MOJ
eISSN: 2574-9935


Case Report Volume 4 Issue 1
1Metropolitan University of Santos - UNIMES, Brazil
2Radiology, WEBIMAGEM, Brazil
3Master degree in Evidence-Based Health, UNIFESP, Brazil
Correspondence: Márcio Luís Duarte, WEBIMAGEM, Avenida Marquês de São Vicente 446, São Paulo, São Paulo, Brazil
Received: February 03, 2020 | Published: March 31, 2020
Citation: Neto AN, Duarte ML, Gastaldi TND. Medial Tibial Stress Syndrome–Magnetic resonance imaging diagnosis in a sedentary person. MOJ Sports Med. 2020;4(1):24-25. DOI: 10.15406/mojsm.2020.04.00089
Medial tibial stress syndrome (MTSS) is one of the most common leg injuries in athletes who run. It's also the most frequent leg injury among militaries and athletes who jump, like basketball players and rhythmic gymnasts.
The gold standard for diagnosis is the history and the physical examination, the imaging methods are important to make the correct diagnosis and to distinguish the MTSS among the differential diagnosis. Imaging studies can help on the diagnosis of MTSS and the magnetic resonance imaging (MRI) is currently the most important method
This article aims to report an unusual case of MTSS diagnosed by MRI in a sedentary person.
Keywords: cumulative trauma disorders/diagnostic imaging, tibia/injuries, fractures, stress/diagnosis, magnetic resonance imaging
CT scan, computed tomography; MRI, Magnetic resonance imaging; MTSS, medial tibial stress syndrome
Medial tibial stress syndrome (MTSS) is a very usual leg lesion - represents 5% of all injuries in the physically active people; between 16% and 50% in select populations, like runners.1,2 MTSS accounts for 18% of musculoskeletal injuries and 60% of lower limb lesions.3 MTSS can be the main factor in restricting athletic performance due to the large rest duration of 16 weeks needed in critical circumstances.3
It´s a chronic disease provoked by repeated movements in sports, like running and jumping, and various risk agents have been proposed.2–4 MTSS has been defined as an overuse lesion or repetitive-stress damage of the tibia.4 Many stress reactions of the tibia and near musculature happen when the body is incapable to repair accurately in response to repeated muscle contractions and tibial strain.4
The risk factors can be categorized into:3,4
This article aims to report an unusual case of MTSS diagnosed by MRI in a sedentary person.
A 47 years-old man complains of pain in the anterior region of the left leg for 3 weeks. A physical examination shows pain on pain on palpation in the anterior portion of the leg. Points out that there is no movement limitation, but the pain worse with walking long distances. There is no change in the color of the skin ante there is mild edema in the anterior part of the leg. The patient denies trauma, surgeries and sports practices, previously.
The radiography was normal. Magnetic resonance imaging (MRI) demonstrates liquid effusion adjacent to the anterior aspect of the tibia with edema of the anterior subcutaneous tissue, edema of the cortical anterior bone of the tibia and a focus of edema in the bone marrow, compatible with medial tibial stress syndrome grade 2 according to Fredericson classification (Figure 1). The patient had a conservative treatment with cryotherapy and rest and, after four weeks, he was asymptomatic.
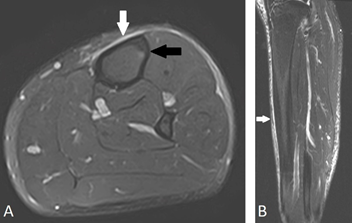
Figure 1 Left leg MRI in axial section in T2 FAT SAT sequence in A and sagittal section in T2 STIR sequence in B demonstrating liquid adjacent to the anterior aspect of the tibia with edema of the anterior and medial subcutaneous tissue (with arrow), edema of the cortical anterior bone of the tibia and a focus of edema in the bone marrow, compatible with medial tibial stress syndrome grade 2 according to Fredericson classification (black arrow).
Physical activity should produce pain throughout or following the exercise.5 MTSS diagnosis can be established when a recognizable pain is present on palpation of the posteromedial tibial margin for 5 cm or more.5 It must distinguish from chronic exertional compartment syndrome which is usually present throughout the exercise and suddenly reduces after exercise.5
The need for imaging investigations in the context of a precise history and physical examination has been doubted, but imaging tests are required when the concerning stress fracture is important.6 Radiographs are usually the primary level in the orthopedic imaging analysis; however, it can be normal – sometimes it demonstrates periosteal reaction or callus formation.6,7
Bone scintigraphy sensitivity in diagnosing MTSS is around 74% to 84%, but overdiagnosis and false-positive findings have been reported.6 CT scan has sensitivity of 42% and specificity of 100%.6
MRI is becoming a popular imaging test in cases of suspected MTSS, essentially because periosteal and bony edema are clearly seen – sensitivity is about 78% to 89%.6 It is the most precise test when the patient has symptoms and may help discriminate among MTSS and advanced stress fracture..6 According to Mann et al, with a 5 minute protocol MRI utilizing T2 FAT SAT sequence in axial section, there is no difference in diagnostic performance in detection and grading of tibial bone stress injuries amidst an abbreviated 5-min and a complete 25-min MRI test, with a substantial inter-reader agreement.7 In addition to the exam being faster, it is also cheaper.7
Fredericson classification for MTSS is an accurate method to connect the area of bone involvement with clinical manifestations, which leads to specific instructions for rehabilitation.6,8 The division of the Fredericson classification is described below:6,8
Presently, a consensus of adequate treatment alternatives for MTSS does not exist 2,5 Routinely prescribed treatments for MTSS include rest, ice, stretching, strengthening exercises, and orthotics, although none are effective as signs and symptoms commonly return with the restart of exercise.2 Reducing the load to 10% a week can be necessary to avoid (re-)injuries.5 While the 10% rule appears a reliable and valid guideline to expose athletes to developing loads, recent articles propose that changing load by up to 30% from week to week may be harmless.5,9
When pain continues notwithstanding the conservative treatment of MTSS, surgery is sometimes executed.5 Fasciotomy, either solely or in association with periosteal stripping, is the surgery performed, although high-quality evidence is lacking to justify clinical support.5
Not applicable
The authors declare that there is no conflict of interests regarding the publication of this paper.
The written informed consent of the patient was obtained, for the publication of her case.

©2020 Neto, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.