eISSN: 2377-4304


Research Article Volume 14 Issue 2
1Department of Obstetrics and Gynaecology. Institut d'Investigació Biomèdica Sant Pau - IIB Sant Pau. Universitat Autònoma de Barcelona. Hospital de la Santa Creu i Sant Pau, Sant Quintí 89, 08025, Barcelona, Spain
2Women and Perinatal Health Research Group, Institut d’Investigació Biomèdica Sant Pau (IIB SANT PAU), Sant Quintí 77-79, 08041 Barcelona, Spain
3Primary Care Interventions to Prevent Maternal and Child Chronic Diseases of Perinatal and Developmental Origin Network (RICORS-SAMID) (RD21/0012), Instituto de Salud Carlos III, Madrid, Spain
Correspondence: Monica Cruz-Lemini MD PhD, Obstetrics and Gynecology Department, Hospital de la Santa Creu i Sant Pau – IIB Sant Pau, Sant Quintí 89, 08025, Barcelona, Spain, Tel +34 93 553 70 48/+34 93 553 70
Received: April 14, 2023 | Published: April 25, 2023
Citation: Bailón-Queiruga M, Cruz-Lemini M, Medina Mallén MC, et al. Double balloon catheter versus vaginal prostaglandins for induction of labor: an observational ambidirectional cohort study. Obstet Gynecol Int J. 2023;14(2):77-82. DOI: 10.15406/ogij.2023.14.00699
Aim: To compare effectiveness and safety of double balloon catheter and prostaglandins for induction of labor.
Methods: an observational ambidirectional cohort study was conducted at a tertiary care university hospital. A total of 666 women with a Bishop score ≤6 requiring labor induction were included. A cohort of 418 patients with double balloon catheter were compared with a retrospective cohort of 248 women induced with prostaglandins, either misoprostol or dinoprostone. Perinatal outcomes were compared between groups, with a p<0.05 considered statistically significant.
Results: The cesarean-section rate was 27% in the double balloon group, compared with 27.8% in the prostaglandin group (p=0.352). The mean induction time-to-delivery was longer in the double balloon group as compared to the prostaglandin group (26.6±9.3 hrs vs 19.1±8.6 hrs, p<0.001). Hyperdynamia and umbilical-cord arterial pH<7.1 rates were significantly lower with the mechanical method compared to prostaglandins (p<0.001 and p=0.043, respectively). Other maternal and neonatal outcomes were similar between the groups.
Conclusions: Double balloon catheter has similar effectiveness in terms of cesarean-section rate compared to prostaglandins, but with a better safety profile. However, the balloon catheter is associated with a longer time-to-delivery compared to prostaglandins.
Keywords: Cervical ripening, double balloon catheter, induction of labor, prostaglandins, vaginal birth
BS, bishop score; CS, cesarean-section; CR, cervical ripening; CTG, cardiotocography; DBC, double balloon catheter; FHR, fetal heart rate; IOL, induction of labor; NICU, neonatal intensive care unit; PTG, prostaglandins
Induction of labor (IOL) is one of the most common procedures in obstetrics and it is estimated that 1 out of four women has labor induced.1,2 IOL artificially initiates effacement, dilation and softening of the cervix and the onset of uterine contractions, with the aim to end pregnancy through vaginal delivery.3 This intervention achieves better maternal and neonatal outcomes as long as the risks of continuing pregnancy outweigh the benefits.4
In women with an unfavorable cervix, IOL begins with cervical ripening (CR), to minimize the rate of failed induction.3 This ripening can be achieved pharmacologically (mainly with prostaglandins [PTG] such as misoprostol or dinoprostone) or using mechanical methods (mostly balloon catheters with either single balloon [Foley catheter] or double balloon [CRB-Cook®]).4 Both PTG and balloon catheters have shown to be acceptable and safe, but there is still no consensus about which is the best approach for IOL.5 However, there is consistent evidence on increased risk of hyperstimulation and possible consequent loss of intrauterine fetal wellbeing with the use of pharmacological methods during CR.6,7 In contrast, mechanical methods have been reported to be safer than PTG in terms of neonatal outcomes.8,9
We present here a real-world setting implementation of double balloon catheter (DBC) as first option for all patients requiring IOL with intact membranes, comparing them with a historical cohort before introduction of DBC at our institution, where only PTG were used. The main aim of the study is to compare the effectiveness of both methods, measured as the caesarean section rate, as well as their safety.
