eISSN: 2377-4304


Research Article Volume 9 Issue 1
1Department of Obstetrics and Gynecology, Massachusetts General Hospital, Boston, MA 02114, USA
2Tufts University School of Medicine, 145 Harrison Ave, Boston, MA 02111, USA
Correspondence: John C Petrozza, Chief, Vincent Reproductive Medicine & IVF, Massachusetts General Hospital and Harvard Medical School, 55 Fruit Street, Yawkey 10A, Boston MA, 02114-2696, USA, Tel 16177266562
Received: September 26, 2017 | Published: January 3, 2018
Citation: Sacha CR, Papageorge M, Souter I, et al. Transvaginal ethanol sclerosis versus saline aspiration of endometriomas prior to ivf: a randomized controlled trial. Obstet Gynecol Int J. 2018;9(1):1-5. DOI: 10.15406/ogij.2018.09.00293
Objective: Evaluate whether transvaginal aspiration of endometriomas with saline or ethanol sclerosis improves ovarian response and IVF outcomes.
Design: This was a randomized controlled trial of 22 women undergoing IVF at a university-affiliated infertility clinic, 1998-2002. Subjects, aged 18-42 with body mass index (BMI, kg/m2) less than 40 and adequate ovarian reserve, had undergone laparoscopic cystectomy for an endometrioma within 12 months followed by an unsuccessful IVF cycle with recurrence on imaging. Ten subjects were randomized to cyst aspiration with saline (control) and 12 to 95% ethanol, followed by another IVF cycle. The main outcomes were ovarian response and IVF outcomes pre- and post-endometrioma aspiration.
Results: There was a higher median peak estradiol level post-aspiration (2598 pg/ml vs. 2107pg/ml, p = 0.04) and a greater increase in the median number of oocytes retrieved during the post-aspiration IVF cycle compared to the pre-aspiration cycle (3 vs. 2, p = 0.04) in the ethanol versus saline group.
Conclusion: Ethanol sclerosis leads to a higher peak estradiol level and a greater increase in the number of oocytes retrieved from initial to post-aspiration IVF cycle compared to saline. In women with recurrent endometriomas attempting IVF, ethanol sclerosis is a minimally invasive alternative to surgery.
Keywords: Endometrioma, Aspiration, Ethanol sclerosis, In-vitro fertilization
IVF, In-Vitro Fertilization; FSH, Follicular Stimulating Hormone; REI, Reproductive Endocrinology and Infertility; AFC, Antral Follicle Count; AMH, Anti-Mullerian Hormone; SAS, Statistical Analysis System
Endometriosis affects 6-10% of reproductive age women and is detected in 21-47% of women with infertility1,2 Notably, it is also present in 20-40% of women undergoing IVF and is often associated with lower rates of live births, clinical pregnancy and implantation rates.3-5 Women with Stage III and IV endometriosis can develop endometriomas, or cysts arising from ectopic endometrial tissue implanted in the ovary with invagination of the ovarian cortex. In the setting of IVF, endometriomas can make oocyte aspiration difficult due to limited visualization of the follicular cohort.6,7 As a result, clinicians often obtain a lower yield of oocytes.4 In addition, there is an increased risk of inadvertent fenestration of the endometrioma, which has been shown to cause inflammatory peritonitis, and if aspirated into the egg retrieval needle, can be detrimental to the oocyte.8
Studies have presented conflicting findings regarding the benefit of surgical excision of endometriomas on pregnancy outcomes. Beretta and colleagues compared laparoscopic cystectomy to laparoscopic drainage and bipolar coagulation of endometriomas and found that the 24-month cumulative pregnancy rate was higher in the cystectomy group with a similar complication rate; whether these results are related to the drainage itself or the use of coagulation is not known.9 More recently it has been noted that surgical management of endometriomas may be associated with decreased ovarian responsiveness and a lower number of oocytes retrieved during a subsequent IVF cycle.10
Given the risk of ovarian damage with cystectomy, an alternative to laparoscopic surgery, transvaginal drainage, has been explored as a minimally invasive option to reduce injury to the ovarian cortex while improving pregnancy outcomes. Ultrasound-guided transvaginal aspiration was initially found by Alboughar and colleagues to be an effective treatment of endometriosis-related pain. Studies have further shown an improvement in fertilization rates for patients undergoing endometriotic cyst aspiration compared to patients who did undergo treatment or who underwent surgical treatment prior to IVF.11,12
