality in pregnant women with COVID - 19 during the 2020-2021 period in Latin America |
2022 |
Peru |
Mortality in pregnant women with COVID-19 during the period 2020-2021 |
Retrospective |
|
Brendolin M, et al.10 |
Severe maternal morbidity and mortality during the COVID-19 pandemic: a short study in Rio de Janeiro |
2022 |
Brazil |
1609 women pregnant women |
Cohort. Prospective |
|
Maza-Arnedo, et al.9 |
Maternal mortality linked to COVID -19 in Latin America: Results from a multi-country collaborative database of 447 deaths |
2022 |
Countries of Latin America (Honduras, Paraguay, Colombia, Ecuador, Peru, Republic Dominican Republic, Bolivia and Costa Rica) |
Mortality of 447 pregnant women. |
Study observational, prospective. |
|
Castañed a, et al.14 |
Maternal mortality in Colombia during the COVID-19 pandemic: time series and social inequities. |
2023 |
Colombia |
6342 |
Retrospective, descriptive |
|
Montoya N, et al.15 |
Impact of COVID-19 in reproductive health: maternal deaths |
2022 |
Peru |
Maternal during the period 2020- 2021 |
Descriptive, Retrospective |
|
Orellana J, et al.16 |
Maternal excess mortality in Brazil: Regional inequalities and trajectories during the COVID-19 epidemic |
2022 |
Brazil |
3291 deaths maternal |
Retrospective |
|
Esquenazi Borrego, et al.17 |
Maternal mortality in Brazil and Cuba: study comparative |
2021 |
Brazil - Cuba |
Deaths maternal during 2005 period-2017 |
Retrospective |
Table 1 Titles, authors and design of research papers related to maternal mortality
The following was found in prospective studies
Gonzalez R. et al.7 in their research: Increase in maternal mortality and prematurity during the COVID-19 pandemic in Chile, describes according to the national database of the Department of Informatics of the Ministry of Health of Chile (DEIS) where they included all births, general and fetal deaths from January 1990 to September 2022. A comparison is made between the basic maternal and perinatal indicators for the last 30 years and during the pandemic. There was an acceleration towards a decrease in the overall birth/death ratio from 1.9 pre-pandemic to 1.4 in the third year of the pandemic. The maternal mortality ratio increased from 19.1 pre-pandemic to 28.1 per 100,000 live births.7
Ortiz S. conducted a prospective trial, to investigate the State of Maternal Health in Nicaragua, post COVID-19 perspectives, this opinion article makes an exploratory analysis of the effect that the coronavirus had on the evolution of maternal mortality in Nicaragua. The pandemic situation caused by the Coronavirus, declared by the World Health Organization in March 2020, could slow down and delay the decline in maternal mortality, which was expected to be less than 70 deaths per 100,000 live births by 2030, according to target 3.1 of the United Nations Sustainable Development Goal (2015). From 1990 to 2017, the global maternal mortality ratio (MMR), decreased by 45 percentage points, from 385 to 211 deaths, however, it is still very high and predominates in poor countries with accentuated social inequalities (WHO, 2017) In Nicaragua 6 out of 10 maternal deaths (59%), occur in vulnerable groups, with high incidence of extreme poverty (MINSA, 2018). This pandemic challenges the continuity of global development. The impact of COVID-19, in Nicaragua is mild, compared to countries in the Americas, as of November 2021 totaled 16877 cases and 209 deaths, according to Johns Hopkins University (Johns Hopkins Medicine, 2021). However, the effect on the country's economy, it is reported, may hold back its development, with losses estimated at U$29.5 million (2018-2023), 2.3 times the nominal gross domestic product (GDP) of 2020 (Government of Nicaragua, 2021).8
Maza-Arnedo, et al.9 conducted a prospective, observational clinical trial to investigate COVID-19-related maternal mortality in Latin America. This study describes the characteristics of maternal deaths from a comprehensive database from several countries in Latin America during the COVID-19 pandemic. It also revealed the barriers faced by Latin American pregnant women in accessing intensive care services when required. Decision-makers need to strengthen awareness of severity and referral strategies to avoid potential delays. Data were collected on 447 maternal deaths. All pregnant and puerperal women included had a positive SARS-CoV-2 test, regardless of the cause of death. The country reporting the highest number of deaths in this database was Honduras (n=126), followed by Paraguay (n=86), Colombia (n=84), Ecuador (n=55), Peru (n=34), Dominican Republic (n=30), Bolivia (n=21), and Costa Rica (n=11).9
