MOJ
eISSN: 2374-6939


Case Report Volume 12 Issue 5
1Department of Orthopedic Surgery and Traumatology, Hospital Universitario Doctor Peset, Spain
2Department of Orthopedic Surgery and Traumatology, Hospital Intermutual de Levante, Spain
Correspondence: Jesús García Álvarez, Orthopedic Surgery and Traumatology Department, Hospital Universitario Doctor Peset, Av. Gaspar Aguilar, 90. 46017, Valencia, Spain, Tel +34 627 744 066
Received: September 10, 2020 | Published: October 30, 2020
Citation: Álvarez JG, Ortiz SP, Tomás JMP. Sciatic nerve dependent schwannoma. MOJ Orthop Rheumatol. 2020;12(5):100-102. DOI: 10.15406/mojor.2020.12.00528
Schwannoma is a tumor composed of Schwann cells. This is the most common benign tumor of the peripheral nerve sheath, representing the 8% of all soft tissue tumors, affecting the sciatic nerve in less than 1% of cases. Due to its location in the nerve sheath, these types of tumors produce symptoms related to nerve function and compression of adjacent structures. Diagnosis is made by magnetic resonance and is confirmed by pathological anatomy, often after screening of radicular pathology with normal magnetic resonance and symptomatology compatible with clinical sciatica.
We report the case of a 53-year-old woman with a tumor in the posterior area of the right thigh of one year of evolution. After the examination and the appropriate complementary tests, she was diagnosed with schwannoma of the peripheral sheath of the right sciatic nerve. The patient underwent surgery for tumor exeresis with satisfactory results and acceptable aftermath.
Keywords: tumor, schwannoma, sciatica, sciatic nerve
MR, magnetic resonance; PA, pathological anatomy; CT,computed tomography; EMG,electromyogram
Pain with radicular characteristics is one of the most frequently consulted pathologies in traumatology services, especially pain at the level of the roots that correspond to the sciatic nerve. Although the main cause of this problem is the discopathy that produces compression of the nerve root, there are other pathologies that, although less frequent, we must take into account, such as injuries that affect the peripheral nerve.
We report the case of a patient with radicular type pain in the territory of the sciatic nerve with normal lumbar magnetic resonance. We emphasize the importance of a correct physical examination, and the extension of the study beyond the proximal zone of the nerve root when the most common pathologies are ruled out.
We report the case of a 53-year-old Caucasian female patient who came to our center with a palpable tumor in the posterior area of the right thigh with a year of progressive growth, that she relates it to overexertion.
A tumor was palpated in the upper third of the posterior face of the right thigh of approximately 3x5cm with hard consistency, adhered to deep tissues, without alterations in the overlying skin and neither vascular nor nervous compromise. She referred spreading pain to the right lower limb and provided recent lumbar magnetic resonance (MR) without pathological findings.
Ultrasound test was requested and revealed a solid mass with well-defined borders, hypoechoic, heterogeneous, with cystic areas, measuring 33x40x55mm. It was located in the muscular compartment of the biceps femoris with vascularization inside.
We completed the study with MR that reported an ovoid lesion of heterogeneous structure and cystic areas inside, with measurements of 37x33x69mm with well-defined borders, maintaining a fatty plane of separation with muscles (signs of non-aggressive lesion), without contrast highlights or signal intensity changes of the muscles adjacent to the lesion (Figure 1). It contacted and displaced the sciatic nerve medially, depending on one of the fascicles of the nerve. With contrast administration, the absorption was progressive, obtaining low-medium values respect to the arterial peak, being compatible with a nervous sheath tumor.
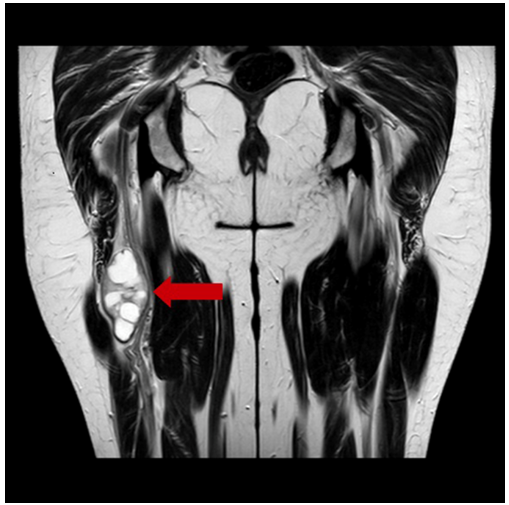
Figure 1 MR of the lower extremities without contrast, coronal cut: ovoid lesion of heterogeneous structure and dependent areas of one of the fascicles of the sciatic nerve (arrow).