Although aspiration alone is an option for management of benign cysts, the high recurrence rate prompted further studies on whether instillation with a sclerosing agent would reduce cyst recurrence. Early data on renal cysts suggested that using a sclerosing agent such as 95% ethanol was a safe and effective method to treat cysts.13 Lipitz et al.14 evaluated aspiration of peritoneal cysts with 95% ethanol and observed no complications or recurrences in their small cohort. In the gynecologic literature, several groups have examined aspiration compared to ethanol sclerosis for both ovarian cysts and endometriomas. Two studies have suggested that the use of ethanol sclerosis for ovarian endometriomas prior to IVF does not adversely affect ovarian reserve, but it also does not improve IVF outcomes.15,16 However, Yazbeck and colleagues demonstrated that it was associated with lower recurrence rates of endometriomas and higher pregnancy rates when compared to simple aspiration.17
In this study, we aimed to evaluate the impact of aspiration of endometriomas with ethanol sclerosis compared to aspiration with saline on subsequent ovarian hormonal response, including day 3 follicular stimulating hormone (FSH), day 3 estradiol, and peak estradiol, as well as IVF success, measured by number of follicles identified, number of oocytes retrieved, and HCG outcome, in women with recurrent endometriomas who had previously undergone an unsuccessful IVF cycle. Subsequent endometrioma recurrence rates were also examined. We hypothesized that cyst aspiration would have no deleterious effect on ovarian response and improve oocyte yield in the post-aspiration IVF cycle.
Study design
This study was conducted at Tufts-New England Medical Center and was approved by the Tufts University Institutional Review Board during the investigation and by the Partners Investigational Review Board for data analysis, as the primary investigator changed institutions. Subjects were prospectively recruited from the Tufts-New England Medical Center Reproductive Endocrinology and Infertility (REI) practice between 1998 and 2002. Within the REI practice, providers were aware of the study and informed eligible patients. Patients were recruited through 2002, when the principle investigator moved to a different institution. Participating subjects were randomized to one of two cyst aspiration protocols using a computer-generated code that was placed in a sealed envelope and opened by the provider when the patient consented at the time of the procedure: cyst aspiration with saline or a 95% ethanol solution. Therefore, the only person not blinded to the study group was the surgeon performing the procedure. Because the participants underwent IVF both before and after cyst aspiration, they served as their own controls.
Subject selection
Eligible participants had at least stage III endometriosis with laparoscopic ovarian cystectomy within the previous 12 months ensuring benign pathology; a failed first IVF cycle within six months post-laparoscopy; and endometrioma recurrence confirmed by ultrasound, who were then advised to proceed with endometrioma aspiration prior to a subsequent scheduled IVF cycle. Further inclusion criteria were the following: age 18-42; BMI < 40; adequate ovarian reserve based on day 3 FSH < 13.5 mIU/ml, day 3 estradiol < 80 pg/ml and antral follicle count (AFC) > 5; and ovarian endometrioma > 2.0 cm diagnosed by ultrasound. Anti-müllerian hormone (AMH) levels were not performed as the assay was not widely available at the time of study recruitment. If patients expressed interest in the study, the details of the study as well as inclusion and exclusion criteria were explained to the patient by research study staff. Exclusion criteria were the following: age > 42; BMI ≥ 40; abnormal ovarian reserve by day 3 labs or AFC; complex ovarian cysts with thick septa, solid components, or multiple loculations on ultrasound; and other co-morbidities that would preclude IVF, an egg retrieval or oocyte aspiration. The recruited patients were provided with the study protocol and asked to sign an informed consent, after which they were randomized to one of the two groups. Eligibility criteria did not change during trial recruitment. Demographic factors of interest included age, number of years infertile, and BMI.
