MOJ
eISSN: 2641-9300


Review Article Volume 1 Issue 6
IMO NovSU them, Yaroslav the Wise, regional clinical Oncology center, Russia
Correspondence: Cherenkov VG, IMO NovSU them, Yaroslav the Wise, regional clinical Oncology center, Russia
Received: November 05, 2018 | Published: December 26, 2018
Citation: Cherenkov VG, Alexandrov AS, Sycheva DN. The value of the residual “HPV load” after surgical treatment of cervical intraepithelial neoplasia. MOJ Tumor Res. 2018;1(6):197-199. DOI: 10.15406/mojtr.2018.01.00041
A comparative analysis of the studies of 330 patients treated for cervical intraepithelial neoplasia II-III degree, confirmed morphologically. In 36 women, the operation was repeated, associated with the recurrence of the disease. Performed loop electroconsult, after that, the wound surface of the cervix by using a disposable sterile probe was conducted swab, placed in transport medium and immediately sent to the laboratory. DNA from epithelial scraping was ekstragirovanie using sorption method (test systems LLC "Nextbio"), amplification was performed by standard methods using commercial test-system "AmpliSens" on the amplifiers in real-time rotary and flatbed types. Before treatment is sufficient to conduct quantitative tests for genes E6 / E7 HPV. For patients with a high level of residual viral load, as well as other authors, we came to the conclusion about the need for additional measures of relapse prevention, aimed at the use of immunotherapy, treatment of concomitant chronic infectious diseases and subsequent control.
Keywords: conization, carrying out residual load of HPV
As is known, the main method of treatment of cervical intraepithelial neoplasia (CIN, dysplasia) is surgical, usually performed by loop electroconization. In this case, the ectocervix epithelium is effectively removed, at the same time a large number of deep "crypts" can be unattainable with conization and can cause recurrence of dysplasia or further progression. Detection of viral load in the cut-off edge was carried out by a number of studies.1‒3 Test systems based on the nucleic acid amplification method are available in the Russian Federation and allow to perform viral load studies much cheaper (10-15 times). Moreover, in these tests it is possible to determine a more accurate quantitative characteristic, to identify separately oncogenes E6/E7. The aim is to study the role of viral load in the cut-off edges of oncogenic types in the epithelium of the wound surface immediately after conization. The study included 330 patients (2017-2018 years) treated for cervical intraepithelial neoplasia II-III degree, confirmed morphologically. In 36 women, the operation was repeated. Loop electroconization was performed, then a smear was carried out from the wound surface of the cervix using a disposable sterile probe, placed in the transport medium and immediately went to the laboratory. DNA from epithelial scraping was ekstragirovanie using sorption method (test systems LLC "Nextbio"), amplification was performed by standard methods using commercial test-system "AmpliSens" on the amplifiers in real-time rotary and flatbed types.
Negative cut-off edges were detected in 73 cases (21.6%). The virus was detected in 262 samples. In 23% of cases had "moderately oncogenic" types of HPV (types 31, 33, 35, 39, 51, 52, 56, 58, 59, 66, 68) alone or in combination with each other. In 35.3% of cases there was the most aggressive type 16, and in 17.1% of cases this type was combined with other types. Thus, the frequency of HPV16 was 67.9% of all positive cases, which is consistent with the literature data. According to the level of viral load, all positive cases were divided into 5 classes. Table 1 provides descriptions classes, the frequency of occurrence of each class of viral load, the frequency of the most oncogenic type 16 of the virus and the age of the patient at the time of surgical treatment.
Class |
The amount of virus, the genome-equivalent |
Frequency of occurrence among the positive cases, % |
Proportion of HPV 16 in class % |
Age women M±m |
1-low |
<0.01 |
14.9 |
71.8 |
36.5±8.6 |
2-moderate |
0.01-0.099 |
35.1 |
61.9 |
35.8±7.9 |
3-increased |
0.1-0.99 |
22.9 |
63.3 |
38.7±8.8 |
4 - high |
1-9.9 |
19.5 |
74.5 |
37.8±9.2 |
5-extremely high |
>10 |
7.6 |
85 |
34.7±7.2 |
Table 1 Distribution of samples with different levels of HPV (by conventional classes)
According to Table 1 there is a certain tendency to increase representation the most aggressive HPV-16 in the "high-loaded" regions, but in relatively clean, it also was not rare. Perhaps the latter phenomenon is explained by the faster development of pathology in cases with HPV 16 in the surface layers of the epithelium. It is also seen that the age of the woman did not affect the magnitude of the viral load. Histological data on samples subjected to HPV test (any viral gene) are shown in Figure 1. The diagram shows that at a high level of the virus light dysplasia, and at an extremely high level of load options "without pathology" are not found at all. Conversely, at low levels of the virus, carcinomas are rare (5.5%). There is also a tendency to increase the proportion of dysplasia of the 3rd degree with an increase in viral load (36% - 41% - 50% - 59% - 45%) and this trend is particularly clear in the observation of dysplasia CIN3 together with a group of carcinomas: 1st class – 41.7%, 2nd – 52.5%, 3rd – 67.3%, 4th – 69.4%, 5th – 70%.
