MOJ
eISSN: 2574-9935


Review Article Volume 7 Issue 1
1Universidad Santa Maria, Venezuela
2Universidad Gran Mariscal De Ayacucho, Venezuela
3Universidad Nacional Experimental Romulo Gallegos, Venezuela
Correspondence: Zulay Palima González, Universidad Nacional Experimental de los Llanos Centrales Rómulo Gallegos: San Juan de los Morros, Guárico, Venezuela
Received: February 13, 2024 | Published: February 28, 2024
Citation: Jessika MM, Alberto MBC, González ZP. Current state of conventional vertical bone regeneration vs with titanium occlusive barriers- literature review. MOJ Sports Med. 2024;7(1):15-20. DOI: 10.15406/mojsm.2024.07.00156
Introduction: The alveolar bone is part of a specialized structure of the bones of the face, specifically the maxilla and mandible, this being the main support for the teeth, which is composed of cortical bones that form the vestibular and palatine walls and lingual. It is also made up of spongy bone, within it there are numerous medullary perforations, being smaller in the cortex. The alveolus is subject to continuous changes that are produced by dental eruption, chewing and a variety of periodontal diseases that can influence its constant remodeling.
Materials and methods: An electronic search was carried out to provide support and justification for this literature review. This bibliographic search was carried out in the Pubmed / Medline, Science Direct and Scielo databases of scientific articles published in English, which had the objective of describing the bone remodeling processes that occur in the alveolar bone after dental loss and the possible treatments for vertical bone regeneration that can be provided to the patient for the subsequent placement of the dental implant.
Results: Of the different conventional vertical bone augmentation techniques described in the literature over the years, CAD/CAM titanium meshes are the ones that present the highest percentage of gain. Likewise, greater bone gain was observed combined with collagen membranes than without them. Distraction osteogenesis presented a lower percentage of gain, followed by guided bone regeneration with non-resorbable membrane and, finally, the onlay or bone block graft technique. However, with the recent appearance of titanium occlusive barriers, the literature reports the highest percentage of gain.
Conclusions: Regarding complications, we can conclude that distraction osteogenesis and block bone grafts are those that obtained the highest complication rate, followed by CAD/CAM titanium meshes and non-resorbable membranes.
Keywords: bone, bone defects, vertical bone regeneration, biomaterials for bone regenerations, absorbable membranes
Phases of bone remodeling
Bone density
In 1985, Lekholm and Zarb7 in their study described four types of bone qualities that we can find in both the maxilla and the mandible, these being:
-Type 1 quality: it is mostly composed of homogeneous cortical bone with a small core of trabecular bone.
-Type 2 quality: composed of a large layer of dense cortical bone that surrounds a core of dense trabecular bone.
-Type 3 quality: it is made up of a thin layer of cortical bone that surrounds a trabecular bone of favorable resistance.
-Type 4 quality: it is mostly composed of spongy bone that is surrounded by a thin layer of cortical bone (Figure 1).
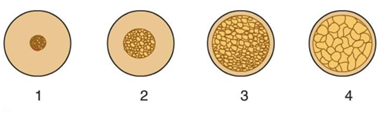
Figure 1 Scheme of bone qualities according to Lekhonlm and Zarb, 1985.7
Types of bone defects
In 1985, Misch and Judy.8 developed four basic categories to determine the availability of bone in the use of dental implantology in both the maxilla and the mandible, following the natural resorption phenomena in each region. They also included both bone angulation and crown height for each bone volume, as they affect prosthetic treatment. Years later, they added two subcategories in order to provide a focus for the different implant treatment options, such as bone grafts and future prostheses (Figure 2).
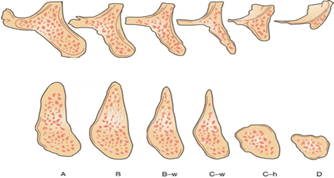
Figure 2 Classification of alveolar bone defects according to Misch and Judy, 1985.8
The categories to determine the available bone are the following:
There are three possible treatments for this type of division:
In this division the following treatment options are proposed:
In this division the following treatments are suggested:
In 1985, Lekholm and Zarb7 published a classification based on the degree of ridge atrophy related to the insertion of Branemark devices. This classification consists of 5 morphologies, according to "Practical Techniques in Periodontics and Implant Dentistry", Wiley, 2022.