Cyst aspiration
Cyst aspiration was performed by the study primary investigator within one month prior to oral contraceptive start. Subjects underwent conscious IV sedation under the supervision of an anesthesiologist. A transvaginal 7.5 MHz General Electric transvaginal ultrasound probe with a needle guide attached and a 17-gauge egg retrieval needle (Cook Medical, Inc., Bloomington, IN) was used to enter the endometrioma. For the saline aspiration group, all cyst fluid was aspirated into a labeled container and then the cyst was flushed with saline until the fluid returned clear. For the ethanol group, all cyst fluid was aspirated and the cyst was flushed with saline until the fluid returned clear. Without removing the needle, the cyst was then filled to 50% of the original volume aspirated with a 95% ethanol solution. The needle and fluid were left in place for five minutes, after which all the fluid was aspirated. The ovarian aspirate was sent to cytology for evaluation.
IVF cycle
After cyst aspiration, subjects underwent a second IVF cycle identical to their first IVF cycle prior to cyst aspiration. Dosing could be altered as the cycle progressed based on the subject’s response. Subjects were pre-treated with the same combination oral contraceptive agent used in their first cycle for three weeks. Ovarian stimulation was performed with a luteal phase GnRH agonist protocol and recombinant FSH, and IVF was completed in the usual fashion. Follicles greater than 10mm were aspirated at the time of egg retrieval. Two embryos were transferred in both cycles per center guidelines at that time.
Ovarian response markers of interest at each cycle included day 3 follicular stimulating hormone (FSH), day 3 estradiol, and peak estradiol. Follicle number and number of oocytes retrieved from both the affected (aspirated) and non-affected (contralateral) ovaries were assessed as IVF outcomes. Recurrence of endometriomas was assessed at the time of post-aspiration egg retrieval. Human chorionic gonadotropin levels were also measured 14 days after embryo transfer in each cycle.
Statistical analyses
All statistical analyses were done with the Mann-Whitney U, Wilcoxon Signed-Rank, and Fisher’s exact tests through SAS (Statistical Analysis System). A P value of ≤ 0.05 was considered statistically significant.
Patients had similar demographic characteristics and endometrioma size
From the eligible population of infertility patients seen at the Tufts-New England Medical Center REI clinic, 22 women were recruited to participate in this study, 10 randomized to the saline group and 12 to the ethanol group. Importantly, no significant difference was found between the two groups’ demographic characteristics (Table 1). HCG was negative for all patients 14 days after the pre-aspiration IVF cycle embryo transfer. All ovarian aspirates had negative cytology.
|
Saline1 (n=10) |
95% Ethanol1 (n=12) |
P-value2 |
|
|
Age (years) |
33.5 (4.0) |
33.5 (5.5) |
0.62 |
|
Years Infertile |
3.0 (1.0) |
2.0 (1.8) |
0.28 |
|
BMI, kg/m2 |
25.5 (4.0) |
24.0 (4.5) |
0.44 |
|
Cyst size (mm) |
40.0 (10) |
47.5 (17.5) |
0.23 |
Table 1 Demographics of patients who underwent endometrioma aspiration with saline or 95% ethanol
1Values expressed as median (interquartile range)
2P ≤ 0.05 is significant.
Ovarian response and IVF outcomes vary after endometrioma aspiration with saline vs. 95% ethanol
In the IVF cycle prior to cyst aspiration, the patients in the saline and ethanol groups had similar median day 3 FSH levels (8.2 mIU/ml vs. 7.8 mIU/ml, p = 0.89), day 3 estradiol (36.5 pg/ml vs. 48.5 pg/ml, p = 0.69), and peak estradiol levels (1951 pg/ml vs. 1962 pg/ml, p = 0.82). In both groups, the pre-aspiration IVF total aspirated follicle number was 10 and the number of oocytes retrieved was 8 (Figure 1).
