MOJ
eISSN: 2641-9300


Review Article Volume 1 Issue 6
North Manchester General Hospital, Department of Urology, United Kingdom
Correspondence: Anthony Kodzo-Grey Venyo, North Manchester General Hospital, Department of Urology, Delaunay?s Road, Crumpsall, Manchester, M8 5RB, United Kingdom
Received: November 25, 2018 | Published: December 19, 2018
Citation: Venyo AKG. Kaposi’s sarcoma of the penis: a review of the literature and update. MOJ Tumor Res. 2018;1(6):187-195. DOI: 10.15406/mojtr.2018.01.00040
Various types of Kaposi’s sarcoma exist including (a) the classic type, (b) the endemic type, (c) the transplant related type, (d) the epidemic type. Kaposi’s sarcoma of penis (KSOP) commonly affects the distal part of the penis and most commonly it tends to affect the glans penis and the coronal sulcus; however, it can also affect the foreskin as well as the shaft of the penis. There is no consensus opinion regarding the aetiology of KSOP because it has not been clarified whether the disease emanates as a reactive condition or it is a true neoplasm. In most cases of KSOP HHV8/KSHV tends to be detected. KSOP could present in any of the typical forms of the disease for example (a) a patch, (b) a plaque, (c) or as a nodular lesion on the glans, coronal sulcus, foreskin or shaft of the penis. KSOP could also present as blue-purple lesions involving the penis. Quite often KSOP lesions are seen as multi-centric penile lesions but isolated single lesion could be encountered occasionally. The findings on microscopic examination of KSOP would depend upon the stage of the lesion whether the lesion is in the patch stage, plaque stage or in the nodular stage of the disease. Immunohistochemistry studies of KSOP tend to show positive staining for: CD34; CD31; Factor VIII related antigen; Podoplanin (D2-40) but it would show negative staining for Desmin and Cytokeratin. A number of treatment for KSOP include: In cases of Kaposi’s sarcoma associated with HIV treatment is given for HIV for example with HAART; Local excision of the lesion; Cryotherapy; Laser therapy; Radiotherapy; Interferon alpha; Chemotherapeutic agents. The outcome of the disease following treatment depends upon the type of lesion and the treatment given; nevertheless, there is no consensus opinion on treatment and no comprehensive data on the outcome of KSOP. There is therefore need for a global multicentre trial on the treatment of KSOP in order to establish a consensus on treatment and to document the comparative outcomes following the various treatment options.
Keywords: Kaposi’s sarcoma, penis, Human Herpes Virus 8, HIV, HAART, Cryotherapy, Laser therapy, Radiotherapy, Interferon alpha, excision, Chemotherapeutic agents, CD34, CD31, Factor VIII related antigen, Podoplanin (D2-40)
Kaposi’s sarcoma is a low-grade vascular tumour which is caused by human Herpes virus 8 (HV*) a virus which is also called Kaposi’s sarcoma associated Herpes virus (KSHV) and the tumour also tends to be associated with HIV.1,2 Nevertheless, Kaposi’s sarcoma may sometimes affect individuals who do not have HIV infection. Kaposi’s sarcoma may affect various organs and may various types of Kaposi’s sarcoma exist. Kaposi’s sarcoma is on the whole a rare disease which most clinicians would not encounter frequently. Kaposi’s sarcoma of the penis (KSOP) is a very rate disease which does present with non-specific features that would require a high index of suspicion for it to be diagnosed easily but because of its rarity there is the possibility that the diagnosis of the disease might be delayed or the disease could easily be misdiagnosed. The ensuing paper on KSOP is divided into two parts
(A) Overview and
(B) Miscellaneous narrations and discussions from reported cases and literature.
Aims
To review the literature on Kaposi’s sarcoma of the penis.
Methods
Various internet search engines were used including google, google scholar, and PUBMED. The search word used was Kaposi’s sarcoma of the penis and Kaposi sarcoma. Sixteen references were identified that were used to write the article.
