eISSN: 2377-4304


Case Report Volume 9 Issue 1
1Resident, St. Lukes Medical Center QC, Philippines
2Consultant, Maternal Fetal Medicine, St. Lukes Medical Center QC, Philippines
Correspondence: Michelle L Malabanan MD, Resident, St. Lukes Medical Center QC, Philippines
Received: July 26, 2017 | Published: February 23, 2018
Citation: Malabanan ML, Zamora BB. Juvenile recurrent respiratory papillomatosis in pregnancy: a case report. Obstet Gynecol Int J. 2018;9(1):74-78. DOI: 10.15406/ogij.2018.09.00309
Juvenile-onset recurrent respiratory papillomatosis (JORRP) is a rare disease, usually acquired by vertical transmission upon vaginal delivery. Human Papilloma Virus (HPV) is the etiologic agent and the most common types involved are 6 and 11 that are the same types associated with anogenital condylomas. It is associated with low mortality but with significant morbidity. Pregnancy was related with accelerated papilloma growth in RRP, while RRP may have an effect on the outcome of pregnancy due to chronic maternal hypoxemia. We present a case of Juvenile onset recurrent respiratory papilloma in pregnancy seen starting 7 weeks age of gestation. The effect of pregnancy on JORRP, its effect on pregnancy, and the latest modalities in treatment including the role of HPV vaccination are discussed in the article with the review of literature.
Keywords: recurrent respiratory papillomatosis, pregnancy, human papilloma virus
Recurrent respiratory papillomatosis (RRP) is a rare disease of the larynx, prevalence of which is 1.11 per 100,000 in the western world.1 However; there are no studies that show any incidence of RRP in Asia upon searching PUBMED, OVID, and GOOGLE SCHOLAR. It is viral in etiology specifically with human papilloma viruses (HPV) -6 or -11. It is associated with significant morbidity and on occasion mortality. These HPV types are associated with anogenital condylomas and are considered at low risk for malignant transformation.3
There are two forms described, an adult onset (AORRP) and the more aggressive juvenile onset (JORRP). Patients typically presents with hoarseness or difficulty of breathing. The burden of RRP is so much in that patient usually undergoes 2-5 surgeries a year, and mostly requiring tracheostomy.3 It causes intense physical, psychological, and financial strain on patients and their families.4 In the United States, a study was done last 2000 to assess the medical costs and the number of quality-adjusted life years lost in JORRP. The annual cost is between $40 million and $123 million depending on the prevalence.5
There are only three case reports published on Recurrent Respiratory Papillomatosis in pregnancy worldwide. All cases were an emergency case where in they presented with obstructive airway. One of the cases published had fatal maternal outcome at 20 weeks age of gestation. In these case reports, they claim that pregnancy is associated with accelerated papilloma growth with reactivation of latent disease. The altered immune system and hormonal status during pregnancy are some theories explored.6 Not only does pregnancy affect RRP but also the other way around. RRP is associated with chronic hypoxemia hence may affect pregnancy outcome. There are reports that chronic hypoxic environment may cause significantly reduced birth weight.7
There is no absolute cure for RRP; however, surgical debulking is the treatment of choice to quickly ameliorate symptoms. There are current adjuvant therapies that may help decrease papilloma growth such as cidofovir, indole-3-carbinol, ribavirin, mumps vaccine, and photodynamic therapy.8 Recent studies also show the role of tetravalent HPV vaccine (Gardasil) in RRP. Reports says that it induces neutralizing antibodies against capsid antigens that may help stabilize the disease in aggressive forms.9
We present a case of Juvenile Onsent Recurrent Respiratory Papillomatosis in Pregnancy seen at 7 weeks age of gestation. This article presents the course of the disease in pregnancy, its effect on pregnancy outcome, the current modalities of treatment and the role of HPV vaccine.