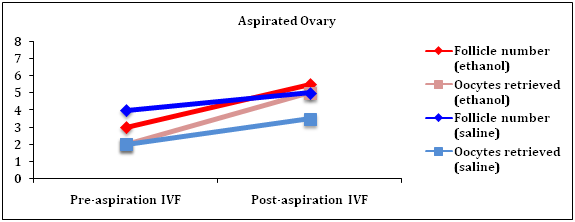
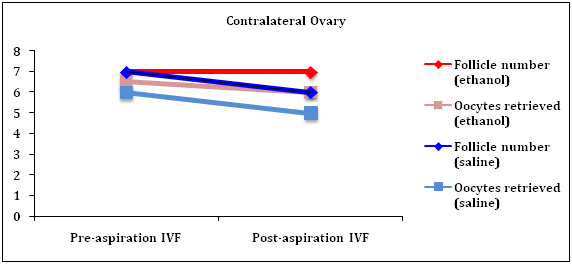
Figure 1 IVF outcomes before and after endometrioma aspiration with saline or 95% ethanol. The trend of the median number of follicles and oocytes retrieved from the pre- (initial) to post-aspiration IVF cycles is displayed for both the aspirated (A) and contralateral (B; non-aspirated) ovaries for both study groups. In the aspirated ovaries, there was a significantly greater increase from the initial IVF cycle in the number of follicles identified and oocytes retrieved for the 95% ethanol group compared to the saline aspiration group (p < 0.01 and p = 0.04, respectively). There was no effect in the contralateral ovaries.
After cyst aspiration, day 3 FSH and estradiol levels remained similar between the two groups (7.8 mIU/ml vs. 7.7 mIU/ml and 35 pg/ml vs. 43 pg/ml, respectively, (Table 3). Interestingly, however, the ethanol group achieved a significantly higher median peak estradiol level after ovarian stimulation than the saline group, 2598 pg/ml compared to 2107 pg/ml (p = 0.04), and the peak estradiol levels in both groups were higher post-cyst aspiration than pre-cyst aspiration (Tables 2 & 3).
The median number of total oocytes retrieved was significantly higher in the ethanol group compared to the saline group post-cyst aspiration (11 vs. 10, p = 0.03). Furthermore, there was a trend towards a higher median number of follicles post-cyst aspiration in the ethanol group compared to the saline group (13 vs. 11.5, p = 0.06). Most importantly, in the aspirated ovary, use of ethanol compared to saline was associated with a greater increase in the median number of oocytes retrieved (3 vs. 2, p = 0.04) and number follicles identified (3 vs. 2, p < 0.01) in post-aspiration IVF compared to pre-aspiration IVF (Figure 1). Cyst aspiration regardless of fluid used did not impact the number of oocytes or follicles in the contralateral ovary, which were similar between the saline and ethanol groups pre- and post-aspiration (Figure 1).
Aspiration with 95% ethanol may increase pregnancy rate and decrease risk of endometrioma recurrence
Positive HCG levels were detected in 50% of the ethanol group patients compared to 30% of the saline group, which was not significant (Figure 2). The clinical recurrence rate of endometriomas, determined at the time of baseline ultrasound for post-aspiration IVF, was 40% in the saline group versus 25% in the ethanol group, though again this was not a statistically significant finding.

Figure 2 Endometrioma recurrence rates and HCG outcomes following endometrioma aspiration with saline or 95% ethanol. The recurrence rates of endometriomas in this population were 40% in the saline group compared to 25% in the ethanol group (p=0.65). Positive HCGs were obtained following post-aspiration IVF in 30% of subjects in the saline group compared to 50% of subjects in the ethanol group (p = 0.41).