Overview
General Comments
Kaposi’s sarcoma of the penis is the commonest sarcoma of the penis.1
Definition
Kaposi’s sarcoma is a low-grade vascular tumour which is caused by human Herpes virus 8 (HV*) a virus which is also called Kaposi’s sarcoma associated Herpes virus (KSHV) and the tumour also tends to be associated with HIV.1,2
Epidemiology
Various types of Kaposi’s sarcoma exist including (A) the classic type, (B) the endemic type, (C) the transplant related type, (D) the epidemic type.
It has been stated that:
Aetiology
Clinical features
Clinical examination
General and systematic examination tends to be undertaken on all individuals who have Kaposi’s Sarcoma of the penis as part of the general assessment of the patient and also to ascertain if there are any other lesions elsewhere which would constitute disseminated disease. Presence and absence of lymph nodes in the groins, axillae and neck regions would also be required. All the systems would tend to examined carefully and if any abnormal clinical findings are made these would tend to be appropriately investigated.
Laboratory investigations
Haematology investigations
Haematological profile of all patients tend to be undertaken as part of the general assessment of patients who have Kaposi’s Sarcoma of the penis as general assessment of all patients but the results would not be diagnostic of the disease.
Biochemistry investigations
Serum Urea and electrolytes, liver function tests and blood glucose tend to be undertaken as part of the general assessment of each individual with Kaposi’s Sarcoma but the results would not be diagnostic of the disease. Nevertheless, if an individual is found to be diabetic or has an impaired biochemical profile this would be investigated accordingly and appropriate supportive treatment would be offered as part of the general management of the individual.
Urine microscopy and culture
Urine analysis, urine microscopy and culture tend to be undertaken as part of the general assessment of individuals and if there is evidence of urinary tract infection this would then be treated to improve the general health of the individual but the results of the urine test would not be diagnostic of Kaposi’s Sarcoma of the pens. Microscopy and culture of discharges from any associated ulcerated lesions of the penis. In the even of an ulceration and discharge from a penile lesion in an individual who has Kaposi’s Sarcoma of the penis a swab and culture of the discharge would tend to be undertaken to confirm presence or absence of an infection and if infection is confirmed, based upon the sensitivity pattern of the organism, an appropriate antibiotic treatment can be given.
Radiological investigations
Because Kaposi’s Sarcoma of the penis could mimic other diseases including other malignancies it would be important to undertake a full clinical and radiological assessment of each individual to ascertain whether the disease is a local or disseminated disease and this may require undertaking ultrasound scan of abdomen and pelvis, or computed tomography (CT) scan of abdomen and pelvis, or magnetic resonance imaging (MRI) scan of abdomen and pelvis.
Ultrasound scan
Ultrasound scan of abdomen and pelvis may be normal or it could reveal enlarged lymph nodes if there are enlarged lymph nodes.
CT scan
CT scan of abdomen and pelvis could be normal but in the case of disseminated or extensive Kaposi’s Sarcoma, the scan would reveal the extent of the disease.
MRI scan
MRI scan of abdomen and pelvis could be normal but in the case of disseminated or extensive Kaposi’s Sarcoma, the scan would reveal the extent of the disease.
Specific tests for HIV infection
In cases of suspicion of HIV infection, HIV screening test would be undertaken and a full HIV work up would then be undertaken for HIV positive individuals. Furthermore, when diagnosis of Kaposi’s Sarcoma of the penis is confirmed based upon histology examination of a biopsy specimen of the penile lesion, HIV laboratory testing tends to be undertaken to exclude possible HIV infection and the tests tend to include: Serology assays EIAs, and rapid tests), CD4 enumeration technologies, and molecular technologies. Antibodies to HIV-1 and HIV-2 tend to be tested by EIA (enzyme-linked immunoassay [ELISA], simple test devices, and western blot (WB) tests.