The case
O.K. is a 27 year old Gravida 2 Para 1 with an obstetric score of 1-0-0-1 came in for labor pains at 36-37 weeks age of gestation. She is a diagnosed case of recurrent laryngeal papillomatosis since 3 years of age presenting as sudden loss of voice. She is non-hypertensive, non-diabetic, with no history of thyroid problems or other diseases. No other family members affected with the disease. No family history of hypertension, diabetes, thyroid diseases or cancers. She is non-smoker, non-alcoholic beverage drinker, and no illicit drug use. She is the eldest of three siblings delivered to a 17-year-old mother by normal spontaneous delivery. Mother denies presence of any genital lesions upon delivery of the patient, with unknown HPV status. Parents were said to be monogamous. She is regularly menstruating every 28-30 days, menarche at 13 years of age, subsequent menses were occurring for 4 days amounting to 2 pads per day with accompanying dysmenorrhea. Coitarche is at 18 years of age with only one sexual partner. Her previous pregnancy was carried to term last 2008, by normal spontaneous delivery to a newborn female weighing 2400g without any fetomaternal complications. During her first pregnancy patient underwent only one laser excision at 12-14 weeks.
Patient was diagnosed with recurrent laryngeal papillomatosis when she was brought to Philippine General Hospital (PGH) due to sudden loss of voice. There she underwent larnygoscopy and biopsy of laryngeal mass, which revealed papilloma. At 4 years of age, she underwent her first operation at PGH where they did only scraping of the laryngeal mass due to lack of facilities. She had nine operations then, and was already diagnosed with recurrent laryngeal papillomatosis. She underwent emergency tracheostomy when she suddenly presented at the emergency room with obstructive dyspnea. She was then referred to a charity association where she was then brought to Canada to undergo series of examinations and operation. She then underwent her first laser excision there and subsequent operations with a total eleven excisions. Her tracheostomy was removed there however after the contract was over with the sponsoring charity, patient was then brought home to the Philippines. Follow up was done with other institution from 2000-2005. There she underwent a total of 18 laser excision. Last 2005, patient again consulted at emergency department due to sudden onset of dyspnea where a tracheostomy was again done at Makati Medical Center. In year 2006, patient was then eventually referred to our institution due to financial constraint. She is already known to ENT (Ears, Nose, and Throat) service, underwent mumps vaccine intralesional injection last 2008 and is on quarterly follow up. She usually undergoes 3-5 procedures a year and as of to date, a total of 83 excision was done last of which was January 21, 2015 at her 12th week of pregnancy.
Last September 2014, patient noted missed menstruation with occasional nausea, however no associated vomiting. Pregnancy test was then done which tested positive. Patient was then referred to our service and came in for her first prenatal consult at 7 weeks age of gestation. Routine diagnostics and examinations were done. During her first visit, patient complaints of occasional dyspnea, vital signs were stable with clear breath sounds; pulse oximetry was at 98-99%. On speculum examination, vagina is smooth with no lesions, cervix is pink, smooth with no lesions, discharge or bleeding. Internal Examination revealed: vagina admits 2 fingers with ease, the cervix is smooth, soft, and parous, and uterus is not enlarged. Pap smear was done which showed non-specific inflammation. Patient was then referred back to ENT for clearance and closes monitoring as well as to Perinatology service and was seen at 12 weeks age of gestation. At this time, patient complaints of increasing episodes of dyspnea, upon examination of ENT service, there was note of papillomatous lesion completely obliterating the airway at the level of the glottis. A conference was done with the perinatology service, ENT, and anesthesia for the planning of the patient’s procedure and as well as for the monitoring of the pregnancy. At the conference, it was decided that patient should undergo tracheobronchoscopy and direct laryngoscopy with excision of the papilloma as soon as possible for prolongation of this state of hypoxemia may cause danger not only to the mother but also to the unborn child. During the conference, other concerns brought up included the monitoring of the progression of the disease since RRP in pregnancy was associated with increased recurrence, the possibility of growth restriction, the risk for recurrent upper respiratory tract infection, the plans for delivery and the anesthesia to be used. The consensus was to closely monitor the growth of papilloma by the ENT service, monitor the growth of the fetus by serial ultrasound and that mode of delivery is still vaginal unless there is an obstetric indication to deliver abdominally. Patient was then admitted, co-managed with our service and underwent tracheobronchoscopy and direct laryngoscopy with microlaryngeal excision of laryngeal papillomatosis under general anesthesia. Intraoperatively, there was note of scarring at the area of the anterior commissure and papillomatous lesion completely obliterating the airway at the level of the glottis (Figure 1). The mass was noted to extend inferiorly before the endotracheal tube level. Biopsy was done which showed squamous papilloma, non-keratinizing. No intraoperative complications were noted and she tolerated the procedure well. There was no note of any hypogastric pain or vaginal bleeding. However, early morning the following day, she experienced difficulty breathing with oxygen saturation of 97%. Suctioning was done, the connect laser flex tube was removed and the tracheostomy button replaced. Her difficulty of breathing resolved and her oxygen saturation increased to 100%. She became comfortable and her distress resolved thereafter. Later in the day there were no episodes of dyspnea, cyanosis, hemoptysis, vomiting, coughs or chest pain. Patient was then discharged improved.