Brendolin M, et al.10 in their study: Severe maternal morbidity and mortality during the COVID-19 pandemic: a short study in Rio de Janeiro, with a population of 1609 pregnant women, found that 25.5% were infected with SARS-CoV-2, based on reverse transcriptase polymerase chain reaction or antigen testing. There were 21 deaths and 67 ICU admissions in 4% of the participating cohort. The incidence of severe maternal morbidity and mortality was higher during the Gamma wave than during the Delta wave. Vaccination conferred protection against the endpoint. Factors associated with severe morbidity and mortality included cesarean section, SARS-CoV-2 infection in the third trimester, and comorbidities.10
The following was found in the retrospective studies
Blanco Andy in his study: Maternal mortality as a human rights problem: the Venezuelan case, describes that maternal mortality has increased in recent years. Between 2010-2014 it reached 70.45 maternal deaths per 100000 registered live births, the highest figure since the five-year period 1970-1974; in this context, in 2014, the Convention on the Elimination of All Forms of Discrimination Against Women (CEDAW) expressed concern about the high rates of maternal mortality and the high number of teenage pregnancies. By 2019, the maternal mortality ratio was still increasing and was at 112.2 per 100000 live births, by 2020, the country would have exceeded 120 obstetric deaths.11
Mendoza MF in his research: Maternal Mortality and the COVID-19 Pandemic in Mexico: critical epidemiological analysis, describes: an analysis using the death database of the Sistema de cubos dinámicos de la Dirección General de Información en Salud [DGIS] de la Secretaría de Salud de México, with validated official data from 1979 to 2020. It included a cohort of 21.4 million deaths registered in Mexico, of which 9,319,102 (43.6%) were women. For that time period, 58,321 deaths classified as maternal were recorded. A weighted maternal mortality rate of 4.2 per 100,000 women of childbearing age, which was 2.14 times higher in the period 1979 -1997 (6.2/100K vs. 2.9/100K); the highest concentration of deaths was observed in the 20-39 years age stratum and the average age at death was almost 29 years. Regarding pandemic data by COVID-19, during the first year of the pandemic (2019 to 2020), the increase in the maternal mortality rate was 57.6% and 19.1% in the following years (from 2020 to 2021).12
Mercedes, K in her study: Impact of the COVID-19 pandemic on maternal morbidity and mortality in the Dominican Republic, using maternal morbidity and mortality data from SINAVE, estimated the ratio of extreme maternal morbidity and the ratio of maternal mortality by cause of death. The results indicate that the COVID-19 pandemic had an impact on maternal morbidity and mortality in the Dominican Republic. The extreme maternal morbidity ratio showed a decrease in 2020 compared to 2019, from 12.1 to 10.4 per 1000 live births; however, the maternal mortality ratio went from 91.4 to 124.2 maternal deaths per 100,000 live births in these years, respectively, showing the impact that COVID-19 had on pregnancy care for women and newborns due to the interruption of health services due to the confinement.13
Castañeda, et al.14 in their study: Maternal mortality in Colombia during the COVID-19 pandemic: time series and social inequities, describes that in 2019, the year prior to the pandemic, Colombia reported 511 maternal deaths with an MMR of 80 maternal deaths per 100,000 live births. The time series model, estimated 483 deaths expected for 2020, considering the behavior of 2019, however, 544 early and late maternal deaths were recorded (MMR of 87 per 100000 live births). This represents an excess mortality rate of 12.6% (95% CI - 21.4% to 95.7%) of deaths.14
Sotomayor Valdiviezo, et al conducted a review article: Mortality in pregnant women with COVID - 19 during the period 2020-2021 in Latin America, a systematic review of scientific articles published from January 1, 2020 to December 31, 2021, made in the Medline databases via PubMed, SciELO, Google Scholar. The question was: What is the mortality in pregnant women with COVID-19 during the period 2020-2021 in Latin America? using the following descriptors controlled: "Gestantes, "COVID-19", "Mortality. Population: Pregnant women, Exhibit: COVID-19, O/Denlace: Mortality. Ten studies showing results were included in the selection process. They were conducted in pregnant women with a positive COVID-19 test and had a study population ranging from 40 to 29416 participants. Maternal mortality in intensive care units was found to be 49% in Mexico City. A study in 8 Latin American countries reported that 86.4 % of women were infected before delivery and 60.3 % of women were infected before delivery.