Treatment
A number of treatment options tend to be adopted and some of these include:
Macroscopic features
Gross examination tends to reveal small 2 to 6 mm bluish penile lesions which tend to be multiple and are most often found on the glans penis1 but they may be found on the coronal sulcus, foreskin and shaft of the penis.
Microscopic features
The findings on microscopic examination of Kaposi’s sarcoma of penis would depend upon the stage of the lesion whether the lesion is in the patch stage, plaque stage or in the nodular stage of the disease.
The patch stage disease
Microscopic examination of Kaposi’s sarcoma that has presented in the patch stage of the disease would tend to reveal the ensuing:
The plaque stage disease
Microscopic examination of Kaposi’s sarcoma of the penis that has presented in the plaque stage of the disease would tend to show the following:
Microscopic examination of Kaposi’s sarcoma of the penis that has presented in the nodular stage of the disease tends to reveal the ensuing:
Immunohistochemistry
Immunohistochemistry studies of Kaposi’s sarcoma of the penis tend to show positive staining for:1
Positive staining
CD34
CD31
Factor VIII related antigen
Podoplanin (D2-40)
Negative staining
Immunohistochemistry studies of Kaposi’s sarcoma of penis tend to show negative staining for:1
Differential diagnoses
Some of the differential diagnoses of Kaposi’s sarcoma of penis include:1
Outcome
Perhaps the outcome following treatment of Kaposi’s sarcoma could be discussed based upon the type of Kaposi’s sarcoma and treatment given. It has been iterated that there is no available standard treatment guideline for primary Kaposi’s Sarcoma of the penis.3 Considerations related to the treatment of Kaposi’s Sarcoma of the penis have been summated as follows:3 Treatment for Kaposi’s sarcoma tend to include: local surgical excision, radiotherapy, chemotherapy, and treatment with laser.3 Treatment that involves utilisation of adjuvant alpha or beta interferon has been has been undertaken in some cases.3
Quite commonly, surgical excision has been recommended for a small solitary lesion, on the other hand, conservative radiotherapy could be utilised for large lesions.3 Systemic chemotherapy tends to be reserved for more advanced cases of Kaposi’s sarcoma associated with visceral involvement or in the situation of generalised lesions.3
