MOJ
eISSN: 2641-9300


Research Article Volume 1 Issue 5
1Department of Surgical, City Clinical Hospital, Russia
2Candidate of Medical Sciences, Nizhny Novgorod, Korablestroiteley ave, Russia
3Head of the surgical department, Nizhny Novgorod, Russia
4Surgeon, Nizhny Novgorod, Russia
5Surgeon of one category, Nizhny Novgorod, Russia
Correspondence: Martynov Vladimir Leonidovich, Department of Surgical, City Clinical Hospital ?12 Sormovo district of Nizhny Novgorod, Russia
Received: August 10, 2018 | Published: September 4, 2018
Citation: Martynov VL, Andrey S, Nikolaevich RV, et al. Prevention of the syndrome of bacterial overgrowth in the small intestine when the right- hemicolectomy for cancer. MOJ Tumor Res. 2018;1(5):144-151. DOI: 10.15406/mojtr.2018.01.00033
Relevance: One of the reasons of the small intestinal bacterial overgrowth syndrome (SIBOS) - excision of a bauginiyev valve at a right-hand hemicolectomy both in planned, and in the emergency order that demands not only restoration of continuity of an intestinal tube, but also a restore of the lost function of the ileocecal valval device.
Purpose of the study: To develop and introduce safe, effective and public areflux in medical activity it is of fine-colon anastomoses in planned (primary anastomosis) and emergency (the delayed compression anastomosis) surgeries.
Materials and methods: New ways of formation the areflux thin-colon anastomoses in the conditions of the emergency and planned surgery for prophylaxis of development SIBOS in a small intestine are suggested, which is confirmed by the hydrogen breathing test.
Results: A right-sided hemicolectomy at 20 patients with primary fine-colon anastomosis without areflux device resulted in 60% of cases to development of the small intestinal bacterial overgrowth syndrome (SIBOS) in a small bowel, at 19 patients with primary anastomosis with formation of the areflux device reduced risk of development of SIBOS to 16%. When forming of the delayed areflux compression thin-colon anastomosis by an author's technique of SIBOS did not develop at 72% of patients.
Conclusions: Bauginiyev valve - the important structure of a human body is created by nature which areflux function needs to be modelled at a right-hand hemicolectomy
Keywords: a right-hand hemicolectomy, thin-colon anastomosis, SIBOS
When performing sided hemicolectomy removes antireflux apparatus (bauginievoy flap) ileocecal junction, which plays a fundamental role in preventing enteric-thick reflux and development of a number of pathological conditions including bacterial overgrowth syndrome (ARIS) in the small intestine.1 The actual prevalence of ARIS for today is unknown.2 This syndrome practitioner for understanding the difficult of.3 One of the leading pathogenesis at ARIS - premature deconjugation primary bile acids (BA).4,5 Dekonyugirovannye LCD have detergent properties, and therefore are capable of damaging the epithelial layer of the small intestinal mucosa,6 until complete atrophy microvilli,6 which leads to disruption of membrane digestion, creators, amilorei and steatorrhea, rising vitamin deficiencies6,7 exacerbate diarrhea syndrome.4,7,8 In fact, this pathological condition badly diagnosed due to the low specificity of its symptoms, which are often clinicians are major producing ARIS disease.9 One of the reasons ARIS - retrograde colonization of the small intestine from the lower GI tract by removing bauginievoy valve for right hemicolectomy in a planned and urgently.10,11 Currently, the tendency is registered adaptation mezhkishechnogo anastomosis under conditions of emergency surgery.12 But contraindications to primary intestinal anastomosis are not clearly defined, focus is only on the experience of the surgeon, without objective evidence. In our view a guide should be the degree of impairment of intra-abdominal pressure. Thus, intra-abdominal hypertension II-III-IV degrees in the pre- and postoperative period causes a disturbance of microcirculation in the intestinal wall, respectively, degrees of abdominal hypertension at 20, 40 and 50% of normal, reduced perfusion pressure of 30-40%.1,13
Develop and implement medical activity safe, efficient and widely accessible areflux thin-colonic anastomoses in the planned (primary anastomosis) and emergency (delayed compression anastomosis) surgery.
For comparison, three prevention SibRO used method for forming thin-colonic anastomosis performed in a planned and emergency surgery: a double-row side by side in joint constructions without areflux, end to side to form arflyuksnogo mechanism deferred mezhkishechny compression anastomosis (OMKA) with areflux structure. Indications for forming OMKA when emergency operation is determined by the values of intra-abdominal pressure, namely, II-III-IV degree. The degree of abdominal pressure increase was determined by measuring the pressure within the bladder, which is currently the method of choice.