% in the third trimester. These studies coincide in describing comorbidities in pregnant women with COIVD-19, among which hypertensive disorders stand out.3
Montoya N, et al.15 conducted an investigation: Impact of COVID-19 on reproductive health: maternal mortality. It dealt with maternal mortality as the study is a qualitative analysis with a descriptive and critical scope. Firstly, the social and economic effect of maternal mortality, secondly, epidemiological data and technical standards, and thirdly, the impact of COVID-19 on the pregnant population. The increase in maternal mortality of 45.4% and 56% in 2020 and 2021 with respect to 2019 was analyzed. The study highlighted the pre-pandemic achievement reached in 2015 in maternal health with a remarkable decrease of 50% between 2000 and 2019, to later succumb to the pandemic in a 12-year setback and become the third and first cause of indirect maternal death in 2020 and 2021.15
Orellana J, et al.16 conducted an article: Excess maternal mortality in Brazil: Regional inequalities and trajectories during the COVID-19 epidemic. They evaluated maternal deaths from the Mortality Information System of the Ministry of Health, assessing excess deaths between March 2020 and May 2021 using overdispersion-adjusted generalized additive quasi-Poisson models. There were 3291 maternal deaths reported during the study period, resulting in 70% excess deaths regardless of region, while in the North, Northeast, South and Southeast regions, with excess deaths regardless of age group. There was an increase in deaths in the March to May 2021 quarter, regardless of region and age group. In the Southeast region, an increase in deaths was observed for the 25-36 age group, regardless of the quarter evaluated, and in the North, Central-West and South regions, the only period in which excess deaths were not observed was September - November 2020. Finally, the study showed an increase in deaths regardless of the quarter in the 37-49 age group in the North region, and the South region showed an explosive behavior from March to May 2021, with an increase in deaths of 375%.16
Esquenazi Borrego, et al.17 in their study: Maternal Mortality in Brazil and Cuba: a comparative study, they used data from the Informatics Department of the Brazilian Unified Health System, and the statistical yearbooks published by the Cuban Ministry of Public Health and the National Bureau of Statistics and Information. In Cuba, the Maternal Mortality Ratio figures remain with values always lower than those of the country itself in 2005; however, as of 2013 they show an increasing behavior. In Brazil, on the other hand, they are higher than those of Cuba and never decrease in relation to the year 2005; and show a marked upward trend.17
Table 2 shows the Maternal Mortality Indicators in Latin America, according to the articles collected. Among which is the Maternal Mortality Ratio Indicator.