Kaposi’s Sarcoma of penis associated with HIV infection would also tend to be treated HAART. The clinical course of primary Kaposi’s sarcoma of the penis would tend to be variable, and it would appear that no consistent follow-up data does exist. Nevertheless, local recurrences tend to be rare if the Kaposi’s sarcoma lesion is completely removed.3 It has been stated that the onset of new Kaposi’s sarcoma lesions could be observed pursuant to a period of approximately 1 year to 2 years.4
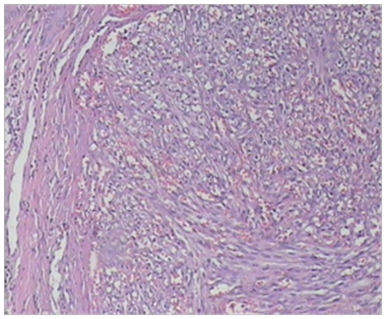
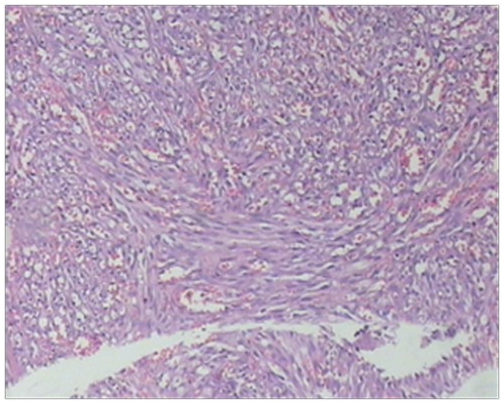
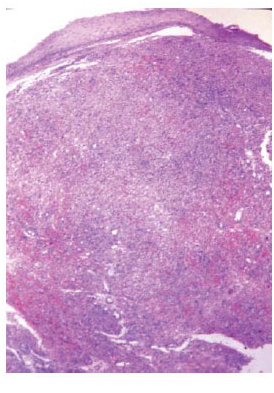
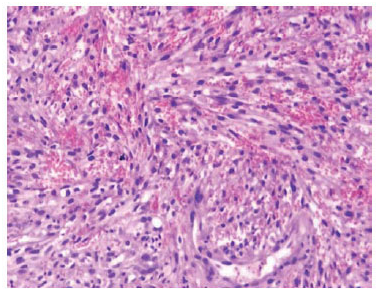
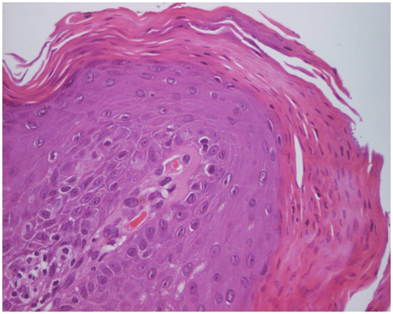
Miscellaneous narrations and discussions from some reported cases
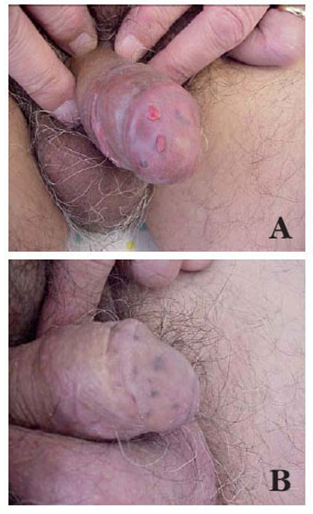
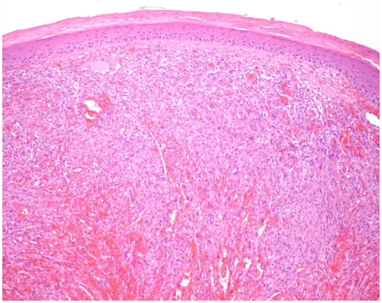
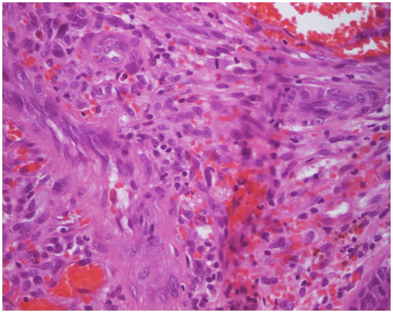
Karami et al.5 reported a 47-year-old man who had suffered from itchy papules on his penis which had started for the first time 5 years earlier. The lesion appeared for the first time as a violet sub-coronal papule which measured which measured approximately 5 mm in diameter. Over the preceding 3 months the lesion had rapidly extended with the development of multiple lesions that looked like the original lesion around the corona of his penis. Apart from removal of a stone from urinary tract 7 years earlier he did not have any significant past medical history or medical treatment. He had once had extra-marital unprotected sex. His general and systematic examinations were normal apart from observation of popular indurate glandular and sub-coronal lesions and some of the lesions were encrusted (Figure 1 & 2). The results of his full blood count, urinalysis and urine culture were normal. The serology results on two occasions for HIV, HBV, and HCV virus were normal. HHV8 was detected in tissue by PCR method in a sample of biopsy specimen of the lesion. Microscopic examination a wedge biopsy specimen of the penile lesion showed spindle cells, around the blood spaces and ectatic capillaries. The examination also showed fibrotic connective tissue containing hemosiderin deposits and mild inflammation of lymphoplasmatic inflammatory cells that had enveloped the spindle cells and blood spaces (Figure 3 & 4). Based upon the aforementioned findings, a diagnosis of Kaposi form of vascular proliferation was made He had ultrasound scan of renal tract which showed a calculus in his left kidney. He had computed tomography (CT) scan of abdomen, pelvis and thorax which was normal and he also underwent endoscopic examination of his urinary tract and gastrointestinal tract was normal He received radiotherapy treatment.


