MOJ
eISSN: 2641-9300


Case Report Volume 1 Issue 2
1Department of Head and Neck Surgery, Croatia
2Department of Pathology and Cytology, Sestre milosrdnice University Hospital Center, Croatia
3Department of Pathology, School of Medicine, University of Zagreb, Croatia
4Division of Surgery, General hospital Nova Gradi?ka, Croatia
5Division of Pathology, General Hospital Zabok, Croatia
6Department of Pathology and Cytology, University Hospital Center Zagreb, Croatia
Correspondence: Bozo Kruslin, Department of Pathology and Cytology, Sestre milosrdnice University Hospital Center, Croatia, Tel 385 1 37 87 177, Fax 385 1 37 87 244
Received: April 11, 2018 | Published: April 20, 2018
Citation: Ledinsky I, Ulamec M, Jukic Z. Late metastasis of granulosa cell tumor mimicking primary angiosarcoma of the spleen; case report and literature review. MOJ Tumor Res. 2018;1(2):90-92. DOI: 10.15406/mojtr.2018.01.00019
A sixty-four year old female patient presented with a left upper quadrant abdominal pain. Magnetic resonance imaging and MSCT scans revealed a solid tumor of the spleen which was first suspected to be a primary angiosarcoma. The final diagnosis, made after splenectomy, was metastatic granulosa cell tumor, which arouse 15 years after a surgical treatment and radiotherapy of a primary ovarian tumor. The tumor was composed of solid sheets and papillary formations lined with atypical epithelioid cells, showing high mitotic rate and proliferative activity of up to 40%. Foci of necrosis and hemorrhage were abundant. Immunohistochemical analysis showed positive reaction for vimentin and calretinin and focally positive reaction for CD31, FVIII and inhibin. According to the English literature, metastatic granulosa cell tumor of the spleen is exceedingly rare, with only a few reported cases. Considering the possibility of late occurrence of metastatic granulosa cell tumor, this case emphasizes the need for close clinical-pathological cooperation in diagnosis and for long-term follow up of these patients.
Keywords: granulosa cell tumor, angiosarcoma, spleen
Granulosa cell tumor is an uncommon stromal cell tumor of the ovary, which is of low grade malignancy, but has an overall recurrence rate of 20-30%. It represents about 1% of all ovarian tumors.1 The majority of cases are associated with estrogenic manifestations such as metrorrhagia, endometrial hyperplasia, fibrocystic breast changes and, less commonly, with endometrial carcinoma. Androgenic manifestations occur rarely. These tumors are considered to be of low grade malignancy and may manifest metastatic disease more than 20 years after treatment of the primary. We present a case of a patient who developed a metastatic granulosa cell tumor of the spleen 15 years after the treatment of a primary ovarian tumor.
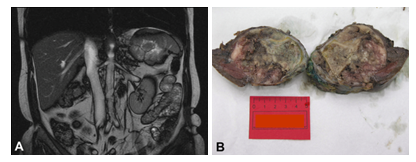
Sixty-four year old female patient was admitted to hospital due to left upper quadrant abdominal pain. Magnetic resonance imaging (Figure 1A) and MSCT examinations of the abdomen revealed a solid tumor of the spleen measuring up to 8.6cm in largest diameter. The patient underwent splenectomy, during which two nodes from the peritoneum were also removed. The patient was discharged from hospital on the 8th postoperative day following uneventful recovery, while protected by pneumococcal vaccine. The preliminary histological, histochemical and immunohistochemical analyses suggested a primary angiosarcoma of the spleen, but due to later obtained clinical data of prior gynecological tumor, a metastatic disease had to be excluded. Complete medical history, gained directly from the patient and her family, revealed that in 1995, the patient had uterus, both ovaries and tubes, as well as omentum removed due to granulosa cell tumor of the ovary. During that operation, the tumor had ruptured and the patient was referred to oncology for further radiation therapy. The patient was under regular gynecological follow-up, which had not shown signs of recurrent disease. In the light of newly obtained information, additional immunohistochemical examination with inhibin and calretinin was performed on the splenic tumor. The final diagnosis was metastatic granulosa cell tumor. PET/CT scan performed two months after the splenectomy did not show increased 2-Fluoro-[18F]-2-deoxy-glucose (FDG) metabolism, typical for metabolically active malignant cells. A few minor lesions in lungs, which did not show increased FDG accumulation, were of open etiology, thus follow-up was recommended. Based on oncologists’ decision, the patient underwent chemotherapy treatment according to PEB protocol (Cisplatinum, Etoposide and Bleomycin). Twenty six months after initial presentation, the patient was well without recurrence. Later on, the patient was lost from follow up.