To confirm the diagnosis, a percutaneous biopsy was performed with trucut. The pathological anatomy (PA) report concluded a neural mesenchymal neoplasm (strong and diffuse positivity for S-100 protein) without signs of malignancy, being compatible with a benign tumor of the peripheral nerve sheath (schwannoma) of the right sciatic nerve.
A complete study was requested that consisted in thoracic, abdominal and pelvic computed tomography (CT) with contrast administration that ruled out systemic extension.
The patient underwent surgery for the exeresis of the tumor. In our case, infragluteal approach was used, pulling away biceps femoris and adductor magnus muscles until the nerve was isolated by plane dissection and neurovascular structures were referenced (Figure 2).
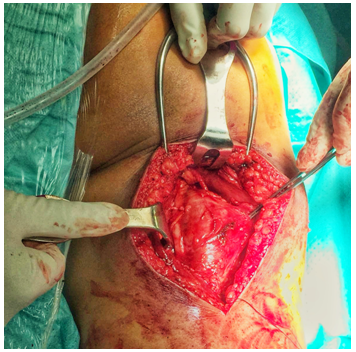
Figure 2 Intraoperative image: nodular tumor with whitish coloration, adjacent to the sciatic nerve in its most cranial portion of the right thigh.
A nodular and whitish-colored tumor was observed next to the sciatic nerve in its most cranial portion of the right thigh. The longitudinal dissection of the peripheral sciatic nerve sheath was performed for complete tumor resection, which was sent to the PA for histological study (Figure 3). The absence of lesion was verified in the proximal and distal ends of the nerve, trying to preserve as many viable nerve fibers as possible.
The PA report showed the presence of nodular tissue of mucinous content and with cystic and hemorrhagic areas, without evidence of malignancy, compatible with the diagnosis of schwannoma.In a postoperative re-evaluation of the functional capacity of the operated limb, parenthesis were observed in the dorsal and lateral face of the leg and foot, besides inability to extend the fingers and to flex dorsally the foot. An electromyogram (EMG) was requested to verify the degree of nerve damage, which showed a damage of 95% of the nerve fibers corresponding to the external popliteal sciatic nerve (EPS) o fibularis communis nerve.
Collaboration was made to the rehabilitation service of our center to design a personal program that allows to reduce the aftermaths to the minimum. Currently, she is carrying out this program.
Schwannoma is a benign tumor derived from the neural sheath of Schwann cells, usually solitary and with a misleading clinical presentation, similar to a radiculopathy and often confused with another radicular pathology. These tumors appear more frequently around the fourth decade of life (63% between 30 and 59 years), being infrequent in children. They present the same distribution by gender.1–5
They present a typical growth along the path of a nervous trunk, growing eccentrically to the nerve, not including its bundles. This fact makes the difference with neurofibroma, giving the schwannoma a different treatment and a much more favorable prognosis. This tumor appears more frequently in the upper limbs, affecting the median nerve, radial nerve and ulnar nerve in 20% of cases.6–8
They usually have a misleading clinical presentation, mainly due to a long subclinical course. When they cause symptoms, their most frequent presentation simulate radiculopathy, with sensory alterations, being motor loss a less common presentation, so that it is often confused with other nerve root pathologies, secondary to degenerative problems of the spine. A radicular pain with a long period of evolution, which does not respond to anti-inflammatory treatment and rest, and the lack of a physical examination and imaging tests that are compatible with lumbar pathology, should make us think about peripheral nervous pathology. The palpation of the tumor is usually difficult in many cases due to its location and, if the palpation is possible, indicates a long period of evolution.9–19
The diagnosis is usually evident by optical microscopy, although confirmation by immunohistochemical techniques may be useful. It presents two different histological types that may coincide in the same tumor: Antoni type A, with a high density of fusiform cells organized in palisade-shaped; and type B, which presents a pattern of lower cellularity with amorphous material between them. These types of tumors have a strong positivity for the S-100 protein.20,21
Despite being benign, some cases of malignant degeneration have been described (less than 0.001%, depending on the series) and especially in cases associated with neurofibromatosis type 1.22,23
Its gold standard treatment is the marginal resection of the tumor, preserving the anatomy and functionality of the nerve. This is possible in the case of schwannomas, which grow eccentrically to the tumor, but not in the case of neurofibromas that require much more aggressive surgery. Recurrence is infrequent after tumor excision.24,25
In summary, schwannomas are benign tumors with insidious clinical presentation, which makes their diagnosis difficult. We must think about them when faced with a patient with clinical symptoms similar to a radicular pathology, but with physical examination and complementary tests not compatible with this pathology. An early surgical treatment is very important, in order to avoid the possible aftermaths that can cause the compression of neighboring structures and to rule out another tumor with a worse prognosis than schwannoma.
None.
The authors declare there are no conflicts of interest.
None.

©2020 Álvarez, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.