Lebari et al.6 reported a 40-year-old man with HIV-1 infection with CD4 count of 551 cells per cubic millilitre and an undetectable viral load who presented with two skin-coloured Kaposi’s sarcoma lesions on the prepuce of his penis. Diagnosis of Kaposi’s sarcoma was established after histological examination of specimen of the lesions. He had been started on anti-retrovirus therapy 3 years prior to his presentation with a nadir CD4 count of 255 cells per cubic millimetre. He did achieve and did maintain viral suppression upon commencing anti-retroviral therapy. He had initially undergone cryotherapy and 5% imiquimod when a provisional diagnosis of a wart was made. He did not respond to the initial therapy and that led to further investigations which established the diagnosis of Kaposi’s sarcoma of penis. They summarized their review findings of literature on Kaposi’s sarcoma reported over the preceding 10 years and they had found 10 published cases of Kaposi’s sarcoma of penis in HIV negative men and only one published case of Kaposi’s sarcoma in an HIV-positive man, who had severe immune suppression with CD4 count below 200 cells per cubic millimetre Their reported case was therefore the first case of a report of an HIV-positive patient who was stable on anti-retroviral treatment with a CD count greater than 200 cells per cubic millilitre and suppressed HIV-1 viral load to have developed two Kaposi’s sarcoma lesions. Lebari et al.6 stated the following
Mukai et al.7 reported a 64-year-old man who had a history of a violet lesion on his external urethral meatus for 8 months, that was associated with lower urinary tract symptoms. The lesion was excised and histological examination of the lesion was reported as being consistent with a diagnosis of haemangioma. He subsequently developed similar lesions on his penis and one was bleeding (Figure 5). He was found on examination to have right inguinal lymph node enlargement. He underwent biopsy of one of the penile lesions and histological examination of the biopsy specimen showed features consistent with Kaposi’s sarcoma (Figure 6 & 7). He had VDRL and HIV serological tests and the results were negative. He underwent 40 sessions of radiotherapy treatment to the penile lesions and by the end of his treatment the nodules had diminished and small ulcerations had remained in his balanopreputial sulcus due to the therapy but this healed after 30 days (Figure 8A & 8B). Mukai et al.7 stated the following:
(a) the classic,
(b) the endemic,
(c) iatrogenic,
(d) and AIDS associated forms.
(a) pyogenic granuloma,
(b) moluscum contangiosum,
(c) condyloma acuminate,
(d) Bowenoid papulosis8

It had been recommended that therapy should be chosen for each patient taking into consideration the fact that there is no consensus regarding treatment of the disease and that with regard to small and single lesions surgical excision could be recommended.8 Following complete excision of the primary lesion recurrence tends to be rare. Relapse / recurrence of Kaposi’s sarcoma lesion tends to occur between 6 months and 2 years pursuant to the procedure. With regard to larger and multiple lesions, the best therapeutic option is radiotherapy and recurrence tends to be infrequent. With regard to advanced diseases associated visceral and generalized involvement by Kaposi’s sarcoma, chemotherapy could be a good option of treatment. Radiotherapy treatment for Kaposi’s sarcoma of the penis should include a periodic and continuous follow-up monitoring in view of the fact that fibrosis of the penis, erectile dysfunction, and new lesions not treated by the radiotherapy may subsequently develop.10,11
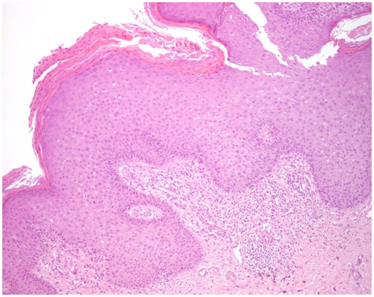