Optimizing IVF outcomes for women with Stage III and IV endometriosis will require a strategy that eliminates endometriomas while preserving the ovarian cortex. Endometriomas in many cases cause pelvic pain that affects the patient’s daily quality of life, and their presence can limit the ability of a provider to visualize follicles on ultrasound and safely perform egg retrieval during an IVF cycle without inadvertent cyst fenestration. It is unclear whether the development of endometriomas itself, distinct from the effect on visualization during IVF procedures, impacts IVF outcomes. Histological studies have illustrated that the ovarian cortex surrounding endometriomas contain fewer follicles than tissue surrounding other benign cysts.18 Furthermore, endometriotic cysts contain higher levels of inflammatory markers and free iron, which is associated with oxidative stress.19 In the context of IVF, one study on patients with unilateral endometriomas who had not undergone prior surgical intervention demonstrated a 25% reduction in the number of co-dominant follicles in the affected ovary compared to the unaffected ovary following ovarian hyperstimulation with gonadotropins.20 However, a later study by the same group determined that there was no significant effect of endometriomas on ovarian responsiveness to gonadotropins or oocyte development.21 These studies are limited by small sample sizes, and the ultimate impact on clinical pregnancy and live birth rates is not assessed. Given the histologic and molecular data, as well as the technical challenges that endometriomas present at the time of egg retrieval, expectant management is often not recommended.
Although cystectomy has traditionally been viewed as the gold standard for management of endometriomas, recent studies have illustrated that surgery has a detrimental impact on ovarian reserve due to removal of normal ovarian cortex surrounding the cyst.18 A meta-analysis by Raffi and colleagues found that after laparoscopic ovarian cystectomy, patients had a decrease in AMH levels, indicative of decreased ovarian reserve.22 In cases of recurrent endometriomas, therefore, repeated surgeries would not be a reasonable option for patients suffering from infertility and intending to undergo IVF. Aspiration of endometriomas prior to IVF presents a minimally invasive alternative for this population of women, particularly since existing data suggests an advantage to intervening compared to expectant management in terms of oocytes retrieved and ovarian response. Furthermore, the use of 95% ethanol, a sclerosing agent thought to render the epithelial cells in the lining of cysts nonviable, has proven to be both safe and effective for benign cysts in the kidney, liver, peritoneum, and ovaries.13,14,23
To our knowledge, no other studies have compared cyst aspiration with saline and ethanol sclerosis prior to a second IVF cycle in women who have recurrent endometriomas status post laparoscopic cystectomy and a first unsuccessful IVF cycle. The management of this unique group of women is particularly challenging to their infertility providers. Successful randomization of our subjects allowed us to evaluate the use of ethanol sclerosis with aspiration of endometriomas compared to aspiration with saline alone, which acted as a control. Notably, the post-aspiration IVF cycle outcomes for both groups could also be compared to their first IVF cycle outcomes, which were performed prior to cyst aspiration but after laparoscopic cystectomy, with the same protocol. This internal control for each group is a major strength of this study.
We first demonstrated that while there was no difference in markers of ovarian response between the saline and ethanol group pre-cyst aspiration (Table 2), the peak estradiol was significantly higher in the ethanol group compared to saline group post-cyst aspiration (2598 vs. 2107, p = 0.04; Table 3). The increased estradiol level in the ethanol group suggests that there are no detrimental effects of ethanol on ovarian response. Furthermore, the peak estradiol level in the ethanol group was higher post-cyst aspiration than pre-cyst aspiration (2598 vs. 1962, Tables 2 & 3). It is possible that the lower ovarian response in the pre-cyst aspiration IVF cycle was rather a consequence of the prior laparoscopic cystectomy. In that context, we can conclude that aspiration is potentially superior to cystectomy in preservation of ovarian response to stimulation measured by peak estradiol in this specific group of women.
|
Saline1 (n=10) |
95% Ethanol1 (n=12) |
P-value2 |
|
|
Day 3 FSH (mIU/ml) |
8.2 (1.3) |
7.8 (1.3) |
0.89 |
|
Day 3 Estradiol (pg/ml) |
36.5 (30) |
48.5 (21) |
0.69 |
|
Estradiol (pg/ml) |
1951 (308) |
1962 (674) |
0.82 |
Table 2 Pre-aspiration ovarian response outcomes
1Values expressed as median (interquartile range)
2P ≤ 0.05 is significant.
|
Saline1 (n=10) |
95% Ethanol1 (n=12) |
P-value2 |
|
|
Day 3 FSH (mIU/ml) |
7.8 (10) |
7.7 (1.0) |
0.6 |
|
Day 3 Estradiol (pg/ml) |
35 (12) |
43 (16.5) |
0.32 |
|
Peak Estradiol (pg/ml) |
2107 (472) |
2598 (531) |
0.04 |
Table 3 Post-aspiration ovarian response outcomes
1Values expressed as median (interquartile range)
2P ≤ 0.05 is significant.
