MOJ
eISSN: 2641-9300


Case Report Volume 1 Issue 2
Institute of Medical Education, Oncology course Novgorod University Yaroslav the Wise, Russia
Correspondence: Cherenkov VG, Institute of Medical Education, Oncology course Novgorod University Yaroslav the Wise, Russia
Received: February 26, 2018 | Published: March 27, 2018
Citation: Cherenkov VG. Improving the effectiveness of screening and treatment of HSIL pathologies. MOJ Tumor Res. 2018;1(2):66 – 69. DOI: 10.15406/mojtr.2018.01.00014
Despite of every women who regularly conducting PAP test, cervical cancer appeared on every fourth of them. To improve PAP test, it is recommended to Cervex-brush (Combi) Rovers for receiving material from the zone of transformation and crypts of the cervical canal. "Liquid Cytology" allows using material for HPV. Correction of a program of cytological screening and treatment of HPV - associated diseases. Analysis of the period between identifying НCIL and entering the clinic showed: only 59 women (of 3.09%) from 1905, appealed in 10 days, 685 (35,9%) women appealed in year, 71 female sent smear on glass. Other women not appealed on clinic for other reasons. Female policlinic do not take on account until the diagnosis is confirmed in dispancer. 1165 women for 2013-2016 was not treated, while the share of advanced forms of cervical cancer has reached -32,7%. In order to control the detection of HSIL and treatment of us in 2016 introduced the "signal card" and sending them to oncologic clinic. After conization of cervical uteri should be administered and carried out by the control оf the cervical canal for HPV. Prescribed Isoprinosine and observation and HPV-test in 6 months. Thus, the introduction of signal cards, control and HPV, treatment isoprinosine of HSIL pathologies, allowed us to treat of 96.2±2.3%, recurrent HSIL and cancer has not been observed.
Keywords: HSIL pathology, conization, immunomodulators, control of the HPV, signal cards
HPV, Human papilloma virus; SIN, Squamous intraepithelial lesion; LSIL, Low grade squamous intraepitelial; lesion, Squamous intraepithelial lesion (CIN I and the presence of HPV); HSIL, High grade squamous intraepithelial lesion (CIN II, III, CIS); PCR, Polymerase chain reaction; PAP, test for Pap test; CIS, Cancer in place, 0 stage (carcinoma in situ); ASCUS, Flat cells with changes qualitatively insufficient for setting LSIL; AGUS, Cells of glandular epithelium with changes qualitatively insufficient for setting LSIL; RWK, Radio wave conization; It, Immunotherapy (isoprinosine)
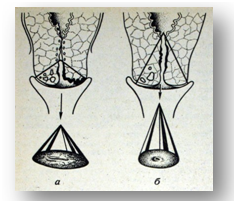
Cervical cancer is one of the few diseases in Russia has a tendency to rejuvenate and increase the frequency of diseases.1,2 Cervical cancer develops gradually from previous lesions, and even earlier it is preceded by infection in almost all cases with viruses, mainly NIP 16 and 18 types.3 Why this fact is not to be used for the prevention of cervical cancer. What's he supposed to be? To date, cervical cancer is the pathology, the development of which can be prevented. The greatest number of cervical lesions, including severe, falls on early reproductive age.4,5 The mentality of adolescents who start sexual activity in 14-16 years and earlier (M=15,6 years more than 55,7%, according to the anonymous survey of students) determines the frequent change of sexual partners, increases the risk of early infection with HPV.6 Therefore, the study of the cervix should begin as soon as possible: taking into account the age of sexual activity. More than 80 years (1928) the method of cervical pathology search is the classical cytological examination of cell smears (PAP-test) using a special brush on the scale of national programs. However, along with the obvious "advantages", the cytological examination also has significant disadvantages that can hinder the work of the doctor and delay timely treatment.7 It is found that every third case of Cervical Cancer according to different authors found in women who regularly passed cytological screening. Informative Papacy test depends on the level of training, as well as the quality of the sampling material. Smear can get too thick or thin, can be contaminated with blood elements, elements of inflammation, etc.8 The main way to improve the reliability of the cytological method of research is the use of the method of ”liquid Cytology" (Figure 1)(Figure 2). The doctor collects cells from the surface of the cervix and from the cervical canal with a special removable brush, which is placed in a bottle with a stabilizing solution. The latter prevents damage to cells, allows in optimal conditions to deliver the collected cells to the laboratory. In addition, the material obtained by the method of “liquid Cytology” is stored for several months and can be used for HPV studies. Data from randomized trials and meta-analysis of cohort studies