|
|
|
Pre pandemic |
Pandemic |
|||
|
Indicators |
Countries |
2015 - 2017 |
2019 |
2020 |
2021 |
Trend |
|
Reason for mortality maternal |
Peru15 |
45,4% |
56% |
Start of Pandemic: Increase in 2019 to 2020 from 45,4% |
||
|
During the pandemic: 2020 - 2021 increase in 7,3% |
||||||
|
Venezuela11 |
112,2% |
120% |
||||
|
Chile7 |
19,1% |
28,1% |
22,0% |
Increase the first year of pandemic in 56% |
||
|
Mexico12 |
2015 |
34,2% |
53,9% |
64,2% |
2020 - 2021 |
|
|
35,0% |
Increase in 19.1% during pandemic |
|||||
|
Colombia14 |
- |
80,0% |
87% |
- |
Increase start pandemic of 12.6%. |
|
|
Republic Dominican13 |
RMM average between 2015-2019 |
91,42% |
124,2% |
153,7% |
||
|
|
105,96% |
|
|
|
|
|
Table 2 Maternal mortality indicator: maternal mortality ratio
Regarding the Pre-pandemic period for COVID-19
Regarding the COVID-19 Pandemic Period
No data on maternal mortality were found in the articles from the following countries: Brazil, Cuba and Nicaragua, according to the articles investigated (Figures 1A–1C).
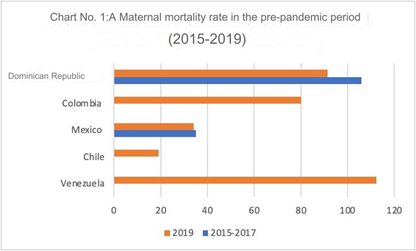
Figure 1a Maternal Mortality Ratio during the Pre-Pandemic Period in Latin American countries, in the period 2015-2019.
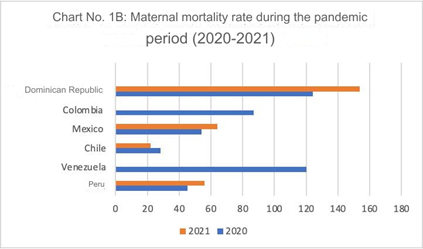
Figure 1b Maternal Mortality Ratio during the Pandemic COVID-19 Period in Latin American countries in the period 2020-2021.
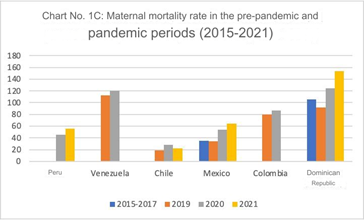
Figure 1c Pre-pandemic and pandemic maternal mortality ratio in Latin American countries in the period 2015-2021.
Table 3 shows the Maternal Mortality Indicators in Latin America according to epidemiological data. Among which is the Maternal Mortality Ratio Indicator.
|
|
|
Pre pandemic |
Pandemic |
|||
|
Indicators |
Countries |
2017 - 2018 |
2019 |
2020 |
2021 |
2022 |
|
Reason mortality maternal |
Peru18 |
2018: 360 MM |
302 MM |
439 MM |
493 MM |
288 MM |
|
Mexico19 |
33,9% |
33,7% |
51,1% |
49,9% |
30,4% |
|
|
Ecuador20 |
41,1% |
37% |
54,3% |
43,5% |
101 MM |
|
|
Colombia21 |
45,3% |
50,7% |
66,7% |
40,4% |
||
|
Chile22 |
23% |
19% |
31,2% |
|||
|
Republic Dominican23 |
196 MM |
164 MM |
206 MM |
260 MM |
142 MM |
|
|
119% |
96% |
131% |
171% |
100,91% |
||
|
|
Brazil24 |
2017 59,7% |
60,7% |
72% |
|
|
Table 3 Maternal mortality indicator: maternal mortality ratio. According to epidemiological situation
MM, Number of Maternal Deaths Source: Own elaboration.
According to epidemiological data
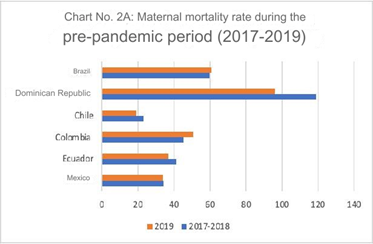
Figure 2a Maternal Mortality Ratio during the Pre-Pandemic Period in Latin American countries in the period 2017-2019.