Among our subjects, cyst aspiration with ethanol also led to a higher number of follicles and a greater number of oocytes retrieved compared to both the saline group post-cyst aspiration and the IVF cycle in the same women pre-cyst aspiration. More specifically, the aspirated ovaries in the ethanol group demonstrated a significantly greater increase in the median number of oocytes retrieved and follicles observed from the pre- to post-cyst aspiration IVF cycle compared to the saline group. Reassuringly, aspiration did not negatively impact the contralateral ovary in either group based on the outcomes examined. The increase in oocyte yield in the ethanol sclerosis group may be secondary to improved follicular visualization during subsequent egg retrieval, as the recurrence of endometriomas overall was less with ethanol sclerosis, or potentially a greater reduction in inflammatory recruitment after endometrioma aspiration with ethanol sclerosis, leading to improved follicular growth within the surrounding ovarian cortex and minimizing the ability of the cyst to re-accumulate. The trend towards a higher rate of positive HCG outcomes in the ethanol group is likely associated with the increased oocyte yield seen in the post-aspiration IVF cycle. Consequently, this study suggests that cyst aspiration with ethanol sclerosis may lead to improved IVF outcomes compared to aspiration with saline alone and cystectomy in this particular group of women with recurrent endometriomas.
A prior study by Eppsteiner and colleagues found that oocyte yield increases from one IVF cycle to the next in women with normal ovarian reserve, a change associated with increased total gonadotropin dose in the second cycle.24 Notably, of those with normal ovarian reserve, about 45% underwent a change in stimulation protocol for the second cycle. Therefore, while it is possible that the change in aspirated follicles and oocyte yield observed in our study could be attributed to natural inter-cycle variation, this is less likely in the setting of consistent IVF protocols between cycles. Moreover, this underlying variation would be similar between the ethanol and saline groups due to randomization and therefore would not affect comparisons between these groups.
The study patients were recruited and treated at Tufts Medical Center, and the delay in data analysis occurred due to the transition of the primary investigator from Tufts to Massachusetts General Hospital. An important limitation to this study is the low power, a common challenge in research on this subject. Moreover, clinical pregnancy rates and live birth outcomes are poorly reported in this body of literature, and unfortunately long-term data on our study patients was not available to address this deficiency. Therefore, more randomized longitudinal data are required to determine if intervention on endometriomas prior to IVF affects long-term clinical outcomes. In addition, AMH was not a widely available assay at the time of data collection, and so changes in ovarian reserve before and after our interventions were not assessed with this parameter. Because the women included in this study were anticipated normal responders, it is unclear whether cyst aspiration with 95% ethanol would benefit poor responders. Finally, this study was limited to patients undergoing IVF, and cannot be extrapolated to patients undergoing other types of fertility treatments.
Our findings indicate that cyst aspiration with ethanol sclerosis is a valid minimally invasive approach to treat recurrent endometriomas in patients undergoing IVF. Aspiration with 95% ethanol leads to a greater increase between pre- and post-cyst aspiration IVF cycles in the number of oocytes retrieved and follicles visualized in the affected ovary compared to aspiration with saline, with no harm to the contralateral ovary. Furthermore, it tends to reduce the rate of recurrence compared to saline aspiration and prior cystectomy in this high-risk group of patients. Thus, in women with recurrent endometriomas, cyst aspiration with ethanol sclerosis can be offered as an alternative to cystectomy that may improve IVF outcomes, improve ovarian response, potentially minimize cyst recurrence, and facilitate ovarian egg retrieval.
The authors are grateful to the Tufts-New England Medical Center Reproductive Endocrinology and Infertility clinic staff for their assistance in the care of the study patients. There were no sources of funding for this project.
The authors have no conflicts of interest regarding this publication.

©2018 Sacha, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.