Morelli et al.12 reported an HIV-negative 53-year old man who presented with a 0.7cm elevated reddish lump on the glans of his penis which had been unsuccessfully treated with cortisone which required excision in September 1996 and histological examination confirmed Kaposi’s sarcoma with the margins of excision clear of the sarcoma. The tumour cells were positive for Kaposi’s sarcoma-associated HHV-8. Histological examination of the specimen showed a vascular proliferation within the submucosa consistent with the plaque stage of Kaposi’s sarcoma. The tumour cells were composed of epithelioid spindle cells had been surrounding the proliferating vascular channels and had formed a coalescence which constituted the classic nodular lesion. He had computed tomography scan, upper and lower gastrointestinal endoscopies which were normal. He had remained well and without recurrence of Kaposi’s sarcoma 7 years after his presentation as well as sero-negative for HIV. Pinto-Almeida et al.13 reported a 47-year old man who presented with painless exuberant papules and nodules on his penis which had enlarged rapidly in the preceding six months. One month prior to his presentation he had been diagnosed as having human immunodeficiency virus (HIV) type 1 infection. He was not on any medication and he did not have any significant past medical history. On examination he was found to have violaceous confluent nodules that had smooth lobular surface that measured between 5mm and 10mm in diameter and had occupied the entire circumference of the corona. Furthermore, over the foreskin and glans penis there were multiple skin-coloured verrucous papules that measured 2mm and 5mm (Figure 9–11). Histological examination of the violaceous lesions showed vascular proliferation at all levels of the dermis and fascicles of spindle cells that had replaced the dermal collagen and had been separated by dilated and angulated vascular in a slit-like pattern as well as the mitotic index was low (Figure 12 & 13). The features were consistent with a diagnosis of Kaposi's sarcoma. Histopathological examination of the skin-coloured lesions did show acanthosis, parakeratosis, elongation of the rete ridges, vascular dilatation, and presence of koilocytes, findings which were adjudged to be compatible with a diagnosis of genital warts (Figure 14 & 15). Molecular biology studies undertaken did exclude high-risk human papilloma virus. His CD4 lymphocyte counts were low (69 per cubic millilitre) and the viral load was high with 16034 copies per millilitre. The rest of his blood test results were within normal range. He had computed tomography scan of thorax, abdomen and pelvis which was normal. The tumour was staged as low risk Kaposi’s sarcoma of penis (confined to the skin -T0, CD4 lower than 150 per cubic millimetre I1, no systemic illness – S0). He refused to undergo surgical treatment. He was commenced on HAART, which comprised of emtricitabine 200 mg per day, tenofovir 245mg per day, efavirenz 600mg per day, which resulted in good clinical, immunological and viral load outcome. Viral suppression was attained in the seventh month. After twenty months of management by HAART without any surgical excision or any other treatment, complete remission of both penile cutaneous lesions of Kaposi’s sarcoma and verrucae had been achieved (Figure 16). After twenty months of HAART suppression of the patient’s viral load had been achieved with an HIV-1 viral load of less than 20 copies per millilitre and his CD4 counts were 196 per millilitre. The patient was free of lesions at his 1-year follow-up. Hernández-Bel et al.14 reported an 80-year-old man who presented with an asymptomatic tumour on his penis which had been growing rapidly over a 2 weeks period He did not have any significant past medical history. He was found to have a soft pink pedunculated nodule which measured 10mm on the coronal sulcus of his penis. He also had a second well circumscribed painless red violaceous lesion which measured that had been present for many years. His examination was normal Histological examination of the larger lesion showed a multinodular proliferation of tumour which comprised of fusiform cells that had lengthened hyperchromatic nuclei and occasional mitosis. Bundles of the cells had formed disruptions that contained blood cells. A number of areas of eosinophilic globular bodies and hemosiderin deposits were also observed. Immunohistochemistry studies of the lesion showed positive staining for CD31 and CD34. Histological examination of the excised second lesion showed similar pathology features as that of the first excised lesion. The patient’s full blood count, coagulation studies, T cell count were normal and his HIV test on two occasions showed that he was seronegative. A diagnosis of primary Kaposi’s sarcoma in an immunocompetent man was made. At his one year follow-up the patient was well with no evidence of a recurrent lesion.