with a high degree of reliability has proven that HPV – testing is a more sensitive method for detection of precancerous conditions of the cervix and cervical intraepithelial neoplasia (CIN II,III degree, CIS). Testing for HPV-BP is currently used in the United States and Europe as an addition to cytological cervical screening in patients 30 years and above. Almost all cases of CIN II and above due to a persistent infection. Nevertheless, 43% of these patients, including those with a normal cytological picture, have a positive outcome for HPV –BP. Strategy for genotyping of HPV was first presented by Thomas C. Wright from Columbia University on the basis of large-scale multicenter study. Screening in 16 and 18 types important additional information to PAP test data for predicting the risk of precancerous conditions and cervical cancer in women. These studies served as the basis for who to include HPV - BP in 2014 in the program of the examination for the detection of precancerous cervical pathology. Solving the organizational and methodological issues of improving the efficiency of cervical screening and mortality from cervical cancer in the Novgorod region on the example of the fgbi, through. N. N. Blokhin.9We analyzed the information content of the smears taken from the ecto - and the endocervix in women with verified process СIN II-III and CIS. Of the 178 patients taken from the endocervix "cervix-brush" 56 (31,4%) revealed an abnormal post-fusional cell. The rest of them are not revealed, which indicates the need to take away the material with the capture not only the zone of transformation, but also the crypt of the cervical canal with the help of Cervex-Brush Combi with plastic bristles on the Central pin (Figure 3).
The material was taken from the cervical canal at the visually normal cervix of the uterus. The mucous plug was carefully removed with a cotton swab. The brush with the bristles under the control of the eye cautiously directed to the Central part of the cervical canal, and then rotated it 3 times in one side and 2 to the other in order to get the cellular elements out deep layers of cervical epithelium. The brush was taken out of the vagina, separated by a finger from the rod and it was discharged into a special bottle with a preservative liquid for cytological examination and PCR. If the examination of the cervix in the mirrors midwife reveals cervical pathology, scraping it does not produce, and the patient directs, and better accompanies immediately to the gynecologist. From the standpoint of modern diagnostic and treatment tactics adopted International cytological classification of Bethesda (2001): ASUS or ASUS – respectively, the cells of flat or glandular epithelium with changes qualitatively insufficient for the formulation of LSIL –requires a second study in 6 months. LSIL - Low grade squamous intraepithelial lesion is a squamous intraepithelial intraepithelial lesion involving a low degree of dysplasia - CIN I and HPV infection. It is known that most women have to 28-30 years in the body itself gets rid of HPV – carriage. In the presence of other infections or reduced immunity and continued DNA. HPV, requires monitoring of the situation and conservative therapy. In such cases, we recommended gynecologist treatment with isoprinosine or neovir, acyclovir in combination with vitamin E and observation in a women's consultation with cytological control through 6 and 12 months. HSIL-high grade squamous intraepithelial lesion (CIN II, III, CIS) – recommended colposcopy, biopsy and referral to an Oncological dispensary for electroconidation and control of HPV and atypia. Treatment of the category of women with HSIL remains one of the topical and debatable. To date, immunotherapy approaches are not included in the standard of clinical application. This paper presents the results of a retrospective comparative cervical conization with pathology НSIL followed by treatment with immunomodulators and without its implementation. For electroconization of the cervix, we used a radiowave apparatus "Surgitron" and a special cone-shaped electrode, which allows by turning 360◦ to remove the cervix in the form of a cone by a single unit. Since 2011, we have performed 1002 conization at the age of 21 to 55 years. Until 2014, after conization, was treated with potassium permanganate 10% until it formed a scab and tampons with a syntomycin emulsion before it fell off, which was taken as a control group. Retrospective analysis of the outcomes of treatment of this group showed that, on average, in 9.8 (± 1.3%) cases with slight fluctuations over the years during 2-3 years, the progression of the disease (dysplasia, cancer in situ and in 2 cases, cervical cancer 1 stage, Table 1). In recent cases, it was necessary to increase the volume of surgery from trachelectomy and extirpation of the uterus.