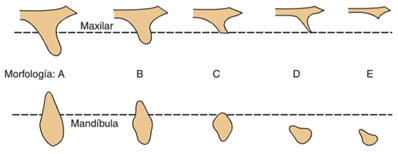
Figure 3 Classification of alveolar bone defects according to Lekholm and Zarb, 1985.7
Hom-lay Wang in 2002,9 proposed a new classification of bone defects based on the Seiberts classification with some modifications, both soft and hard tissue defects were included in this scheme with their respective treatment option. Seibert's three categories are still present, but with the use of simpler terminology, which classifies them into class I (horizontal), class II (vertical) and combined defects, subdividing in turn into small ones (s, ≤ 3 mm ), medium (m, 4 to 6 mm) and large (l, ≥ 7 mm).
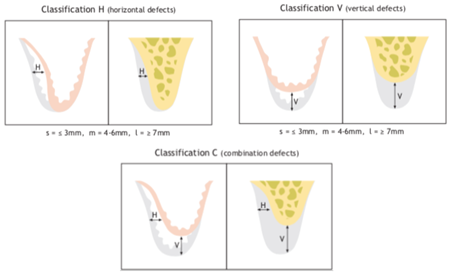
Figure 4 Classification of alveolar defects according to Hom-lay Wang, 2002.9
Chiapasco in 2018,10 is based on the concept of “implant placement driven by prosthetic restoration” optimizing both the function and aesthetics of the patient, for which it publishes an article based on evidence and oriented to future restoration, in turn describes in detail a diagnostic protocol, classification of bone defects and the main augmentation techniques.
One of the general rules when performing a restoration on implants is that viability must first be verified from a prosthetic point of view. As a diagnostic method we can use plaster molds and a wax-up, since it will allow us to recognize discrepancies or asymmetries of the edentulous ridges. If we are only going to restore one hemiarch, the contralateral side should be taken as a reference, both to evaluate the alveolar crest and dental morphology. On the other hand, a Cone Beam Computed Tomography (CBCT) should be performed in conjunction with facial and intraoral clinical photographs, since they are a very important tool when defining the appropriate treatment plan for the patient.
Once the bone defect has been identified, it must be analyzed whether the bone volume is adequate for the placement of the prosthetically guided implant, or whether it is necessary to perform a graft procedure.
Classification of bone defects according to a prosthetic diagnostic protocol and its various surgical treatment options:
The main surgical techniques for the correction of deficits in this class are:
After having performed the ROG, you should wait approximately 4 to 9 months (depending on the type of treatment selected) for the subsequent placement of the implant.
The main surgical techniques for combined defects are according to “Paolo Casentini" Horizontal bone-augmentation procedures in implant dentistry: prosthetically guided regeneration", Periodontology 2000, 201”

Figure 5 Classification of bone defects according to Chiapasco, 2018.10
Guided bone regeneration
ROG can be described as a surgical procedure that allows us to increase the alveolar bone when it is deformed due to tooth loss, periodontal diseases or consequences of trauma, reasons for which it can cause a reduction in both vertical and horizontal dimensions which prevents us from correctly placing dental implants. As we know, alveolar regeneration is a unique event since the site previously occupied by dental roots does not have bone, and for bone to form a series of events must arise that begin with the deposition of a provisional matrix of connective tissue that Finally, it is replaced by bone tissue and then by lamellar bone. One of the most used substitutes when a dental organ is lost is usually osseointegrated implants, which provide us with both the lost facial aesthetics and the chewing function, therefore, ROG techniques are indicated as long as the patient needs them and there is no possibility of placing short implants.11
ROG techniques can be performed in one surgical phase, which would involve the simultaneous placement of the implants and bone augmentation, or in two surgical phases, first performing the bone augmentation, and then, after a few months, the placement of the implants.12 In this second phase, it must be taken into account that the thickness of the vestibular cortex must be at least 2 mm, to guarantee stability of the peri-implant soft tissues. For the success of these procedures, a membrane must be used to act as a barrier to prevent soft tissue migration before osteogenic cells begin to form and at the same time seal the gap to develop new bone matrices. “Alberto Monje "Guided Bone Regeneration in Alveolar Bone Reconstruction", Oral and Maxillofacial Surgery Clinics of North America, 2019”