We conducted an ambidirectional cohort study where we compared two cohorts of IOL: one performed with DBC and the other with PTG (misoprostol or dinoprostone). The DBC group was an ambidirectional cohort composed of 200 patients reviewed retrospectively, who underwent an IOL from January 2018 to September 2019, and 218 patients prospectively recruited during a 12-month period from October 2019 to October 2020. The PTG cohort was retrospective and included 248 cases from January 2016 to December 2017, when DBC was not yet used in the hospital.
Our study was conducted in a tertiary center. The protocol was approved by our institution’s Ethics Committee and Biomedical Research Institute, IIBSP-CRB-2019-70). All patients gave informed consent and their anonymity is guaranteed.;
Patients included were women over 18 years old, singleton pregnancies, from 37+0 to 41+6 weeks, which required IOL and had a Bishop score (BS) <7. Exclusion criteria included contraindication for vaginal delivery, prior cesarean delivery, rupture of membranes, breech presentation, fetal distress, major fetal malformation, or stillbirth.
At the time of inclusion, maternal age, comorbidities (such as diabetes, hypertension, and thyroid disease), parity, indication for IOL, initial BS and gestational age were recorded.
DBC (CRB Cook® with stylet) was the first-line method applied to all IOL with intact membranes from 2018 onwards. The device was placed by the physician or midwife with a speculum, and both balloons were filled with 80 cc of saline solution, except in cases of poor tolerance, in which the maximum volume tolerated by the patient was set. If positive vaginal or rectal swab for Group B Streptococcus, antibiotic was started at the time of placement (intravenous penicillin G, 5 million IU loading dose, followed by 2.5 million IU every 4 hours until delivery). A 30-minute cardiotocogram (CTG) was performed before and after balloon placement. The DBC was left in place for 12 hours, unless it was spontaneously expelled.
After removal/expulsion of the balloon, expectant management was carried out for two hours, favoring cephalic pelvic engagement. After that period, amniotomy was performed systematically or PTG were commenced if BS was still <3 and amniotomy was not possible. PTG doses after DBC were: for vaginal misoprostol (PTG-E1) 25 mcg every 4 hours with a maximum of 4 doses; for vaginal dinoprostone (PTG-E2), 10 mg slow release for a maximum of 24 hours (every 12 hours was considered one dose). Oxytocin was administrated if there were identical conditions 2 hours after amniotomy, and there were less than 5 contractions per 10 minutes.
Concerning induction with PTG, misoprostol or dinoprostone were used according to presence of risk for hyperdynamia, loss of fetal wellbeing or uterine overdistention. Dinoprostone was used in all high-risk cases (intrauterine growth restriction,10 pregnancy-associated hypertension and oligohydramnios). Misoprostol was administered 25 mcg vaginally every 4 hours until favorable cervical conditions (BS ³7), with a maximum of 6 doses. Vaginal delivery system for dinoprostone was applied in the posterior vaginal fornix and cervical conditions were evaluated after 12 hours, with the possibility to wait until 24 hours. When favorable cervical conditions were reached and if active labor was not established, amniotomy was performed if feasible, or intravenous oxytocin was started. For both, a 30-minute CTG was performed before and 1 hour after PTG placement and every 4-6 hours in case of dinoprostone use. Active stage of labor was defined according to the World Health Organization (WHO) recommendations, when cervical dilation was at least 5 cm, concomitantly with regular contractions.11 Final BS and BS difference were recorded.
