eISSN: 2377-4304


Research Article Volume 14 Issue 2
1Department of Anatomy, College of Medicine, King Saud University, Riyadh, 11523, Kingdom of Saudi Arabia
2Embryology Laboratory, Anova Fertility & Reproductive Health, Toronto, Ontario, M2N 6S6, Canada
Correspondence: Murid Javed, DVM, MSC (Hons), PhD, Embryology Laboratory, Anova Fertility & Reproductive Health, 25 Sheppard Ave (W), Suite 650, Toronto, ON, M2N 6S6, Canada, Tel +1-416-731-9885
Received: April 01, 2023 | Published: April 11, 2023
Citation: Alfhead NK, Shaheen S, Al Yahya K, et al. Effects of uterine polyps on embryo implantation in IVF cycles. Obstet Gynecol Int J. 2023;14(2):65-67. DOI: 10.15406/ogij.2023.14.00696
Embryo implantation requires healthy uterine endometrium for natural or assisted reproductive technology conception. However, in presence of any endometrial anatomical abnormality or disease, implantation is affected. Uterine or endometrial polyps are over growths of endometrial cells that extend into the uterine cavity. They are usually noncancerous. There can be one or many polyps. They range in size from a few millimeters to several centimeters or larger. They may cause vaginal bleeding in between periods, heavy periods, frequent or unpredictable periods and infertility. The objective of this study was to find out effects of endometrial polyps on embryo implantation in assisted reproductive technology cycles of Saudi women being treated at an infertility clinic. This was a case-control study. The participants were in ratio of 5:1 i.e., for every 5 patients there was one control. The polyp diagnosis was carried out with ultrasound and endometrial biopsy. We observed high incidence of implantation failure in patients with uterine polyps as compared to that in the control patients. The results of this study indicated that the presence of endometrial polyps is a risk factor for infertility and failure of conception after in vitro fertilization.
Keywords: uterine polyps, implantation, IVF, ICSI, endometrial biopsy, implantation failure, pregnancy
Infertility is one of the emerging medical problems. Parenthood is one of the most sought purpose of couples. However, many couples can’t attain spontaneous conception and may require medical intervention to manage their infertility.1 The infertility causes distress in women. The level of distress increases as the marriage duration, desiring time for a baby and the duration of infertility treatment increases.2 There are several treatment options to help infertile couples, such as medical treatment, surgical treatment, and assisted reproductive technology (ART). When medical and surgical treatments fail, ART facilitates and allows carrying out fertilization and growth of early embryos outside the body. For this reason, this treatment evades various disease conditions in females like disorders of ovaries or fallopian tubes and even in males’ problems of sperm that are not treatable by surgical or medical interventions. The selection of treatment relies on the aetiologies, effectiveness, price, and accessibility of choices and can be influenced by societal, traditional, and religious concerns.1,3
The endometrial polyp is an abnormal growth that contains glands, stroma and blood vessels outgrowing from the endometrium and occupies space small or large enough to fill the uterine cavity. The matrix of polyps consists of fibroblast-like fusiform cells and thick-walled large blood vessels.4 Most often polyps are present in the fundus and in the cornual area. They range in size from approximately 5 mm to as large as filling the whole uterine cavity. The endometrial polyps can be asymptomatic. They have been implicated in about 50% of cases of abnormal uterine bleeding and 35% of infertility5,6 and can reduce pregnancy rate, increase miscarriage rate, and interfere with sperm transport. Endometrial polyps have been found in about 25% of females with unexplained infertility.7
A number of studies highlighted factors responsible for successful embryo implantation in IVF procedures.8,9 However, studies on effects of endometrial polyps on implantation especially in the Kingdom of Saudi Arabia (KSA) are still inadequate.10 Therefore, the aim of this study was to provide current knowledge and prevalence of endometrial polyps, their association with infertility, and their role in the efficiency of embryo implantation in IVF procedures.
The study was conducted in collaboration with a very busy IVF centre in Riyadh, Saudi Arabia. The case to control ratio was 5:1, i.e., one control for every 5 cases. Endometrial polyp diagnosis was carried out by endometrial biopsy and pelvic ultrasound examination. The ovarian stimulation, oocyte collection, oocyte fertilization and embryo culture were carried out using recommended protocol by the Thuriah Medical Centre, Riyadh.
For all the participants, IVF cycle data and pregnancy status were recorded. For biopsy, a small tissue specimen about 2 cm x 0.5 cm was taken, fixed in 10% neutral- buffered formalin, dehydrated by ascending grades of ethyl alcohol 10%, 20%, 50%, 95%, and 100%, cleared in xylene and embedded in soft paraffin.11 Each paraffin block was cut into 4 µm thick sections, mounted onto a slide and stained with Haematoxylin and Eosin stains (H&E).
The digital scan of each slide was viewed at 100x and analysed using Nikon AmScope software. The transvaginal ultrasound image was analysed using Sonoscope S60 software. For all participants blood samples were collected to measure E2 level in the serum by Abbott Architect. All data were entered in Excel sheet and descriptive data analysis was carried out for the 50 study patients. The pregnancy rates were recorded for the study and control groups. The research protocol was approved by Thuriah Medical Centre’s Institutional Review Board. An informed written consent was obtained from each study participant.
Haematoxylin and Eosin-stained section of endometrial tissue is shown in Figure 1A and 1B. The normal blood vessel wall with normal distribution is reflected by “a” and normal size of endometrial gland lined with columnar cells with uniform direction is indicated by “b”. The endometrium from patients having polyps is shown in Figure 2C and 2D.