On the other hand, the literature supports that in certain cases in which there is not the adequate amount of bone for the correct placement of the implants, surgical techniques can be used, such as grafts in intraoral blocks obtained from the residual ridge, the symphysis mandibular and the mandibular body or branch, or extraoral, coming from the iliac crest and tibia, for the reconstruction of said defects.13
After the extraction of a tooth, whether due to trauma, cysts, tumors or advanced periodontal disease, the alveolar bone undergoes dimensional changes that can be detrimental to the placement of dental implants in the correct position, compromising their future rehabilitation. These changes can occur horizontally, vertically or in combination, with the posterior area of the mandible and maxilla being the most affected areas, since the bone is resorbed more quickly than in the anterior area. Different authors have developed various classifications regarding jaw atrophy, based on the quantity and quality of bone available.14
One of the biggest clinical challenges today is vertical bone regeneration, for which there are various procedures prior to therapy with dental implants.15 Chiapasco and Casentini in 2018,10 conducted a study based on the concept of “implant placement driven by prosthetic restoratio, in which they described in detail a diagnostic protocol for the classification of bone atrophies and the main vertical bone augmentation techniques. Bone regeneration with non-resorbable membranes, distraction osteogenesis, onlay graft or block graft or Le Fort osteotomy. In turn, Scavia et al., in their 2021 study, proposed a new ROG technique with d-PTFE, in pocket, obtaining encouraging results, with a bone increase of 8.78 mm, being similar to the average reported in the literature.
Likewise, Wang et al. determined that for these procedures to achieve their objective, 4 biological principles must be met: primary closure, angiogenesis, creation and maintenance of space, and clot stability. Alveolar ridges with severe bone deficits and inadequate soft tissue volume present difficulties for stability of the grafted material and primary closure.16
Numerous comparative studies have been carried out that assess the effectiveness of the different biomaterials used for bone augmentation, with autogenous bone being the material of choice, despite the morbidity and possible complications of the donor site.
The growth of soft tissue is faster than the formation of bone tissue, so the membranes act as a barrier preventing the migration of soft tissue to the area we want to regenerate.17
Likewise, it is known that membrane exposure compromises the effectiveness of the ROG. Chiapasco and Zaniboni,18 described in their 2006 comparative study that 20% of the e-PTFE membranes presented exposures and infections, with a coverage of 63 to 100% despite their exposure, while the collagen membranes presented a 95% coverage.
Recently, the possibility of performing vertical bone regeneration procedures with a subperiosteal barrier membrane without the need to use any type of biomaterial has been studied, since it provides a stable blood clot that transforms into bone tissue.19
They observed that the same amount of bone formed under fully airtight occlusive membranes compared to semipermeable membranes. It has also been shown that these barriers have osteoconductive properties. However, Lundgren in 1998 conducted a comparative study in rats, in which he used totally occlusive versus perforated barriers to evaluate the composition and quality of the tissue formed over time. They reported that the quality of bone obtained was better in the case of totally impermeable barriers than in semipermeable ones. Other authors, such as Perret carried out a series of cases in which they evaluated the bone changes obtained after the placement of a titanium barrier to achieve bone regeneration, obtaining a vertical bone gain of 7mm in the vestibular and 4mm in the lingual, stating that the use of occlusive barriers without primary closure are successful in alveolar reconstruction.20
Table of the different vertical bone regeneration techniques
Comparative table of the different vertical bone regeneration techniques in terms of bone gain and the percentage of complications of the different existing procedures (Table 1).