Formation of a primary ligature areflux finely-colonic anastomosis as prevention ARIS at scheduled sided hemicolectomy14
After completion sided hemicolectomy transversely isoperistaltic superimposed thin-colonic anastomosis end to side; the free portion of omentum with missed therethrough nonabsorbable implant ligature is cut out to 200mm and a width of 10-12mm, which is held by the edges mesenteric anastomoziruemyh portions small and large intestine 3-4cm from the proximal anastomosis formed; by linking the ends of the implant ligature around anastomoziruemyh portions small and large intestines formed a ring, the circumference of which is equal to the diameter of the colon (Figure 1). By increasing the intraluminal pressure in the colon cult to above intracavitary pressure in the ileum, colon compresses the ileum to the chassis, which performs the function of the ring created by the implant, and the contents of the colon is not received in the small intestine (Figure 2). If the pressure in the lumen of the colon is less than the pressure in the ileum, the latter is not crushed and its contents enters the colon (Figure 3). As a result, simulated operating in standalone mode, an arbitrary design for areflux function area thin-colonic anastomosis and prevention ARIS in the small intestine. In carrying out reconstructive intervention in order to impart properties areflux formed in the previous step is thin-colonic anastomosis operation starts with a laparotomy, In peritonitis, ileus formation primary anastomosis dangerous high probability of failure and fatal complications.
We have developed hardware compression forming finely-delayed colonic anastomosis in embodiment areflux
ARIS for prevention for emergency sided hemicolectomy.16 Designed and constructed apparatus, which is a clamp Fedorov, in which the jaws are parallel to each other are arranged two needle of 2.5mm diameter, 50mm in length. In the needle-tube nozzle wear Medical steel and a length equal to the length minus the length of the needle "sharpener" needles, and 2.6mm in diameter. Nozzles are composed of two parts, a greater length determines the length of the anastomosis. For example, 10mm and 40mm, 25mm and 25mm, 20mm and 30mm. (Figure 4) (Figure 5) (Figure 6). Operation is as follows: the tube-selected nozzles, depending on the length of the anastomosis formed and its distance from the puncture. Wear on the nozzle needle, first - a lower part, and then - greater. Resecting the affected portion of the intestine, the distal end of the intestine sutured tightly, some distance from 10-12cm which gray-serous seam isoperistaltic crosslinked portions small and large intestine for about 10cm below the leaving compounds not crosslinked 15cm area for subsequent removal on its stoma. Departing from the seam lines 1cm, at the edges of two portions protivobryzheechnyh intestine through two puncture needle device is introduced with tubes, two nozzles in the intestine lumen. Device maximum jaws approach each other and fixed in this position (Figure 7). Ligatures № needle 5 through the bowel wall parts is performed under large-nozzle tubes at 3 points (the middle and at the edges). Above the serosa at the site of contact between the intestinal loops laid nonabsorbable yarn, then over which tightly bind the ends of the ligatures № 5, which causes further compression of constant wall tissue two segments between crosslinked gut-tubes nozzles (Figure 8). Laid along fold line anastomotic suture, orienting its ends to the intestinal stoma and is carried through a needle introduced through the lumen and through the wall of the small intestine extending on the stoma (Figure 9), (Figure 10). The needle is removed. Necessary areflux finely-delayed colonic anastomosis is achieved by compression to form a ring around the intestines anastomoziruemyh above 3-4 cm free section of OMKA omentum with drawn therethrough nonabsorbable ligatures analogously primary areflux finely-colonic anastomosis (Figure 11). Ligature retaining the tubular metal structure is fixed to a gauze ball (Figure 12).
Needles remaining to them in small pieces of tubes, nozzles removed from the lumen of the gut, leaving most of the tubes, nozzles in their lumen. The puncture site is sutured Z-shaped seams, locating them behind the line of anastomosis. Impose a second row of gray-serous sutures. The small intestine to the stoma output. After 8 - 11 days of compression lines occurs nekrotizirovanie tissues and intestinal walls interconnected large part-ducts nozzles for ligature outputted through the stoma to the outside. More rational manufacturing factory option unit (Figure 13). After 10-12 months after surgery, patients underwent a follow-up examination. To evaluate the effectiveness areflux anastomoses performed barium enema. Extremely important is repeated X-rays after a bowel movement, as during defecation maximum pressure is created in the intestine, which is accompanied by regurgitation of a radiopaque substance into the ileum in the absence of adequate areflux apparatus.