After the procedure, patient continued her regular follow up with our service, with improvement of symptoms. Patient was noted to be more comfortable at this time. At 23-24 weeks, congenital anomaly scan was done which revealed normal results. At 25-26 weeks age of gestation, an oral glucose tolerance test was done which revealed normal results too. Serial ultrasound every 2-3 weeks was done to assess for any fetal growth restriction caused by her condition (Table 1). Tracheoscopy by ENT service was done and showed papillomatous lesion at glottis and plan is for excision of mass post-partum if with no recurrence (Figure 2). At 30 weeks, plan of perinatology is serial ultrasound every 2-3 weeks was done to assess fetal growth restriction as a possible complication of her condition. There was note of decrease in fetal growth from 50-75th percentile to 25th-50th (Table 1). At 33 weeks, patient complains of occasional hypogastric pains and perceived contractions on prenatal check up, Non-stress test was done: reactive, with baseline fetal heart rate of 130s moderate variability with acceleration no decelerations, good fetal movements with no uterine contractions. Patient was given Nifedipine 10 mg/tab every 8 hours for 3 days and advised follow up after 1 week and was already advised fetal surveillance once weekly by non-stress test. On her 34th week, there were already no complaint of hypogastric pain, any perceived contractions and vaginal bleeding. However, seen at the IE room for cough and colds. On examination, stable vital signs, afebrile, oxygen saturation at 99%, with note of nasal congestion and post-nasal drip. Breath sounds were clear, with adynamic precordium. Assessment is upper respiratory tract infection, probably viral. ENT service was informed; patient was given butamirate citrate for the cough and salinase spray for nasal congestion. Advised increase oral fluid intake and Vitamin C and was sent home.
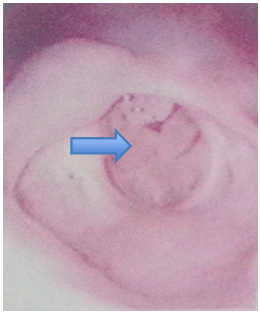
Figure 1 Laryngoscopic view shows glottic papilloma (blue arrow) caused by recurrent respiratory papillomatosis prior to excision.