Perinatal outcomes recorded were time period to vaginal delivery, time period to delivery, epidural anesthesia, use of oxytocin, mode of delivery, cesarean-section (CS) indications, labor complications, and uterine hyperdynamia during CR. Our primary outcome was CS rate. Failure to progress was defined as same labor conditions once reached the active stage of labor and achieved regular contractions for at least 4 hours. Failed induction of labor was defined as the inability to achieve the active phase of labor after completed cervical ripening, amniotomy if technically possible, and 12 hours of oxytocin perfusion. Time to delivery was defined as time from initiation of IOL to delivery in hours. Uterine hyperdynamia included uterine tachysystole (more than 5 contractions in 10 minutes on at least two occasions, with or without fetal heart rate [FHR] changes) and uterine hypertonia (contraction lasting longer than 2 minutes with non-reassuring FHR changes). Labor complications recorded included intrapartum fever, uterine atony, placental abruption and postpartum endometritis (diagnosis performed >24 hours after delivery and up to six weeks postpartum). DBC specific complications obtained were voiding problems, vaginal bleeding, vasovagal response, decreased fetal movements, balloon displacement, fetal malposition, pain requiring partial emptying of the balloons, unintended amniotomy and non-reassuring FHR.
Neonatal outcomes recorded were gestational age at delivery, birth weight and birth weight percentile, Apgar score at 1 and 5 minutes, umbilical artery and vein pH, admission to neonatal intensive care unit (NICU), days at NICU and overall perinatal outcomes.
Data from the PTG group was analyzed without differentiating between misoprostol and dinoprostone. Although the DBC was the method of choice for all IOL, PTG type was chosen according to specific indications and IOL risk.
Data were analyzed using the IBM SPSS Statistics 26 statistical package. Variables studied were tested for normal distribution using the Kolmogorov‐Smirnov test. Comparisons between study groups were performed with Student’s t-test, χ2 or Fisher’s exact test where appropriate, and are presented as mean ± standard deviation (SD) or percentage (n). Kaplan-Meier analysis was used to evaluate time-to-delivery, in women with vaginal delivery. P‐values below 0.05 were considered statistically significant for all tests performed.
666 women were included in this study: 418 in DBC group and 248 in the PTG group (150 misoprostol and 98 dinoprostone).
Baseline characteristics of patients are shown in Table 1. The most common indications for IOL were prolonged pregnancy (≥41+3 weeks) and intrauterine growth restriction, which was significantly lower in the PTG group. Gestational age at induction was also significantly lower in the DBC group (DBC 39.7±1.7 vs PTG 40.1±1.6, p=0.004) with no differences in initial BS.
|
|
Double-balloon catheter (n=418) |
Prostaglandins (n=248) |
p-value |
|
Maternal age (years) |
33.7 ± 5.9 |
33.2 ±5.2 |
0.337 |
|
Maternal morbidity |
|||
|
Diabetes |
4.3 (18) |
4.4 (11) |
0.937 |
|
Hypertension |
3.6 (15) |
0.8 (2) |
0.028 |
|
Hypothyroidism |
9.1 (38) |
9.3 (23) |
0.937 |
|
Dyslipidemia |
0.2 (1) |
1.2 (3) |
0.117 |
|
Obesity |
2.9 (12) |
5.6 (14) |
0.074 |
|
Nulliparity |
67.2 (281) |
73.0 (181) |
0.119 |
|
Previous vaginal delivery |
32.3 (135) |
26.2 (65) |
0.098 |
|
Indication |
|||
|
Prolonged pregnancy |
34.4 (144) |
37.5 (93) |
0.427 |
|
Intrauterine growth restriction* |
22.0 (92) |
15.3 (38) |
0.035 |
|
Pregnancy-associated hypertension |
12.2 (51) |
13.3 (33) |
0.678 |
|
Diabetes mellitus |
6.7 (28) |
5.6 (14) |
0.589 |
|
Cholestasis of pregnancy |
8.4 (35) |
10.9 (27) |
0.28 |
|
Oligohydramnios |
0.7 (3) |
0.4 (1) |
0.991 |
|
Other |
15.6 (65) |
16.9 (42) |
0.638 |
|
Gestational age at induction (weeks) |
39.7 ±1.7 |
40.1 ±1.6 |
0.004 |
|
Initial Bishop Score |
2.8 ±1.4 |
2.8 ± 1.7 |
0.858 |
Table 1 Baseline characteristics of the studied population
Data shown as mean ± SD or %(n). p-values obtained by Student’s t test or Chi-squared test, where appropriate.