Soufiane et al.15 reported a 73-year-old man who presented with a tumour on his glans penis which had started like a macule and then changed to a papule before developing into a tumour over a period of nine months. His clinical examination revealed a an exophytic tumour on his glans penis with ulcerated and surrounded by small purplish macules. His clinical examination was otherwise normal apart from his exophytic penile lesion on his glans penis. The results of his full blood count, serum biochemistry tests and HIV serology were all normal. He underwent excision of the tumour mass and electrocoagulation of the small macule. Histological examination of the excised lesion showed spindle cells that had nuclear atypia and occasional mitosis as well as blood-filled vascular slits which was adjudged to be consistent with a diagnosis of Kaposi’s sarcoma of penis. Human herpes-8 DNA was detected within the tumour tissue. He had CT scan of abdomen and thorax which was normal. He also had radiotherapy treatment for the lesion and at his 2-year follow-up he was well without any evidence of recurrence of tumour.
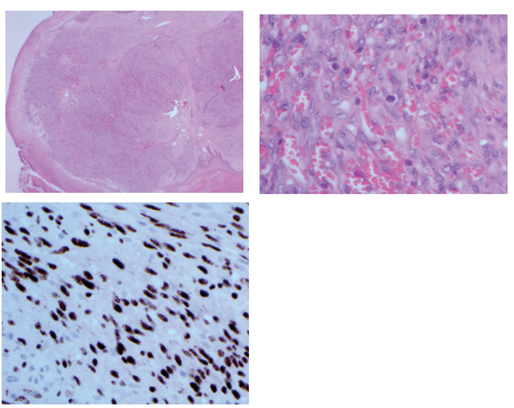
Momen et al.16 reported a 21-year-old HIV-negative Somalian man who had been diagnosed with an immunohistochemically proven human herpes virus 8 (HHV8)-positive primary Kaposi’s sarcoma of penis. He denied any previous sexual activity. On examination he was found to have a 1 cm polypoid nodule on the right side of his external urethral meatus and a 5 mm subcutaneous nodule on the left side of his glans penis. He was treated by means of local excision of 2 penile lesions and had remained in complete clinical remission for 18 months. Histological examination of the specimen showed spindle cell lesions. Immunohistochemistry studies of the lesions showed positive staining for and HHV8. Immunohistochemistry studies of the lesions also showed negative staining for Desmin. Histological examination of the initial lesions showed that the lesions had extended to the deep margins so further wide excision was undertaken which showed clear margins. Figure 17 for the histology features and the immunohistochemistry features seen Momen et al.15 stated that their case was the first case of a heterosexual teenage and young adult patient to be diagnosed with primary Kaposi’s sarcoma of the penis without a history of sexual intercourse. Momen et al.15 further stated that their case would provide clinical evidence that Kaposi’s sarcoma may be transmitted via other routes than via sexual intercourse.
Kaposi’s sarcoma is an important cause of morbidity in HIV-infected patients. Kaposi’s Sarcoma of the penis can affect both HIV-negative individuals as well as HIV-infected individuals. Kaposi’s sarcoma of the penis could affect sexually active and non-sexually active males. The presentation of Kaposi’s sarcoma of the penis is non-specific and this tends to mimic the presentation of other diseases. A high-index of suspicion is required to diagnose the disease. Diagnosis of Kaposi’s Sarcoma of the penis would require histology examination of biopsy specimens of the penile lesion (s). Treatment of the lesion(s) would depend upon the size and extent of the lesion(s).
None.
The authors declare that there is no conflict of interest.

©2018 Venyo. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.