|
|
May 14, 2015 |
June 2, 2015 |
June 23, 2015 |
|
EFW |
1089 grams,+/-159 grams |
1517grams +/-228grams |
1730 grams,+/-253 grams |
|
Percentile |
50th – 75th |
50th -75th |
25th-50th |
|
Weight gain |
-- |
428g |
213g
|
Table 1 Table of patient’s estimated fetal weight monitoring
Recurrent respiratory papillomatosis (RRP) is a rare disease of the larynx caused by infection with human papillomaviruses (HPV) -6 or -11, associated with significant morbidity and on occasion mortality.10 Its true incidence and prevalence is uncertain. Numerous studies have been performed to elucidate this. Recently, Campisi etal. Created a national database incorporating all children (less than 14 years old) with RRP in Canada treated by Pediatric Otolaryngologists. This study found the national incidence of JORRP from 1994 to 2007 to be 0.24 per 100 000 with a prevalence of 1.11 per 100 000.1
It is characterized by exophytic; wart-like lesions of the upper airway that tend to recur and have the potential to spread throughout the respiratory tract. Sir Morrell Mackenzie (1837–1892) was the first to recognize papillomas as a lesion of the laryngo-pharyngeal system in children in the late 1800s. It was not until the advent of modern molecular genetic techniques in the 1990s that HPV was confirmed as the causative agent of RRP.3
Approximately 100 types of human papillomavirus infection (HPV) have been identified, at least 40 of which can infect the genital area. Most infections are self-limited and are asymptomatic, others, unrecognized. Most sexually active persons become infected with HPV at least once in their lifetime. Oncogenic, high-risk HPV infection (e.g., HPV types 16 and 18) causes most genito-anal, and oropharyngeal cancers and precancers, whereas non-oncogenic, low-risk HPV infection (e.g., HPV types 6 and 11) causes genital warts and recurrent respiratory papillomatosis.2
Recurrent respiratory papillomatosis is categorized into juvenile onset (JORRP) and adult onset (AORRP) based on diagnosis before or after 12 years of age, respectively. Studies have shown that there is no sex predilection, however in AORRP, there is slight male predilection. The majority of JORRP patients (75%) have been diagnosed by 5 years of age.5 Children who are diagnosed at a younger age was said to have a higher risk for disease progression compared with children diagnosed later in life. Patients typically present with symptoms of hoarseness or respiratory obstruction in childhood or adolescence. In the majority of cases, the papillomas are confined to the larynx; only 5% of patients exhibit more distal involvement of the trachea, and involvement of lung parenchyma occurs in less than 1% of cases.5 As in our patient, she was diagnosed with RRP at age of 3 presenting with sudden loss of voice. And as previously mentioned, patients presenting at an early age exhibit a more aggressive course compared to those diagnosed later, hence, we could see the aggressiveness of the disease in our patient where she experiences 3-5 excisions a year and a total of 2 tracheostomy. She also now has a distal involvement of the trachea.
Retrospective and recent prospective studies have confirmed that HPV may be passed by vertical transmission from mother to child. The virus is thought to gain entry to its host cell, the basal keratinocyte, by micro traumas or abrasions to the surface epithelium. Mounts demonstrate that a maternal history of genital warts in pregnancy was identified as the principal risk factor for the development of JORRP. Silverberg et al.11 showed that children born to mothers with active condylomata had a 231-fold increased risk of developing RRP when compared with children born to disease- free mothers. In addition, they showed that children born to women with active condylomata had a twofold higher risk of developing RRP if labor lasted more than 10 hours.11 Kashima also found that childhood-onset RRP patients were more likely to be first born and vaginally delivered than were control patients of similar age. The authors hypothesized that primagravid mothers are more likely to have a long second stage of labor and that the prolonged exposure to HPV in the birth canal leads to a higher risk of infection in the first-born child. They also suggested that newly acquired genital HPV lesions are more likely to shed virus than long-standing lesions. This would explain the higher incidence of RRP observed among the offspring of young mothers of low socioeconomic status – the same group that is more likely to acquire sexually transmitted infections such as HPV. Hallden and Majmudar showed that 54% of JORPP patients were born to mothers with a history of vulvar condylomata at the time of delivery.3 As in our case, patient is the first born, delivered by normal spontaneous delivery to a 17 year y old mother: the triad of risk factors for JORRP. However, there was no evidence of HPV infection of the mother at that time of delivery, for she denies any lesions seen or palpated.