Diagnosis of ARIS. In order to determine the small intestine ARIS patients indirect methods of diagnosis performed:
These follow-up studies were conducted anticipating irrigoscopy 1 month or 1 month after her. Patients did not receive antibiotic therapy, diet therapy is not performed well as a course for at least 1 month prior to the study. These conditions can not affect the biocenosis of the small intestine. Statistical analysis was performed using Fisher's exact test.
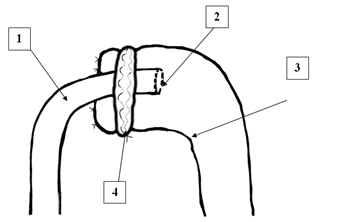
Figure 1 Scheme of formation of arefluous small intestine anastomosis: 1 - ileum; 2 - transverse anastomosis; 3 large intestine; 4 - areluxe device.
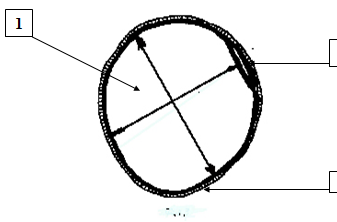
Figure 2 Scheme of the areluxe structure - pressure in the lumen of the colonic stump (1) above the pressure in the lumen of the small intestine (2), which is compressed by the colon on the framework of the implant (3).
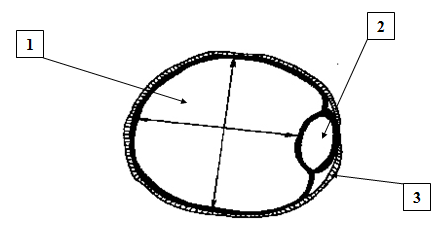
Figure 3 The pressure in the lumen of the colon (1) is less than the pressure in the ileum (2), due to this the latter is not squeezed on the frame (3) and its contents enter the large intestine.
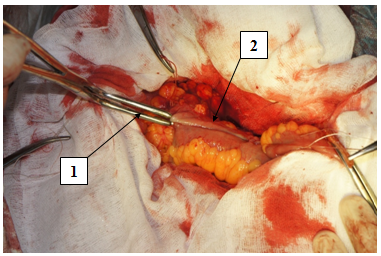
Figure 6 Branches of the device (1) are as close as possible, fixed, maximally compress the walls of the connected intestines (2).
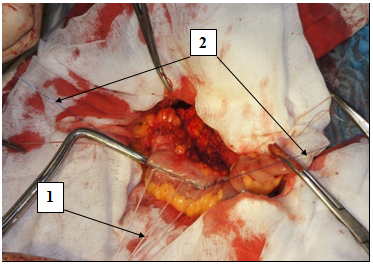
Figure 7 Three ligatures hold tubules (1), compressing tissues of the intestinal wall; one ligature (2) - to hold the tubes in the luminal cavity.

Figure 8 Through the lumen and the wall of the small intestine (1), going to the stoma, a needle (2)
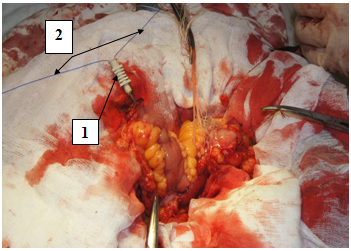
Figure 9 Through the lumen of the needle (1), the ends of the ligature (2) holding the tubular metal structure
Inclusion criteria were 64 patients in the study - the implementation of right-sided hemicolectomy for cancer of the right half of the colon. The patients were divided into 3 groups. Criteria for inclusion in one group (19 patients), - forming a primary areflux finely-colonic anastomosis on the developed methods. Criteria for inclusion in the 2nd group (25 patients), - forming a delayed mezhkishechnogo compression anastomosis (OMKA) in areflux embodiment with breeding ileostomy when the execution of the primary finely-colonic anastomosis was dangerous due to the high risk of its failure when intra-abdominal hypertension II-III-IV degrees. Criteria for inclusion in the group 3 (20 patients), - creation of finely-colonic anastomosis side in the right-side after gemikoektomii areflux without forming apparatus.