* Intrauterine growth restriction includes all fetuses with an ultrasound estimated weight below the 10th centile.
Labor outcomes are shown in Table 2. Final BS and BS differences were significantly lower in DBC group. There was no registered case of uterine hyperdynamia in the DBC group during CR, compared with 20 cases (8.1%) identified in the PTG cohort. A non-reassuring FHR was concomitant to hyperdynamia in 8 (3.2%) of cases and among them two ended in a CS during CR (one for persistent bradycardia due to placental abruption and the other for persistent non-reassuring FHR). In 46 cases (11%) the DBC was expelled spontaneously due to favorable cervical conditions. In the PTG group, mean doses of misoprostol or dinoprostone were 2.9±1.4 and 1.5±0.5, respectively. There were no statistically significant differences between groups regarding cesarean-section rate (DBC 27% vs PTG 27.8%, p=0.352) or failed IOL as cesarean indication (DBC 16.8% vs PTG 24.6%, p=0.199. However, there was a significantly higher CS rate for fetal distress in the PTG group (PTG 40.6% vs DBC 17.7%, p<0.001). Time to delivery was significantly shorter in the PTG group, as well as time to active labor. Concerning oxytocin infusion during labor, its usage was significantly higher in the DBC compared to PTG (60.0% vs 50.8%, p=0.02). In terms of maternal morbidity, there were no significant differences in labor complications. Kaplan-Meier analysis of time from induction to vaginal delivery is shown in Figure 1.
|
|
Double-balloon catheter (n=418) |
Prostaglandins (n=248) |
p-value |
|
Final Bishop score |
6.2 ± 2.4 |
7.0 ± 2.2 |
<0.001 |
|
Bishop score difference |
3.4 ± 2.3 |
4.3 ± 2.4 |
<0.001 |
|
Uterine hyperdynamia during CR |
0 (0) |
8.1 (20) |
<0.001 |
|
Time periods in vaginal deliveries (hours) |
|||
|
Time to 5 cm |
19.1 ± 7.5 |
14.4 ± 7.5 |
<0.001 |
|
Time to second stage of labor |
23.5 ± 8.2 |
16.7 ± 7.7 |
<0.001 |
|
Time to delivery |
25.2 ± 8.7 |
18.1 ± 8.3 |
<0.001 |
|
Time periods in all deliveries (hours) |
|||
|
Time to 5 cm |
19.6 ± 7.8 |
14.7 ± 7.5 |
<0.001 |
|
Time to second stage of labor |
23.7 ± 8.2 |
16.6 ± 7.6 |
<0.001 |
|
Time to delivery |
26.6 ± 9.3 |
19.1 ± 8.6 |
<0.001 |
|
Epidural anesthesia |
93.8 (392) |
94.8 (235) |
0.818 |
|
Oxytocin requirement |
60.0 (251) |
50.8 (126) |
0.02 |
|
Mode of delivery |
|||
|
Spontaneous vaginal delivery |
57.2 (239) |
52.4 (130) |
0.232 |
|
Cesarean-section |
27.0 (113) |
27.8 (69) |
0.825 |
|
Operative vaginal delivery |
15.8 (66) |
19.8 (49) |
0.19 |
|
Cesarean indication |
|||
|
Failure to progress |
47.8 (54) |
23.2 (16) |
<0.001 |
|
Fetal distress |
17.7 (20) |
40.6 (28) |
<0.001 |
|
Failed induction of labor |
16.8 (19) |
24.6 (17) |
0.199 |
|
Cephalopelvic disproportion |
10.6 (12) |
8.7 (6) |
0.673 |
|
Other |
7.1 (8) |
2.9 (2) |
0.23 |
|
Labor complications |
|||
|
None |
93.8 (392) |
96.4 (239) |
0.147 |
|
Intrapartum fever |
2.2 (9) |
0.4 (1) |
0.143 |
|
Uterine atony / bleeding (>1L) |
1.4 (6) |
1.2 (3) |
0.918 |
|
Placental abruption |
0.2 (1) |
0.8 (2) |
0.647 |
|
Postpartum endometritis |
0.5 (2) |
0.4 (1) |
0.647 |
|
Other† |
1.9 (8) |
0.8 (2) |
0.42 |
Table 2 Labor outcomes
Data shown as mean ± SD or %(n). p-values obtained by Student’s t test or Chi-squared test, where appropriate. CR, cervical ripening
† Other complications include retained placenta, vulvar or vaginal hematoma, surgical wound infection, postpartum urinary retention, cord prolapse and iliohypogastric nerve entrapment.