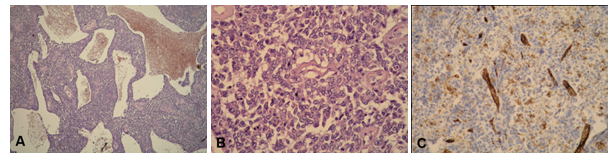
Pathological examination revealed relatively well delineated splenic tumor, measuring 8 x 7 x 6.5cm (Figure 1B). The cut-surface of the tumor was grey to brown, with areas of necrosis and hemorrhage. There were no lymph nodes isolated from the adjacent fat tissue. Histologically, the tumor was composed of solid sheets and papillary formations lined with atypical epithelioid cells (Figure 2A). Anastomotic, partly slit like vascular spaces lined with relatively uniform atypical cells with hyperchromatic, and/or vesicular nuclei with visible nucleoli, were also found (Figure 2B). Mitotic rate was high, up to 20mitoses/10 HPF. Necrotic areas and hemorrhage were abundant. Proliferative activity measured immunohistochemically with Ki-67 was 40%. Remnants of normal splenic tissue were found at the edge of the material. Extensive histochemical (PAS, Giemsa, Gomori) and immunohistochemical analyses (vimentin, CD31, CD34, FVIII, CD68, CK7, CK20, CD3, CD20, CD30, bcl-6, Ki-67, HMB-45) were made. Beside positive reaction to vimentin and focally positive reaction to CD31 (Figure 2C) and FVIII, all other markers were negative. Histologically, lymph nodes from the peritoneum did not contain tumorous tissue. The surrounding fatty and connective tissue contained remains of surgical catgut, mononuclear infiltrate and multinuclear giant cells of the foreign body type.
Preliminary histological, histochemical and immunohistochemical analyses suggested primary angiosarcoma of the spleen. However, the initial biopsy report and bioptic material of primary ovarian granulosa cell tumor were obtained. Tumor of the ovary measured up to 7cm in diameter, had a smooth capsule and was yellow on cut surface. Histologically, solid pattern of mostly small, cuboid to polygonal cells with Call-Exner bodies and focal necrosis were observed (Figure 3A). Tumor cells showed high mitotic activity. Therefore, additional immunohistochemical examination with inhibin and calretinin was performed on the splenic tumor. The tumor cells showed a positive reaction to calretinin (Figure 3B) and a focally positive reaction to inhibin. The final diagnosis was metastatic granulosa cell tumor.
According to the WHO classification of tumors, adult granulosa cell tumor of the ovary typically presents as unilateral, encapsulated node with smooth surface, yellow or grey in colour. Microscopically it consists of small, uniform cells of cuboid to polygonal shape, with small “coffee bean”- like nuclei showing grooves, and almost always focally forming Call-Exner bodies. Nuclear atypia is usually absent but mitotic activity is variable.1 Histological appearance cannot predict clinical behavior of these tumors.1,2 Primary tumor of here described patient showed solid pattern, focally forming Call-Exner bodies. Necrotic foci were present, as well as high mitotic rate, both of which are unusual for the granulosa cell tumor. Metastatic tumor was examined on 25 slides and there were no structures that could correspond to Call-Exner bodies. According to some studies, there are several immunohistochemical markers which may aid in diagnosis. On of these showed that inhibin is more specific, whereas calretinin is more sensitive marker.3 In our case, metastatic tumor showed a positive immunohistochemical reaction to calretinin and focally positive to inhibin.