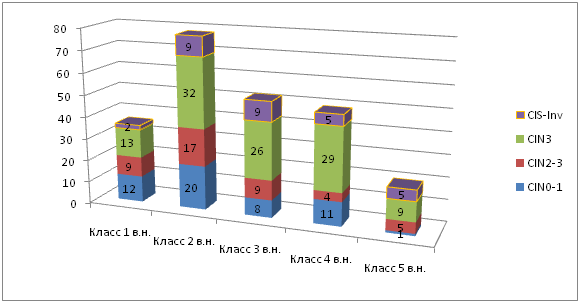
Figure 1 Distribution diagram of the number of samples with different levels (class) of viral load (VN) morphology (histological study: CIN, Intraepithelial neoplasia; CIS, Carcinoma it situ).
In an attempt to analyze the statistical reliability of differences in viral load (in native values), it was found that the number of virus differs significantly only between the group of carcinomas in situ and the groups "without pathology" or CIN1 (the reliability of p=0.0005 and p=0.006, respectively). Enlargement of the compared groups to two (with moderate or weak dysplasia and pronounced pathology) worsens statistical reliability (p=0.6). That is, with an obvious tendency to a higher residual level of viral load of cases with severe (morphologically) pathology, these signs are quite independent. In the analysis of the Association of relapses (n=36) of dysplasia with the level of viral load, it was found that the level of viral load measured by the content of one of the HPV genes: E1, E2, E6, E7 or others did not differ (p=0.8) in patients with relapse and without relapse. The analysis of grouped cases (classified by level) showed a certain tendency, but the differences in the groups were not significant (p=0.073, Figure 2). The analysis of the role of E6/E7 HPV genes revealed the following results. Cases with a high content of the virus (grades 3-5) at the level of genes E6/E7 were smaller. There were a number of cases where there was a high level of E6/E7 genes at low (more than twice lower) or undetectable level of E1/E2 genes (Figure 3). Comparing the results of HPV (E6/E7) test with the results of morphological study revealed significant differences in a significantly larger number of categories than in E1/E2 test. The content of E6/E7 genes did not change in the groups "without pathology" and "CIN1" (p=0.27). But comparing the categories "without pathology" and "CIN2" and the more "CIN3" clear differences were obtained (p=0.019 and p<0.000001). Also significant differences were obtained when comparing the categories "CN1" and "CN3" (p=0.00008) or "CIS-inv" (p=0.0066), as well as "CIN2" and "CIN3" (p=0.0058). Thus, the clinically significant pathology of the cervix is influenced to a greater extent by the level of genes E6/E7, rather than other viral genes.
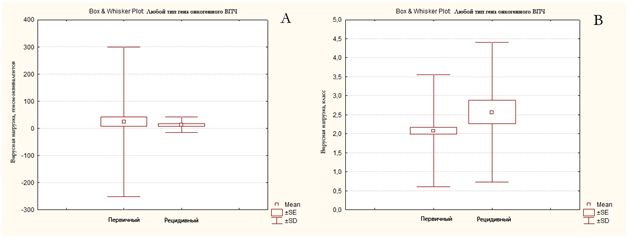
Figure 2 Dependence of recurrence of cervical dysplasia on viral load, determined by the level of General (and unspecified) viral genes. Figure A shows the distribution of cases in genome equivalents, and figure B shows the "classes" of viral load.
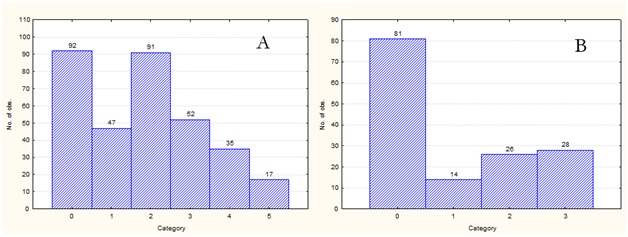
Figure 3The distribution of cases according to the level of genes E6/E7. On the histogram A - the number of cases without genes E6/E7 (category 0), with low (class, category 1), moderate, elevated, high and extremely high categories 2-5, respectively). On the histogram B-cases where E6/E7 genes dominated: category 1 – moderate level, 2 - high, 3 – extremely high.
The most interesting was the comparison of the results in patients with recurrent cervical disease and without relapses. Both the results of the morphological study and the HPV test showed a positive predictive value. In the group without relapse, severe dysplasia or carcinoma was observed in 49.8% of cases, in the group with relapses - 66.7% (comparing the level of pathology by the t-test criterion, the differences were significant, p=0.01). A high level of residual carrier of E6/E7 virus genes (more than 0.1 copies of the virus per human genome) was found in the group without relapse at a frequency of 27.6% and more than twice (57.1%) in the group with relapses (according to the t-test criterion, the differences are also significant, p=0.004) (Figure 4). For rice 4 the distribution of categories of morphological pathology and the level of viral genes in patients with and without registered relapses is shown. The highest levels of residual viral load were found in 40% of cases of recurrent disease and were three times rarer in the group without relapse. Unfortunately, in this study, not described prospective cases of recurrence (i.e., recurrences, held on the backdrop of the residual level of viral load), however, described nine cases have also highlighted the important role of residual viral load. Only one case of low (0.002 genome equivalents) levels of mixed viral infection (a combination of type 16 with other oncogenic HPV types) resulted in a relapse 5 months after conization. The other two cases were elevated (more than 0.1 genome equivalents) and the other six had high or extremely high viral loads. Thus, the positive predictive index for increased or higher E6/E7 gene content was 89%. Negative predictive index was-100% ("clean edges" for a short period of observation did not recurent).
None.
The author declares that there is no conflict of interest.

©2018 Cherenkov, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.