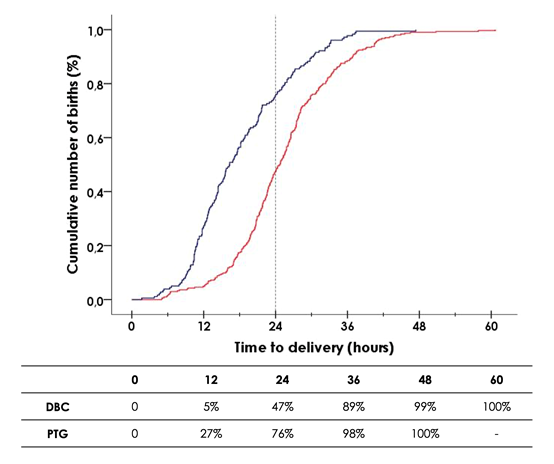
Figure 1 Kaplan Meier survival curve showing women who gave birth vaginally at time after initiation of cervical ripening, by double balloon catheter (DBC, red) or prostaglandins (PTG, blue).
Main neonatal outcomes are shown in Table 3. Gestational age at delivery, birth weight as well as its percentile were significantly lower in DBC compared with PTG. Umbilical artery and vein pH were significantly lower in the PTG group compared to the DBC group (7.24 vs 7.26, p=0.002, and 7.29 vs 7.32, p=0.001, respectively). Additionally, there was a higher rate of neonatal acidemia at birth (umbilical artery pH <7.10) in the PTG group (PTG 5.8% vs DBC 2.3%, p=0.043). Other neonatal outcomes were not statistically different, although days of admission were higher in the PTG group.
|
|
Double-balloon catheter (n=418) |
Prostaglandins (n=248) |
p-value |
|
GA at delivery (weeks) |
39.9 ± 1.7 |
40.2 ± 1.6 |
0.011 |
|
Birth weight (grams) |
3160 ± 549 |
3295 ± 536 |
0.002 |
|
Birth weight percentile |
39.3 ± 32.4 |
44.5 ± 31.6 |
0.04 |
|
Apgar <7 at 1 min |
4.3 (18) |
5.2 (13) |
0.579 |
|
Apgar <7 at 5 min |
0.7 (3) |
0.4 (1) |
0.612 |
|
Umbilical artery pH |
7.26 ± 0.08 |
7.24 ± 0.08 |
0.002 |
|
Umbilical vein pH |
7.32 ± 0.07 |
7.29 ± 0.08 |
0.001 |
|
Umbilical cord artery pH <7.05 |
1.3 (4) |
2.9 (5) |
0.211 |
|
Umbilical cord artery pH <7.10 |
2.3 (7) |
5.8 (10) |
0.043 |
|
Admission to NICU |
5.3 (22) |
4.0 (10) |
0.473 |
|
Days at NICU |
3.6 ± 4.3 |
6.3 ± 6.0 |
0.189 |
|
Overall neonatal outcomes |
|||
|
Normal |
94.7 (396) |
96.0 (238) |
0.473 |
|
Respiratory distress |
3.3 (14) |
3.6 (9) |
0.848 |
|
Perinatal deaths |
0 (0) |
0 (0) |
- |
|
Other |
1.9 (8) |
0.4 (1) |
0.198 |
Table 3 Neonatal outcomes
Data shown as mean ± SD or %(n). p-values obtained by Student’s t-test or Chi-squared test, where appropriate.