Years |
Control group (НSIL) |
Study group (HSIL) |
|||
|---|---|---|---|---|---|
RWK* |
Including identifying resurgence |
RWKс IT* |
Including revealed |
||
HPV in crypts Revealed |
|||||
2011 |
89 |
9(10,1%) |
- |
- |
- |
2012 |
117 |
13(11,1%) |
- |
- |
- |
2013 |
172 |
15(8,7%) |
- |
- |
- |
2014 |
281 |
18 (6,4%) |
- |
||
2015 |
- |
378 |
89(23,5%) |
5(0,3%) |
|
2016 |
326 |
78(23,9) |
4(0,2%) |
||
Всего |
659 |
55(8,34±1,3) |
704 |
167(23,7%) |
9 (0,27±0,5%) |
Table 1 The results of immunotherapy of HPV associated cervical lesions (HSIL) after radio wave conization in comparison with the control group
*RWK, Radio wave conization; It, immunotherapy (isoprinosine)
Given the extremely high level of recurrence and the persistence of HPV in the crypts of the cervical canal, starting in 2015 after carrying out minimally invasive surgical interventions for HSIL (CIN II-III,CIS ) required manipulation of the steel cone biopsy with removal of the crypts (Figure 4) and the control of the upper cone cervical atypia and HPV. Women were discharged with recommendations for treatment with immunomodlators. In particular, neovir, inosine pranobex (isoprinosine) in the opinion of domestic and foreign authors, can achieve cure rates up to 96% after conization.9–11 The average duration of treatment was 28 days. When yousave НРV treatment was repeated, including sexual partner. However, in any case, the progression of lesions during the study period was not detected. Comparative statistical analysis of two groups of relapses "Statistic -6" showed that the difference between the results is reliable (P<0.05). However, tracing the pathway from the moment of HPV associated HSIL lesions detection to receipt in the year showed that only 39 women (2.1%) out of 1712 revealed in the last 2 years appealed within 10 days from the moment of diagnosis, 469 women enrolled in оncological gospital from 1 to 6 months and another 116 women received full treatment within a year (Table 2). Other women, for various reasons and due to the absence of any symptoms, allowed themselves to postpone the visit to the oncologist. Invalid is the direction of these patients accepted at least without surveys and stekloprokata, which recorded the defeat of the cervix. Repeated PAP smears may be negative. Moreover, 25% of women from this category arrived in onkological gospital, but was returned in the antenatal clinic with stekloprokata and laboratory "low surveys» to be negative.
Years |
The terms of the treatment of women with lesions HSIL |
|||||
|---|---|---|---|---|---|---|
Dо 10 Dн |
Up to 1 mon |
Dо 3 мес |
Up to 3-6 мес |
Dо 12 мес |
RWK not conducted |
|
2015 |
14 |
37 |
37 |
85 |
69 |
575 |
2016 |
25 |
46 |
46 |
138 |
47 |
513 |
Yust |
39 |
83 |
163 |
223 |
|
1 1088 |
Table 2 The terms of the treatment of women with lesions of HSIL to conduct mers in recent years
Moreover, 25% of women from this category arrived in onkological gospital, but was returned in the antenatal clinic with stekloprokata and laboratory "low surveys" (UAC, urine analysis, ECG, chest x-rays chest, blood tests for hepatitis RV), which causes extreme discomfort for women in connection with the remoteness of the territories, the increase in extent of pathological lesions and the failure of the timing of treatment. Interdisciplinary aspects of cancer control are crucial to its effectiveness. Continuous monitoring, rapid analysis and control is an integral part of anti - cancer activities. For the purpose of continuity onkological gospital with cytological laboratories of area, except the direction of women according to" minimum", now we are entered by the order of Department of health of area"signal cards" to be filled out and send to the within 10 days from the date of HSIL pathology, which allows monitoring the onkological gospital timeliness of their treatment and reducing the category of women not covered by treatment. Preliminary experience in the organization of screening for HPV-VCR (combining 2 tests of detection and quantification), associated with high risk, provide important additional information to the data of the PAP test for the prognosis of cervical cancer risk in women. Monitoring, operational analysis and control of treatment activities HSIL pathology is an integral part of the interdisciplinary aspects of screening aimed at reaching women, reducing morbidity and mortality from cervical cancer.
None.
The author declares no conflict of interest.

©2018 Cherenkov. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.