After surgery recovery of gastrointestinal function observed in all groups at day 3-5 (median days after surgery - 4 days) (Table 1). Retrospective analysis of surgical complications arising after sided hemicolectomy, conducted (Table 2) according to the classification Clavien-Dindo (The Clavien-Dindo Classification of Surgical Complications, 2009). In the first group (forming the primary areflux finely-colonic anastomosis - 19 patients) to complications attributed I degree 2 cases of wound infection to item II. - 2 cases of thrombosis ileofemoralnogo (did not require surgery) and other complications were observed. In the second group (formation OMKA 25 patients) to complications attributed I degree 2 cases of wound infection to item II. - 2 cases of blood transfusions to Article III. - 4 cases (IIIa Art. -in 2 cases of spontaneous anastomosis disclosure has not occurred within 3 weeks. For their disclosure required additional manipulations as violent impacts on the finger metal structures and the region of the anastomosis through a stoma;IIIb Art. -in 2 cases the anastomosis and not opened, they are made reconstructive surgery), to Article IV. - 1 case (IVb Art -. Multiorgan failure as a consequence preoperative peritonitis colonic obstruction on the ground, which caused death at 5 days after surgery before the disclosure anastomosis - V v.). In group 3 (the formation of nervichnogo finely-colonic anastomosis without areflux apparatus 20 patients) to complications attributed I degree 2 cases of wound infection to item II. - 2 cases of blood transfusions toArticle III. - 2 cases (IIIb Art. -two patients occurred anastomotic leak, which required emergency surgery, which was accompanied by renal insufficiency - IVa The criteria were anastomosis disclosure defecation through the rectum and the appearance of a radiopaque substance in the colon, when administered through a catheter in ileostomy (Figure 14). Term their disclosure ranged from 11 to 15 days - the median days disclosure anastomosis after surgery - 12 days. Insolvency superimposed compression anastomosis were observed. In 4 cases after anastomosis disclosure colostomy closure was carried out at initial hospitalization without discharge from the hospital. In other cases, a patient after anastomosis and discharge opening closure colostomy was performed at rehospitalization. Control examination carried out after 10-12 months after surgery.
Barium enema
In 20 patients, which is formed without creation of a primary anastomosis device obturator contrast freely fed into the small intestine (Figure 15). In 19 patients in the formation of a primary anastomosis created developed obturator device contrast is not fed into the small intestine at 15 (Figure 16) or in it determined traces 4 (Figure 17). Fisher index = 0.01488.
ARIS study on VDT
Of the 20 patients who completed without hemicolectomy areflux VDT device revealed ARIS 12 (degree 1 - y 2, the second degree - at 2, 3 degree - in 8). Of the 19 patients who had primary areflux formed thin-colonic anastomosis VDT ARIS defined in 3, wherein the one degree. Fisher index = 0.00791.
ARIS study on indikanu urine
Of the 20 patients who completed without hemicolectomy areflux device urine qualitative reaction indican was positive in 10 of 19 patients and with the formation areflux device - at 3. Fisher index = 0.04074.
The first results of the delayed hardware compression forming finely-colonic anastomosis in areflux embodiment for preventing ARIS for emergency sided hemicolectomy
In contrast barium enema cast into the small intestine was not detected in 21 patients, and 4 were determined in the small intestine of contrast marks. Of the 25 patients with the formation areflux device when OMKA VDT ARIS revealed in the small intestine in 7 patients (1 degree - in 5 degree 2 - y 2) - 28%. The positive reaction of urine on indican detected in 1 patient. - 4%.

Figure 14 Contrast, introduced through the ileostoma, enters the large intestine (1) - the anastomosis is uncovered.
Primary areflux thin-colonic anastomosis |
OMKA |
Primary finely-colonic anastomosis device without areflux |
||||
Number of patients |
N = 19 |
N = 25 |
N = 20 |
|||
|---|---|---|---|---|---|---|
planned |
Headline |
planned |
Headline |
planned |
Headline |
|
12 |
7 |
2 |
23 |
6 |
14 |
|
Median age (years) |
69 |
70 |
69 |
73 |
72 |
72 |
The median number of concomitant diseases |
2 |
2 |
3 |
3 |
3 |
3 |
Indicators abdominal pressure before operation (number of patients) |
I Art. - 12 |
I Art. - 7 |
I Art. - 0 |
I Art. - 0 |
I Art. - 6 |
I Art. - 14 |
II Art. - 0 |
II Art. - 0 |
II Art. - 2 |
II Art. - eleven |
II Art. - 0 |
II Art. - 0 |
|
III Art. - 0 |
III Art. - 0 |
III Art. - 0 |
III Art. - 12 |
III Art. - 0 |
III Art. - 0 |
|
IV Art. - 0 |
IV Art. -0 |
IV Art. -0 |
IV Art. -0 |
IV Art. - 0 |
IV Art. - 0 |
|
The severity of the scale SABS II |
<10/0 |
<10/7 |
<10/0 |
<10/0 |
<10/0 |
<10/0 |
(Score / quantitative |
10 - 29/0 |
10 - 29/0 |
10 - 29/0 |
10 - 29/11 |
10 - 29/0 |
10 - 29/7 |
of cases) |
30 - 49/0 |
30 - 49/0 |
30 - 49/0 |
30 - 49/8 |
30 - 49/0 |