GA, gestational age; NICU, neonatal intensive care unit
Complications observed during CR with the DBC are described in Table 4. Pain or discomfort requiring partial emptying of the balloon (20 cc of each balloon) +/- oral paracetamol was the most frequent complication (3.8%), but CR continued without other incidences. One patient had voiding problems, which resolved emptying 20 cc from each balloon, allowing a normal urination after. Vaginal bleeding was observed in 4 cases, all of them mild and self-limited, and no additional management was required. 6 cases presented fetal malposition (transverse or breech) during IOL, so an external cephalic version was attempted in 3, successfully achieved in 2 patients, and followed by oxytocin infusion; however, none of these achieved vaginal delivery. Only 1 case of non-reassuring FHR was reported during CR with DBC, but it was an IOL indicated for non-reassuring CTG. In the PTG group no other complications except hyperdynamia presented during CR.
|
Complication |
% (n) |
|
None |
91.4 (382) |
|
Voiding problems |
0.2 (1) |
|
Vaginal bleeding |
1.0 (4) |
|
Vasovagal response during placement |
0.2 (1) |
|
Decreased fetal movements |
0.5 (2) |
|
Balloon displacement |
1.0 (4) |
|
Fetal malposition |
1.4 (6) |
|
Pain, discomfort requiring partial emptying of the balloons |
3.8 (16) |
|
Unintended amniotomy |
0.2 (1) |
|
Non-reassuring FHR |
0.2 (1) |
|
Data shown as %(n). FHR, fetal heart rate. |
|
Table 4 Double balloon catheter complications
Main findings
In this study we confirm effectiveness and safety of DBC as first line treatment for IOL with intact membranes, achieving vaginal delivery in 72% of women. We compared this approach with a historical cohort in which PTG were used as first choice, finding that DBC has a better safety profile, with significantly lower rate of hyperstimulation, loss of fetal wellbeing, and lower rates of umbilical artery pH<7.1. However, we also observed that the DBC has a longer time interval to delivery compared to the PTG group.
Our results regarding effectiveness of DBC and PTG, in terms of CS rate, are consistent with previously published studies. Beckmann et al. compared DBC IOL (n=347) to dinoprostone IOL (n=348) and reported CS rates of 32.6% vs 25.8%, respectively (p=0.240).12 Similar data were published by Løkkegaard et al. who randomly assigned 412 patients to DBC group and 413 patients to dinoprostone group, obtaining respectively a CS rate of 27.7% vs 25.9% (RR 1.07 [0.85–1.34]).13 A Cochrane systematic review focused on mechanical methods for IOL reported that CS rates were similar when comparing DBC vs vaginal PTG-E2, but may be increased when compared to vaginal misoprostol, with lower risks of uterine hyperstimulation with FHR changes with the balloon.8 Other systematic reviews and meta-analysis that compared DBC and PTG-E2 agree that both methods have similar effectiveness in terms of CS rate, but higher risks of uterine hyperstimulation and admission to NICU were found in the PTG-E2 group.14–16
Even initial BS was similar in both groups, there was a significantly different gestational age due the higher incidence of intrauterine growth restriction IOL indication in DBC group, which is normally induced before.