|
Author |
Magazine |
Year |
Study |
Technique |
Gain in mm |
Complication in % |
|
Chiapasco |
Clin. Oral. Imp. Res. |
2021 |
Retrospective clinical study. |
CAD/CAM titanium mesh. |
8.9mm |
/ |
|
Cucchi |
Clin. Oral. Imp. Res. |
2021 |
Clinical trial. |
CAD/CAM titanium mesh. |
/ |
Membrane 13% Without membrane 33% |
|
Urban |
Clin. Oral. Imp. Res. |
2021 |
Multivariate analysis. |
ROG with d-PTFE. |
5.2mm |
3% |
|
Scavia |
J. Contemp. Dent. Pract. |
2021 |
Preliminary results. |
ROG with d-PTFE. |
8.78mm |
/ |
|
Urban |
J. Clinical Periodontology. |
2019 |
Systematic review and meta-analysis. |
ROG with e-PTFE. |
4.31mm |
12.1% |
|
Urban |
J. Clinical Periodontology. |
2019 |
Systematic review and meta-analysis. |
ROG with d-PTFE. |
4.99mm |
12.1% |
|
Urban |
J. Clinical Periodontology. |
2019 |
Systematic review and meta-analysis. |
Distraction osteogenesis. |
8.4mm |
47.3% |
|
Urban |
J. Clinical Periodontology. |
2019 |
Systematic review and meta-analysis. |
Block graft. |
3.46mm |
23.9% |
|
Brigulio |
Inter. J. of Dentistry. |
2019 |
Systematic review. |
ROG with titanium meshes |
12.4±3.1mm |
34.8% |
|
Elnayef |
The Int. J. of Oral Maxillofacial Impl. |
2017 |
Systematic review and meta-analysis. |
ROG |
3.83mm |
Infection 5.8-31.8% Dehiscence 8-27% |
|
Elnayef |
The Int. J. of Oral Maxillofacial Impl. |
2017 |
Systematic review and meta-analysis. |
Distraction osteogenesis. |
6.8mm |
Infection 8-57% Elimination of the distractor 6.8-18% |
|
Elnayef |
The Int. J. of Oral Maxillofacial Impl. |
2017 |
Systematic review and meta-analysis. |
Block inlay graft. |
4.92mm |
Infection 10-20% Dehiscence 8-30% |
|
Elnayef |
The Int. J. of Oral Maxillofacial Impl. |
2017 |
Systematic review and meta-analysis. |
Onlay block graft. |
3.47mm |
Infection 10-16% Dehiscence 3.8- 45.8% |
|
Yun |
The Int. J of Oral and Maxillofacial Impl. |
2016 |
Systematic review and meta-analysis. |
Distraction osteogenesis. |
7.65mm |
/ |
|
Yun |
The Int. J of Oral and Maxillofacial Impl. |
2016 |
Systematic review and meta-analysis. |
Onlay bone graft. |
5.83mm |
/ |
|
Van Steenberghe |
Clin. Oral. Impl. Beef. |
2003 |
Clinical trial. |
Occlusive barriers. |
16mm |
20% |
Table 1 Representative analysis of the different vertical bone regeneration techniques, indicating their bone gain and their percentages of complications
Regarding the vertical regeneration procedure with completely hermetic titanium occlusive membranes, Van Steenberghe conducted a clinical trial describing a bone gain of 16 mm without the need for bone grafting.
Taking into account the studies analyzed, the average bone gain between the different types of conventional vertical regenerations is 6.85 mm. In the case of occlusive barriers, the bone gain described is 16 mm. However, more long-term studies are needed to confirm the success rate of implants placed in regenerated bone with occlusive barriers.21
There are various techniques for vertical bone augmentation such as: guided bone regeneration with non-resorbable membranes, distraction osteogenesis, block bone grafts, le fort I, personalized CAD/CAM titanium meshes and bone regeneration with titanium occlusive barriers.
Conventional techniques obtained an average bone gain of 6.85 mm and occlusive membranes of 16 mm. Despite the limitations of this bibliographic review, vertical bone regeneration with titanium occlusive membranes is a promising technique, and although, using other techniques, the percentage of complications is high, with this technique it can be reduced. However, long-term studies of regeneration with the occlusive barrier technique are needed and long-term studies are needed to assess the success rate of implants placed in this regenerated bone.
None.
The author declares that there are no conflicts of interest.

©2024 Jessika, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.