Reports of neonatal papillomatosis suggest that, in at least some cases, development of the disease may occur in utero. As cesarean section does not seem to prevent the development of RRP in all cases, a better understanding of the risk factors associated with RRP is needed before the efficacy of caesarean delivery in preventing papilloma disease can be fully assessed.3
While most JORRP is acquired by vertically, there are few reports on its transmission. A study made by Gerein et al.12 showed that children and partners of patients with recurrent respiratory papillomatosis have no evidence of the disease during long-term observation.12
JORRP is frequently misdiagnosed as Laryngotracheobronchitis, Asthma, Laryngomalacia or foreign body in the throat initially. While a diagnosis can be suspected from the clinical presentation, it needs to be confirmed radiologically, and histopathologically. Microlaryngoscopy and histopathological examination of the papillomata are common means of achieving this.4 First examination usually is an indirect laryngoscopy, which reveals warts-like masses obstructing the larynx. They are seen as sessile or pedunculated masses, pink to white in color, in irregular exophytic clusters. A direct laryngoscopy is then performed in the operating room under general anesthesia and a biopsy is taken. Diagnosis of HPV can be made using polymerase chain reaction (PCR), dot blot hybridation, immunohistochemistry and in situ hybridation. Detection of HPV mRNA of the E6 and E7 transforming genes is a new method of diagnosis, seems to be 100% sensitive.13 In the case of our patient, she presented with sudden loss of voice, a laryngoscopy with biopsy was first done to establish her diagnosis. However, there is still limited use of PCR or immunochemistry in our country. Newer studies also have offered HPV DNA testing to test what HPV DNA type is present in order to predict the course of the disease, or its malignant potential.
On histopathology, papillomatous lesions of RRP is said to preferentially occur anatomically at the sites of “transformation zones”, where squamous epithelia abut ciliated columnar epithelia but can infect anywhere in the respiratory tract.8 The classical sites for recurrent disease in the upper aero-digestive tract would be the nasopharyngeal area of the soft palate, limen vestibuli, midzone of laryngeal area of the epiglottis, upper and lower margins of the ventricle, vocal fold undersurface, carina and bronchial spurs. It is interesting to note that papillomata have been observed at tracheotomy sites and tracts where the iatrogenic induction of change of epithelialization also occurs.10 Histologically, maybe seen as finger-like projections of nonkeratinized stratified squamous epithelium supported a core of highly vascularized connective tissue stroma its basal layer maybe normal or hyperplastic.
The malignant transformation rate of RRP has ranged from 1% to 23%. Severel factors have been associated with increase cancer risk, which include irradiation therapy, laryngopharyngeal reflux, smoking, and exposure to other carcinogens. In RRP, dysplasia is common and to detect those laryngeal papillomas progressing from dysplasia into invasive carcinoma, repeated biopsy must be done.
Literatures say that pregnancy is known to worsen condyloma acuminatum; hence pregnancy may also be a significant risk factor for exacerbation of established RRP. On a case report made by Scurry, they propose that the hormone-altering state of pregnancy is the likely the etiologic factor in the apparent accelerated growth of RRP during gestation. They presented a case of 25 year old on her 14th week of pregnancy who came in for dyspnea and voice changes. In her intitial presentation at 14 weeks’ gestation and her laryngoscopy at 35weeks’gestation, her RRP had rapidly progressed again to nearly complete laryngeal obstruction. At 2 months postpartum, the patient’s RRP seemed to have slowed. Hence, the recurrence of the papillomas may really be affected by pregnancy. However, that is not the case in our patient. She had her previous excision last November 2014, during her conception and repeated at 12 weeks age of gestation. As of today, there was recurrence of laryngeal papillomas however; there is still no need for excision.
So, how does pregnancy increase recurrence of RRP? The role of estrogen on the growth of RRP has been conjectured, since it has been discovered that RRP exhibits increased binding of estrogen.6 It has been described that indole-3-carbinol (I-3-C), a compound that is found in high concentration in cruciferous vegetables such as cabbage, cauliflower, and broccoli, has been shown to inhibit estrogen metabolism and reduce papilloma growth. Specifically, in one study I-3-C reduced the formation of HPV-induced papilloma tumors in immunocompromised mice by nearly 75%.8 In a phase I trial of the use of I-3-C for the treatment of RRP, the clinical response to I-3-C in children with RRP was closely correlated with the ratio of hydroxylated estradiol in urine.6 From these studies, it seems that RRP is responsive to estrogen concentrations. It is known that estrogen levels rise significantly during pregnancy. Therefore, the increased estrogen levels during pregnancy could explain any accelerated growth of RRP during the gestational period.