Metastases of granulosa cell tumor occur in 25-30% of the cases. Local recurrences or foci of peritoneal spread are more common than real metastases which are described in liver, pancreas, lungs and bones, but are very rare.4,5 Only a few cases of metastatic granulosa cell tumor of the spleen are described in the literature.6‒9 In 1977 Laczkovics6 described the first case of metastatic granulosa cell tumor of the spleen, diagnosed 19 years after the primary tumor and five years after local recurrence.6The main symptom in this case was abdominal pain. Macroscopically, few white to gray nodes were detected in the spleen, the largest measuring 14 cm in diameter. Histologically, these nodes showed typical features of the granulosa cell tumor with relatively high mitotic rate.6 In our case, only one tumorous node was found in the spleen. Ylagan et al.,7 presented a patient with cytologically diagnosed metastatic tumor in the spleen 21 years after the primary granulosa cell tumor.7 Clinical-pathological cooperation and accurate clinical data were critical in this case. Lal et al.,8 described cytological characteristics of 7 metastatic granulosa cell tumors. In one of those cases tumor metastasis was discovered in the spleen.8 In a case by Chew et al.,9 a splenic rupture resulted from metastatic tumor occurring 29 years after curative resection of granulosa cell tumor of the ovary. They also reviewed 27 literature cases with recurrence and metastases occurring more than 10 years after the primary tumor. Metastasis to spleen was described in only one of those cases.9
In 2008 Salani et al.,10 reported 3 cases of laparascopic management of granulosa cell tumor of the ovary with intraoperative rupture. Consequently patients underwent chemotherapy according to the BEP protocol. Five, eleven and thirteen years after treatment they were well and without recurrent disease.10 In our case, after intraoperative rupture of the primary ovarian tumor, the patient underwent radiotherapy. Metastatic disease manifested fifteen years after the treatment of the primary. Tumor rupture has been reported as a significant prognostic factor in patients with granulosa cell tumor of the ovary. These tumors and their metastases are hypervascular with propensity to rupture and cause abdominal pain and intraperitoneal hemorrhage.4 Differential diagnosis in our case primarily included angiosarcoma, which is rarely found in the spleen, but represents most common nonlymphoid primary malignant splenic tumor, accounting for 7.4% of all splenic primaries.11,12 The mean age at presentation for primary angiosarcoma of the spleen is 59 years, and it is more prevalent in males. The presenting symptoms usually include abdominal pain, splenomegaly, microangiopathic anemia, thrombocytopenia, coagulopathy and rupture.11,12 It is an extremely aggressive malignant neoplasm with 6 months median survival. Usually, at the time of diagnosis, the metastatic spread had already occurred. In the past, patients had often been treated by radiotherapy.11,12 In our case, the patient presented with left upper quadrant abdominal pain. Gross and histological examination showed vascular component, sheets of atypical cells and even papillary projections with hyaline cores, foci of necrosis and hemorrhage and high mitotic activity. To our knowledge, there are only a few reported cases of metastatic granulosa cell tumor of the spleen and we believe this is the first case of such metastasis after the intraoperative rupture of the primary ovarian tumor, in the English Literature.4‒9,13,14 These tumors have indolent growth and show late recurrence, even 25 years after inital treatment.4‒9,13,14 It has been difficult to evaluate the efficiency of the various therapeutic approaches used in treatment of this tumor. Our patient presented with the metastasis fifteen years after combined surgical and radiotherapy treatment. Due to late manifestations of metastatic disease, here described case emphasizes the need for close clinical-pathological cooperation in diagnosis and for long-term follow up for patients with granulosa cell tumor of the ovary.
None.
The authors declare no conflict of interest.

©2018 Ledinsky, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.