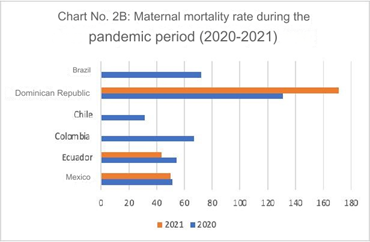
Figure 2b Maternal Mortality Ratio during the Pandemic COVID-19 Period in Latin American countries in the period 2020-2021.
Maternal health indicators have been affected by the COVID-19 pandemic, evidencing the impact it had on pregnant women and newborns, due to the interruption of health services due to confinement and the consequent reduction in the supply of health services, not only in infrastructure, but also in the number of human resources.13
Prior to the pandemic, there was evidence of a worldwide trend of decreasing maternal mortality; WHO notes that from 1990 to 2017, the MMR decreased by 45 percentage points, from 385 to 211 deaths, however, it still turns out to be very high, predominating in poor countries with accentuated social inequalities (WHO, 2017). This is due to the context of poverty and geographical conditions in the regions, which limit access to timely prenatal services, delivery or puerperium care with trained personnel and advanced health technologies. Social and cultural aspects also play a role characteristic of the different ethnic groups living in the region.8
Many Latin American countries had shown a reduction in their maternal mortality indicators during the pre-pandemic period, but later succumbed to the COVID-19 pandemic in a notable setback, constituting one of the leading causes of indirect maternal death. Due to the COVID-19 health emergency, human and financial resources of various health programs were frequently diverted to respond to the outbreak of the infectious disease, affecting sexual and reproductive health services. In addition, the reduction of health personnel to provide continuous sexual and reproductive health services, the restriction of access to health services, with health facilities closed or with reduced opening hours, and patients' fear of contagion, thus preventing them from going to health centers. In the case of Peru, the insufficient public health budget of 3.3% of the Gross Domestic Product (GDP), according to World Bank figures Peru allocated 13471 billion soles in the years 2016 and 18495 billion soles in 2020 in the COVID-19 pandemic, which affected in the quality of budget allocation and execution. In health, this was reflected firstly by the weak management and regulatory capacity and high turnover of officials at the three levels of execution; secondly by the fragmentation and disarticulation of the various public and private health providers in the country.15
In the work done by Diguisto C. and collaborators, where the study population was 8 European countries with permanent surveillance system, they show maternal mortality data collected during the pre-pandemic period, where Norway stands out with the lowest rate (2.7) in the period 2014 - 2018, followed by Denmark with 3.4 in the period 2013 - 2017. The rates of the highest mortality rates occurred in the countries of Slovakia and the United Kingdom, with a maternal mortality rate of 10.9 and 9.6, respectively. In contrast to the results found in Latin America, it reflects a great variation among maternal mortality rates, reflecting the precariousness of the health system in our region.25
It is also observed in the study conducted by Thoma ME and collaborators, that based on data collection during the pre-pandemic period, the mortality rate in the USA was 25.1%, compared to the 2020 pandemic period, where a relative increase of 33.3% was found, demonstrating that they have a higher mortality rate compared to the countries of the European continent.25
The causes of maternal mortality can be direct or indirect, with direct causes predominating in Latin America. Direct maternal mortality is due to gynecological-obstetric causes, with obstetric hemorrhage being the leading cause of direct maternal death, followed by hypertensive disorders. Indirect maternal mortality is due to non-obstetric or pre-pregnancy causes, currently the most frequent cause is COVID-19. Most cases of maternal mortality occur during the puerperium stage, with the majority of cases occurring in health facilities.26
According to the National Center for Epidemiology, Prevention and Disease Control - MINSA, the deaths reported were considered as direct and indirect, occurring up to 42 days after the end of gestation. In the period 2015-2019 (pre-pandemic), direct causes had a value of 64.7%, compared to indirect causes with a value of 35.5%. In the year 2020, direct causes decreased to 56.9% and indirect causes had a value of 35.5% indirect causes increased to 43.1%. In the year 2021, it was seen that both causes were equally related, that is, 50% for each, and in the year 2022, there was a new increase in direct causes to 64.3% and a decrease in indirect causes to 35.7%. In conclusion, the direct causes are of higher mortality, however, due to external factors that had the pandemic situation, the number of deaths was exacerbated.18