There is no specific report on effects of RRP in pregnancy for there are only few cases seen. However, RRP is associated with hypoxia and there are reports that chronic hypoxic environment may cause significantly reduced birth weight. The role of oxygen in fetal growth is underscored by observations that IUGR is seen frequently in pregnancies complicated by decreased maternal oxygen-carrying capacity as well as localized hypoxia due to poor uterine perfusion.7 The role of oxygen in fetal growth is further underscored by observations of significant fetal growth restriction and increased fetal and neonatal morbidity and mortality in pregnancies accompanied by fetal anemia and hypoxia.7 In the current study, by Huang etal, they have found that chronic, but not acute, exposure to hypoxia results in significant fetal growth restriction, consistent with clinical observations in humans and models of in utero hypoxia and uterine artery ligation. In addition, chronic hypoxic stress results in decreased litter size and pregnancy failure.7 Hence, pregnant patients with RRP are prone to have growth-restricted neonates. Fortunately, in our case there were no associated fetal complications during her first pregnancy, however, during this second had preterm birth. There is no evidence or theories reported that RRP is associated with preterm delivery.
Management of recurrent respiratory papillomatosis is still a mystery. The disease course of JORRP is highly variable but typically requires extensive medical and surgical treatment. On average, patients undergo 5 surgeries per year and more than 20 in their lifetime. Juvenile-onset recurrent respiratory papillomatosis also causes intense physical, psychological, and financial strain on patients and their families.4
Many treatment modalities for RRP have been tried; some of them more efficacious than others, but none of them have been proven fully efficacious for a cure in all patients. Surgical debulking is currently the treatment of choice for RRP. Newer surgical approaches utilizing microdebriders are replacing laser ablation.10 Surgical excision aims to secure an adequate airway and improve and maintain an acceptable quality of voice. Various lasers such as CO2, KTP, and pulsed dye were found to be the preferred method of surgical removal of RRP in children.8 In our patient, tracheobronchoscopy and direct laryngoscopy with microlaryngeal excision of laryngeal papillomatosis was done. ENT monitored patient every month with tracheoscopy to check for any recurrence of papillomas.
Aside from surgery, others use adjuvant therapy for certain cases. The current criteria for adjuvant therapy are the necessity for more than 4 surgical procedures annually, rapid regrowth of papillomata with airway compromise and/or remote multisite spread of the disease.9 Adjuvant treatments currently used include cidofovir, indole-3-carbinol, ribavirin, mumps vaccine, and photodynamic therapy.8
Cidofovir is the gold standard in the adjuvant therapy in RRP. It is a cytosine nucleotide analogue with antiviral activity for the treatment of cytomegalovirus (CMV)-retinitis in persons with acquired immunodeficiency syndrome. The recently developed tetravalent HPV vaccine Gardasil induces neutralizing antibodies against capsid antigens.9 It has been shown that the expression of papilloma virus L1 genes in vitro induces high titers of virus neutralizing serum antibodies when administered as an immunogen. There are some case reports describing a stabilization of the disease in the very aggressive forms, which is promising but further studies must be done.9 Our patient underwent mumps vaccine intralesional injection last 2008, with note of decrease recurrence of the papilloma. Post-partum, plan is to still closely monitor patient for there is still altered hormonal status at this time. One of the 3 cases of RRP in pregnancy had her obstructive symptoms developed day 2 postpartum.14 HPV vaccination is still being discussed with the patient and ENT service. Breastfeeding is still highly encouraged for there are no contraindications.
RRP is a rare disease that causes significant morbidity. It is transmitted vertically from the infected mother to her fetus. However, there are reported cases of neonatal papillomatosis that may indicate that it is not always the case and other routes should be explored. Hence, indication for cesarean section in patients with HPV infected mothers for prevention of RRP is still a controversy. HPV-induced papilloma growth accelerates in the presence of increased estrogen concentrations; hence, we should always advise that all women known to have RRP should be warned of the possibility of the worsening of their airway disease during pregnancy. Even if this not always the case as seen in our patient, multidisciplinary management with other services is vital and close monitoring by their otolaryngologist and perinatologist is advised.
There is no acknowledgement.
Authors declare there is no conflict of interest.

©2018 Malabanan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.