eISSN: 2377-4304


Case Report Volume 9 Issue 1
1Division of Obstetrics and Gynecology, Pontificia Universidad Catolica de Chile, Chile
2Department of Obstetrics and Gynecology, Center for Research and Innovation in Maternal-Fetal Medicine (CIMAF), Chile
3Division of Surgery, Hospital Sotero del Rio, Chile
4Department of Radiology, Hospital S?tero del R
Correspondence: Paula Vargas, Designation Center for Research and Innovation in Maternal-Fetal Medicine (CIMAF), Department of Obstetrics and Gynecology, Hospital Stero del Ro, Santiago, Av. Concha y Toro 3459, Chile, Tel 56991581927
Received: October 05, 2017 | Published: January 9, 2018
Citation: Silva P,Vargas P, Munoz A, et al. Expectant management of an abdominal pregnancy diagnosed at 18 weeks: a case report. Obstet Gynecol Int J. 2018;9(1):13-16. DOI: 10.15406/ogij.2018.09.00295
A 36 years-old, G2P2 patient presented at 18+2 weeks of gestation with abdominal pain and vomiting. A transabdominal ultrasound at admission showed a single live fetus according to gestational age, while a transvaginal sonographic examination revealed a normal uterus without an intrauterine gestation. Due to the suspicion of an abdominal pregnancy, the patient was admitted for further study. A magnetic resonance imaging confirms an extrauterine abdominal pregnancy and established placental implantation, blood supply and abdominal organs compromise. Together with the patient and a multidisciplinary team, an expectant management was decided. Serial ultrasound assessments were performed to evaluate fetal condition, as well as serial MRI to exclude any intra-abdominal organ compromise. A laparotomy was performed for fetal extraction at 34 weeks of gestation without complications, leaving the placenta in situ. The patient and newborn had a successful postnatal evolution. This report provides evidence that the expectant management of an abdominal pregnancy diagnosed early in pregnancy is feasible.
Keywords: Abdominal pregnancy, Ectopic pregnancy, Advanced extrauterine pregnancy, Expectant management
The prevalence of an ectopic pregnancy is 1-2%, with approximately 95% of them located in the Fallopian tubes.1 An abdominal pregnancy is a very rare form of ectopic pregnancy, which is located in the peritoneal cavity.2 The estimated incidence of an abdominal pregnancy is around 1:10.000, representing approximately 1, 4% of all ectopic pregnancies.3-5 Potential implantation sites include the uterine serosa, omentum, pelvic wall, broad ligament, posterior cul-de-sac, abdominal organs (i.e spleen, bowel, liver), pelvic vessels, and diaphragm.6-8 Given its different forms of clinical presentation, a high index of suspicion is needed to make the diagnosis. Its clinical symptoms include persistent abdominal pain, nausea, vomiting, painful fetal movements, weight loss, vaginal bleeding, and palpation of an abdominal mass distinct from the uterus.9-12 Here, we report a successful expectant management of an abdominal pregnancy diagnosed at 18 weeks of gestation.
A 36 years-old Hispanic women, G2P2 with two previous term deliveries (two cesarean deliveries), non-sensitized Rh-negative, was admitted at 18+2 weeks of gestation due to abdominal pain and vomiting. On physical exam, a soft abdomen and stable vital signs were found. A transabdominal ultrasound at admission showed a single live fetus according to gestational age, while a transvaginal sonographic examination revealed a normal uterus without an intrauterine gestation, and a small amount of free fluid. Due to the suspicion of an abdominal pregnancy, the patient was admitted to our High Risk Pregnancy Unit for further evaluation. A magnetic resonance imaging (MRI) was performed and confirmed an extrauterine intraperitoneal gestational sac located in the maternal right flank with a single live fetus inside. The placenta impressed bilobar, located on small bowel, colon, cecum, and part of the mesentery. Computer tomography angiography showed placental blood supply from the right adnexal plexus depending on the hypogastric artery of that side, excluding involvement of great vessels. The case was discussed with the patient and a multidisciplinary team. Since the patient requested an expectant management, she was kept admitted in order to perform serial assessment of the maternal and fetal condition, as well as MRIs for further anatomic assessment, including potential placental invasion of intra-abdominal organs (Figure 1). A double J stent was installed due to right hydroureteronephrosis, and anti-D inmunoglobulin (300 mcg) was administered at 28 weeks of gestation. Antenatal corticosteroids were administered at 24 weeks of gestation and repeated just before the cesarean section. Delivery was planned at 34 weeks on maternal request due to maternal discomfort. A supraumbilical laparotomy was performed for fetal extraction, and the intraoperative findings revealed an intra-abdominal amniotic sac surrounded by extensive vascular areas with a small a vascular window by which fetal extraction was performed (Figure 2). A female newborn was obtained weighing 2187grs, with an Agar score of 5/8. The placenta was left in situ. The patient has had a successful postoperative first week without any complications. CT scan was performed to evaluate postoperative findings (Figure 3). Human chorionic gonadotropin levels dropped from 115.592 mUI/mL to 40.840 mUI/mL during postoperative first week. The need to administer methotrexate was discussed with the Gynecology Oncologist specialists and decided just to follow up with serial images. Patient was discharged at 13th day.