30 - 49/7 |
50 - 69/0 |
50 - 69/0 |
50 - 69/0 |
50 - 69/6 |
50 - 69/0 |
50 - 69/0 |
|
Table 1 Characteristics of the study groups of patients
|
Primary areflux finely-colonic anastomosis (N=19) |
OMKA (N=25) |
Primary finely-colonic anastomosis without areflux device (N=20) |
I power |
2 |
2 |
2 |
II Art. |
2 |
3 |
2 |
III Art. |
- |
4 |
- |
IIIa Art. |
- |
2 |
- |
IIIb Art. |
- |
2 |
2 |
IV Article |
- |
- |
- |
IVa Art. |
- |
- |
2 |
IVb Article |
- |
1 |
- |
V Art. |
- |
1 |
- |
Table 2 Postoperative complications (by Clavien-Dindo)
Nearly two decades in the domestic literature the notion of ARIS, and in the wake behind it - a sufficient number of works on this subject, but mostly therapeutic areas. One reason ARIS all authors note unanimously inconsistency bauginievoy valve, its removal sided hemicolectomy Field.2‒4,8 About surgical correction of ARIS are only a few works, and the practice of medicine for this problem does not pay attention.16 One possibility is to provide a preventive ARIS areflux finely-sided colonic anastomoses after hemicolectomy, due not only to the reduction of the continuity of the intestinal duct, but with replenishing lost obturator function ileocecal valve apparatus.16,17 In practice the hitherto most commonly used conventional kontsekontsevye, longitudinal and lateral kontsebokovye finely-colonic anastomosis, a consequence of which the average anastomotic leak generated manually suture the hub constitute 2,6-8,4% and postoperative mortality - 2.9-7.1%.18,19 Only some authors propose to form fine-colonic anastomoses, having a valve properties.16,17 Creating innovative technology methods for forming thin-colonic anastomoses, Currently, there advocates the primary and the opponents mezhkishechnogo anastomosis in conditions of emergency surgery,12 the routine surgery all surgeons finely-formed primary colonic anastomosis.
Application delayed compression intestinal anastomoses in ileus conditions reduces the frequency of early postoperative complications to 4.5%,20 followed by minimal inflammatory manifestations, being alternative two-stage surgical approach.21‒23 But the complexity of processing and manufacturing of NiTi significantly increases the cost of construction thereof.23,24 and makes them relatively difficult to access. To make a decision on the formation of a primary anastomosis, in our opinion, should focus on the details abdominal pressure, which affects the microcirculation in the intestinal wall. Conclusive studies showing that intra-abdominal hypertension II-III-IV degrees in the pre- and postoperative period causes a disturbance of microcirculation in the intestinal wall, respectively, degrees of abdominal hypertension at 20, 40 and 50% of normal, reduced perfusion pressure of 30-40%.1,13 This prompted us to abandon after anastomosis formation primary sided hemicolectomy under conditions of increased intraabdominal pressure II-III-IV degree. But the loss of the ileocecal obturator apparatus transition practical medicine does not pay attention, that entails the development in the small intestine ARIS all pathological effects.15 We have developed a safe, public methods areflux forming apparatus during the formation of the primary and delayed finely-colonic anastomosis.15 Conduct hydrogen breath test, determination of urinary indican proves the effectiveness of the proposed methods for reducing the risk of development in the small intestine ARIS to 16%, which is diagnosed in 60% after anastomosis without areflux function. Method OMKA possible to avoid 95% of patients complex reconstructive operation, limited only ileostomy closure, to eliminate 72% SibRO development in the small intestine. Public methods areflux forming apparatus during the formation of the primary and delayed finely-colonic anastomosis.15 Conduct hydrogen breath test, determination of urinary indican proves the effectiveness of the proposed methods for reducing the risk of development in the small intestine ARIS to 16%, which is diagnosed in 60% after anastomosis without areflux function. Method OMKA possible to avoid 95% of patients complex reconstructive operation, limited only ileostomy closure, to eliminate 72% SibRO development in the small intestine. Public methods areflux forming apparatus during the formation of the primary and delayed finely-colonic anastomosis.15 Conduct hydrogen breath test, determination of urinary indican proves the effectiveness of the proposed methods for reducing the risk of development in the small intestine ARIS to 16%, which is diagnosed in 60% after anastomosis without areflux function. Method OMKA possible to avoid 95% of patients complex reconstructive operation, limited only ileostomy closure, to eliminate 72% SibRO development in the small intestine. The above leads us to conclude that bauginieva flap - created by nature important structure of the human body, areflux function which to be modeled at sided hemicolectomy (Figure 18).25f‒29
None
The author declares there is no conflict of interest.

©2018 Martynov, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.