It should be highlighted that although the mode of delivery was similar, there was a higher improvement in BS after CR in the PTG group compared to the DBC group, as reported by Cromi et al.17
Another finding that is consistent with literature is that IOL takes longer with the DBC compared to PTG. This exceeding time related to balloon probes is also reported in several studies comparing Foley catheter with PTG1,18,19. In our study, we report a mean of 26.6 hours from the start of IOL to delivery in the DBC group, which is comparable to other published studies such as the one by Løkkegaard et al., which shows a time of 27.3 hours.13
Another relevant issue is the incidence of uterine hyperdynamia during CR. In our series it presented in 20 patients (8.1%), requiring use of tocolytics in 5; in contrast, there was no hyperdynamia during CR with DBC, and there are very few cases published.20 This advantage of mechanical methods makes the DBC a very safe CR method which may allow safe outpatient management, since it is not necessary to monitor fetal heart rate during CR, and may contribute to greater satisfaction in patients who desire to perform the first part of IOL at home.20,21
Oxytocin infusion was significantly more frequent in the DBC group, as shown in the PROBAAT-P or PROBAAT-M trials.16–19,22 This is probably due to the fact that mechanical methods promote cervical changes without causing primary uterine contractions, which also supports a decreased risk of uterine hyperstimulation.19
From our point of view, the greatest clinical advantage of DBC is its safety, derived from a low risk of hyperdynamia and fetal distress, at the expense of an increased time to delivery compared to PTG. However, this may not be a disadvantage in patients who can benefit from CR as outpatients, since they will spend less time in the hospital and this may lead to the impression that IOL has lasted less. Additionally, this shorter hospital stay in outpatient CR reduces the economic burden derived from an IOL.233 In our institution we introduced the DBC because of safety advantages mentioned and since it is considered to be the most physiological approach to initiate labor, which is a fact very appreciated by women and their families.24 To our knowledge, currently no guidelines recommend DBC as an initial elective method for IOL, and its use is limited to women with previous CS or cases at risk of hyperdynamia and fetal distress, such as intrauterine growth restriction.10,25
Regarding complications associated to DBC IOL, fetal malpresentation after catheter removal presented in 1.4% of patients, consistent with data reported by Salim et al.26 This is an adverse outcome related only to DBC, since no case of fetal malposition has been reported in the PTG group. We performed a subanalysis after this finding and realized that most of cases had a history of unstable presentation during the third trimester, an external cephalic version or polyhydramnios. This resulted in changes to our induction protocol and nowadays we exclude the use of DBC in these situations.
Strengths and limitations
The main strength of our study is a large number of consecutive patients in a single center, managed with a strict protocol of IOL that allows to establish well defined study groups in order to analyze differences with low bias. As main limitation, the PTG data is retrospective and therefore, these results should be interpreted cautiously, since the results of the DBC group are compared with an historical cohort.
To conclude, DBC has a similar effectiveness in terms of CS rate compared to PTG but with a better safety profile, a significantly lower rate of hyperstimulation and lower rates of umbilical artery pH<7.1. However, the use of DBC was associated with a longer time-to-delivery compared with the PTG group. Implementation of DBC as first choice in a real clinical setting is feasible and improves results in terms of safety. More studies are needed to evaluate patients’ perspectives and experiences regarding induction with DBC to better determine the best choice for IOL.
Mónica Cruz-Lemini is supported by Juan Rodés contract JR19/00047, Instituto de Salud Carlos III - Spanish Ministry of Health. This work was supported by the Primary Care Interventions to Prevent Maternal and Child Chronic Diseases of Perinatal and Developmental Origin Network (RICORS-SAMID) (RD21/0012), Instituto de Salud Carlos III, Madrid, Spain, and the Spanish Clinical Research and Clinical Trials Platform, SCReN (Spanish Clinical Research Network), funded by the ISCIII-General Subdirectorate for Evaluation and Promotion of Research, through project PT13/0002/0028, integrated in the 2013-2016 R + D + I State Plan and co-financed by and the European Regional Development Fund (FEDER). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
None.
Dr. Llurba reports receiving fees for lectures from Cook, while the remaining authors report no conflicts of interest.

©2023 Bailón-Queiruga, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.