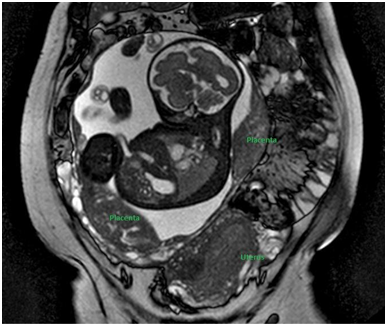
Figure 1 MRI at 28 weeks showed an extrauterine intraperitoneal gestational sac located in the maternal right flank with a single live fetus inside. The placenta impressed bilobar, located on small bowel, colon, cecum, and part of the mesentery.
The baby was admitted to Neonatal Intensive Care Unit (NICU) for further observation due to gestational age. During the fifth day in NICU, the newborn developed a necrotizing enterocolitis, with good response to medical treatment and no surgical intervention was required. At second week, the baby was discharged to Intermediate Care Unit.
Abdominal pregnancy is a very rare entity, representing approximately only 1% of all ectopic pregnancies. Main risk factors for this condition include tubal damage, pelvic inflammatory disease, endometriosis, assisted reproduction techniques and multiparity. The theories proposed for its etiology are:
Because clinical signs and symptoms are non-specific, high index of suspicion is needed to make the diagnosis. In a retrospective study, only 45% of the abdominal pregnancies were diagnosed preoperatively.15 The most frequent localizations reported were pouches surrounding uterus, uterine fundus and adnexa, based on a review of abdominal pregnancies diagnosed before 20 weeks.16 It is believed that implantation site and blood supply available are key factors to allow the possibility of fetal survival.17,18 Ultrasound is the most used diagnostic tool in obstetric practice; nevertheless, it is limited by many factors including maternal obesity, meteorism and operator ability. Despite advances in obstetric ultrasound diagnosis, MRI is a very useful tool to identify placental implantation site, blood supply, and its relationship with great vessels, bowel or other vital structures that could be affected.19-21
Fetal survival is exceptional, since the perinatal mortality reported is as high as 80-90%.22 While some authors consider that it is possible an expectant management and wait until fetal lung maturity, others propose that there is a high risk for a life-threatening hemorrhage.23,24 In this case, the expectant management until 34 weeks was decided together with a multidisciplinary team without any maternal complication during pregnancy. However, the optimal treatment of an abdominal pregnancy is unknown. Because abdominal pregnancies frequently implant in organs or vascular structures, one of the major issues in delivering an abdominal pregnancy will be hemorrhage control and placental management after delivery. In a review of 225 case reports, mean blood loss was 1450 mL (range 50-7500 mL) and 25% of women required blood transfusion.16 Among the options available for preoperative preparation are arterial embolization, ureteral catheters insertion, bowel preparation, blood bank assistance for massive transfusion protocols, and a multidisciplinary surgical team available.20,25
There is a debate in the literature regarding management and removal of the placenta. Placental removal can be associated to a massive bleeding, and efforts to control the bleeding may lead to organ damage.26,27 Leaving the placenta in situ may lead to secondary hemorrhage, abscess formation, adhesions, necrosis, coagulopathy, and need for a second surgical intervention.28,29 The partial and complete removal of the placenta have been reported with successful outcome,30,31 however, if removal of the placenta is not possible due massive vascular invasion, it is recommended to leave the placenta in situ and maintain a close follow-up for involution and early identification of potential complications. Thus, placental management must be individualized and assessed at the operating room, removing it only if it is safe to do.32-34 Use of postoperative methotrexate has been described in cases with placenta left in situ, although some authors have proposed that rapid placental destruction leads to accumulation of necrotic debris, favoring bacterial growth.20 Rahman et al.35 reported five patients treated postoperatively with methotrexate. Although they had rapid decline of urinary gonadotropin concentrations, all cases developed intra-abdominal infection and two died. Other authors suggest that it could be used at lower doses and with less frequency to prevent fast placental destruction and accumulation of necrotic tissue in excess.36
Here, we present a rare case of an abdominal pregnancy diagnosed at 18 weeks of gestation, followed during pregnancy with expectant management and a favorable maternal and fetal outcome. Serial assessment with MRI allowed us to define placental implantation and vascular involvement preoperatively and also to prepare a multidisciplinary team by the time of surgery. Intraoperatively, an amniotic sac surrounded by significant vascularization was found, and bleeding from the amnioplacental interface was successfully controlled, leaving the placenta in situ.
We would also like to thank to all surgical team from Hospital Sotero del Rio, Santiago, Chile for their support and help for making possible this surgery.
The authors declare that there is no conflict of interest regarding the publication of this article.

©2018 Silva, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.