As it should be noted, some factors from the managerial, supply and demand point of view, which favored the increase in the maternal mortality ratio, stand out:
An increased risk of maternal-perinatal morbidity and mortality associated with SARS-COV-2 infection, in addition to the vulnerability condition itself, probably due to the difficult access to medical care and the reduction of health care workers and intensive care unit beds in low- and middle-income countries (LMICs), such as Venezuela.4
A study in 8 Latin American countries reported that 86.4 % of the women were infected with COVID-19 before delivery and 60.3 % in the third trimester, and also described comorbidities in pregnant women with COVID-19, including hypertensive disorders, another factor related to the increase in the mortality indicator. They included cesarean section as another factor associated with morbidity and mortality.3,10
During the pandemic, an observational clinical trial by Maza-Arnedo, revealed the barriers faced by pregnant women in Latin American countries to access acute care services when required. Therefore, decision-makers must prepare health systems, in their service delivery components, financing and referral strategies, to avoid possible delays.9
Likewise, the research by Montoya and collaborators determined that the impact of the COVID-19 pandemic has caused a deterioration in the Peruvian health system, which is reflected in the response capacity and quality of health facilities, as well as in the equity of service providers, generating an increase in maternal health maternal deaths in 2020 and 2021, becoming an indirect cause of death in maternal mortality.15
Despite significant improvements in maternal health over the past few years, there are still large inequalities based on place of residence and educational level. Skilled care in childbirth makes the difference between life and death. For this reason, quality policies for maternal health services are important to guarantee the health and life of pregnant women.27
The delay in the analysis of maternal mortality, according to WHO, is due to the difficulty in recognizing the signs, decision making, lack of access and the problem in the health system. Factors that prevent women from receiving or seeking care during pregnancy or childbirth are health system failures that result in poor quality care, including disrespect, mistreatment and abuse; an insufficient number of health workers, who also lack adequate training; shortages of essential medical supplies; and poor accountability in health systems. Social determinants, such as per capita income, access to education, race and ethnicity, as well as external factors that contribute to health system instability and fragility, such as climatic and humanitarian crises. In order to improve maternal health, barriers limiting access to quality maternal health care must be identified and addressed, both at the health system and societal levels.28
Improving maternal health is essential to address some of the underlying causes of maternal mortality, which is a global public health problem, as it represents an important indicator of human development for countries.27
Maternal mortality is a medical, social, economic, political, cultural and multisectoral problem. This pandemic not only affected the health of the population, but also challenged the continuity of world development. Consequently, it recommends establishing care strategies with protocols according to the level of intra- and extramural care, the differentiation of health services, with monitoring healthy and personalized from the maternal comorbidities that were exacerbated in the context of the pandemic, to promote telemedicine in addition to face-to-face consultations, and to expand the capacity of critical care beds for this group of patients. At the same time, pregnant women should be considered as a vulnerable population, requiring timely vaccination coverage and other intramural procedures. Finally, we recommend that information should be expanded in other Latin American countries, in order to formulate an approach, organization and management of health services in the face of an upcoming pandemic.28
The present study has several limitations. One of the limitations was to obtain in the studies, the standard indicator of the ratio of maternal mortality. For example, in Peru, only the total number of maternal deaths was reported, but not the mortality ratio, in addition to an underreporting of mortality among pregnant women, and national studies were scarce.
In conclusion, there was an increase in the maternal mortality ratio in the pre-pandemic period and during the pandemic compared to previous years, which was associated with the presence of comorbidities and maternal risk factors, as well as with the limited supply of health services and lack of intra- and extra-mural organization.
None.
None.
Authors declare that there is no conflict of interest.

©2024 Casanova, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.