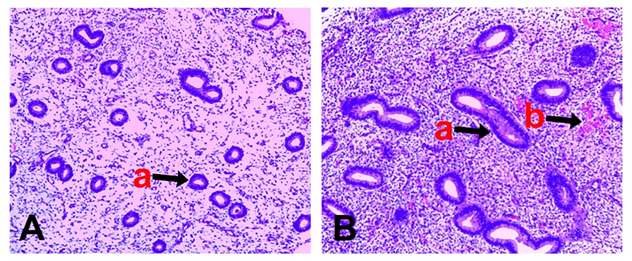
Figure 1A and 1B Haematoxylin and Eosin-stained sections of normal endometrium: normal endometrium glands are indicated by “a” and blood vessel is indicated by “b”.
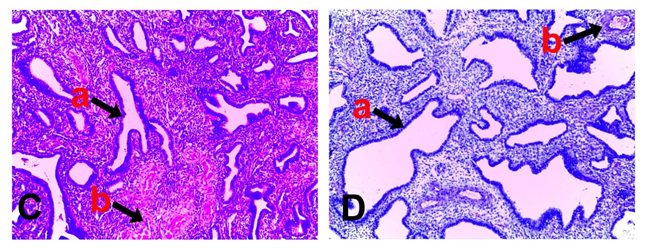
Figure 2C and 2D Haematoxylin and Eosin-stained section of abnormal endometrial tissues from patients with endometrial polyps; (a) Dilated glands in different directions and (b) Thick walls of blood vessels.
The endometrial glands (a) are dilated in different directions and the walls of blood vessels are thickened.
When comparing the E2 levels between patients without and with endometrial polyps, it was found that majority (70%, n=35) of patients with endometrial polyps had high E2 levels, 20% (n=10) had normal E2 levels, and 10% (n=5) had low E2 levels. The majority of patients without endometrial polyp showed normal E2 levels in most cases (Figure 3).
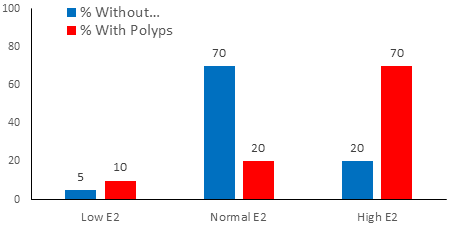
Figure 3 Comparison of E2 levels between without polyp and with polyp groups. Without polyp group is indicated by blue colour and with polyps group is shown in red colour.
Regarding the pregnancy rates in patients without and with endometrial polyps, it was found that 84% (n=42) of the patients with endometrial polyps had negative pregnancy test, while 70% (n=7) of the patients without endometrial polyp had positive pregnancy test (Figure 4).
The results of this study indicate that the presence of endometrial polyps increases chances of failure in assisted reproductive technology cycles. Previously published studies indicated that the level of failure depends on size of the polyp12 however, in the present study, no size measurement was made, the diagnosis of the endometrial polyp was taken as a whole. A study [7} reported that the presence of endometrial polyps decreases the uterine receptivity thus resulting in lower implantation. These authors suggested to perform a detailed evaluation of the uterine cavity and if any endometrial polyp is identified, polypectomy should be performed before initiating infertility treatment to improve fertility. Another report recommended to adopt a policy of egg retrieval, cryopreserving the embryos, performing polypectomy and transfer the embryos in the future reproductive cycle to increase the “take-home baby” rate.13 Although endometrial polypectomy is recommended in infertility patients, however, more studies are needed to verify that endometrial polypectomy itself will increase the pregnancy rate as small size polyps regress spontaneously.14,15 The endometrial polyp formation could be due to the localised chronic inflammation. The inflammation results in the formation of new blood vessels and growth of tissue. Cyclooxygenase-2 (COX-2), a key enzyme involved in the production of prostaglandin in mast cells, was significantly higher in patients with polyps as compared with those with normal endometrium.5 The mast cells initiate and control inflammation through their secretion of cytokines and growth factors. The localized chronic inflammation results in reduced implantation and pregnancy rate.
Another factor that may affect the pregnancy is the high oestrogen level in patients during the assisted reproductive technology cycle. Estradiol at physiological level is required to prime the endometrium for further endometrial growth by progesterone to prepare a suitable environment for embryo implantation. Higher than physiological levels of E2 are not suitable for embryo implantation and may cause excessive stimulation of endometrial glands resulting in the formation of uterine polyps. The polyps are oestrogen-dependent structures15 and their pathogenesis is related to the high level of estrogen in the body. The progesterone can slow down recurrence of endometrial polyps. However, long-term systemic use of hormone drugs has side effects and inconvenience, and many patients lack compliance. Therefore, it is necessary to develop some new drugs or ways that can reduce the recurrence of endometrial polyps, increase implantation, and improve the quality of life of patients. The present treatment options for endometrial polyps are observation and waiting, progesterone drug therapy; and surgery.4
Implications for practice
The endometrial polyps reduce implantation rate, increase miscarriage, and interfere with sperm transport. The level of failure depends on size of the polyp. A detailed evaluation of the uterine cavity is required and if any endometrial polyp is present, polypectomy should be performed before initiating infertility treatment. The endometrial polyps are estrogen dependent.
The results of this study indicate that infertility patients having endometrial polyps had much higher levels of E2 in blood resulting in lower pregnancy rate after assisted reproductive cycle. The patient number in this study was small, therefore, larger studies are needed to find out relationship between high E2, endometrial polyps and the implantation failure.
We acknowledge support from Thuriah Medical Center and its Embryology staff for providing us opportunity to conduct this study.
Submission declaration
The work described has not been published previously. It is not under consideration for publication elsewhere. Its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere including electronically in the same form, in English or in any other language, without the written consent of the copyright-holder.
Data declaration
The research data contains patient specific information and is confidential.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
All authors declare any financial interest with respect to this manuscript.

©2023 Alfhead, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.