MOJ
eISSN: 2374-6939


Research Article Volume 11 Issue 3
1Scientific Committee of the Mexican Hip Fracture Audit
10Centro de Investigación Ósea, Guadalajara
11Hospital General de Tijuana, Tijuana, Baja California
2Hospital Regional del ISSSTE León, Guanajuato
3Hospital Ángeles Puebla, Puebla
4Hospital Regional PEMEX, Reynosa, Tamaulipas
5Hospital San Francisco de Asis, Guadalajara, Jalisco
6Hospital General de Zona 58 IMSS, León, Guanajuato
7Instituto Nacional de Rehabilitación, Ciudad de México
8Hospital General de Zona 21, León, Guanajuato
9Escuela Nacional de Estudios Superiores Unidad León, Universidad Nacional Autónoma de México
Correspondence: Juan Carlos Viveros G, Geriatría, Medicina Interna, Scientific Committee of the Mexican Registry of Hip Fracture, Mexico
Received: April 29, 2019 | Published: May 2, 2019
Citation: Viveros-García JC, Robles-Almaguer E, Albrecht-Junghanns RE, et al. Mexican Hip Fracture Audit (ReMexFC): objectives and methodology. MOJ Orthop Rheumatol. 2019;11(3):115-118. DOI: 10.15406/mojor.2019.11.00483
Introduction: Hip fracture (HR) is a public health problem with high morbidity and mortality. In other countries, national FC records have been made. England launched the National Hip Fracture Database (NHFD) which has registered 30,000 cases. They were followed by Norway, Australia, New Zealand and Spain. These records have helped to measure quality indicators, care outcomes and decrease mortality.
Justification: In Mexico there is no national registry on the characteristics of hip fracture.
General Objective: To know the demographic characteristics, assistance, adherence to quality indicators and postoperative results in Mexican patients with fracture of hip due to fragility in Mexico.
Methodology: Observational, epidemiological, descriptive, multi-center study in different hospital centers of the Mexican Republic. The data suggested by the Fragility Fracture Network (FFN) will be measured, including sociodemographic characteristics, cognitive and functional status prior to fracture, quality indicators and a 30-day follow-up. Re-entry and reoperation will be documented, as well as mortality in the acute phase and at 30 days. The information will be analyzed with SPSS of IBPM version 20.0.
Keywords: hip fracture, registration
In Mexico 1 out of every 4 adults is suffering from osteopenia or osteoporosis,1 the most serious consequence of which is hip fracture (HR). It is estimated that between 8.5% and 18% of women will have a hip fracture throughout their lives.2,3 In Mexico City, an incidence of 1 725 cases in women and 1 297 men per 100 000 inhabitants has been reported, and it is believed that it will increase by at least 7 times by 2050.4
Hip fracture has been considered a public health problem due to its high impact on morbidity, mortality, dependence and costs.5–7 Mortality at one year is usually 25%, and of these only 10% die in the acute phase.8–12 On the other hand, only 73% of patients recovered the mobility they had prior to the fracture,9 which increases the risk of dependence.12
In addition to the welfare consequences, the costs of FC also make it a catastrophic entity.7,13–15 In 2002, the Mexican Institute of Social Security (IMSS) spent close to 1 927 072 United States Dollars (USD) on care in the acute phase of FC,6 with an average cost per event, up to 12 thousand US dollars. Despite this complex scenario, in Mexico there is currently no multicenter study or registry on the sociodemographic and assistance characteristics of hip fracture. Most of the work has been done in Mexico City, in a single center, so it is not possible to have a global vision of this problem. In other countries in recent years, many efforts have been made to study FC and try to improve its prognosis, increase the quality of care and reduce hospital costs. This through clinical practice guidelines, implementation of multidisciplinary teams, inclusion of the geriatrician in the care from the acute phase and the formation of Orthogeriatric units,15–17 in addition to the publication of recommendations and quality indicators in the care.18,19
Another tool that has been used to try to improve FC care is the regional and national registers. In 2007, the National Hip Fracture Database20 was launched in England, which has so far recorded nearly 30,000 hip fractures. Other countries have followed Norway,21 Australia and New Zealand,22 Scotland23 and recently Spain.24
These records have proven to be useful for situational diagnosis, as well as to improve adherence to quality indicators. After the implementation of the NHFD it was possible to reduce the surgical delay, reaching the goal of surgery in 48 hours or less in 71% of the cases. This impacted on a decrease in mortality in the acute phase. It was also possible to reduce the hospital stay and increase the participation of geriatricians in phase25 care.
Justification
There is not a multicentric, regional or national registry of Fractures of the Hip due to frailty. This registry will allow a situational diagnosis on this important public health problem, as well as measuring the quality indicators and comparing them among the participating hospitals, and later, in a second time, comparing ourselves with other countries in the world. This will facilitate the detection of opportunity points and generate policies that help us improve the prognosis of patients with hip fracture in Mexico.
Goals
An observational, cross-sectional, epidemiological, descriptive, multicenter study will be carried out in different hospital centers of the Mexican Republic. An invitation will be made to participate to subinvestigators interested in the hip fracture care of the specialty areas: Traumatology, Internal Medicine, Geriatrics, Rheumatology and related specialties.
An informed consent will be obtained from each patient to be included in the registry, which will be stored in said center and will be subsequently collected digitally. The suggested variables in the Common Database (Minimun Common Dataset) will be documented by the Fragility Fracture Network "FFN" (Fragility Fracture Network), which is a non-profit Academic Institution are headquartered in Switzerland and global representation, dedicated to the global optimization of the multidisciplinary management of fragility fractures (Figure 1) (Table 1).
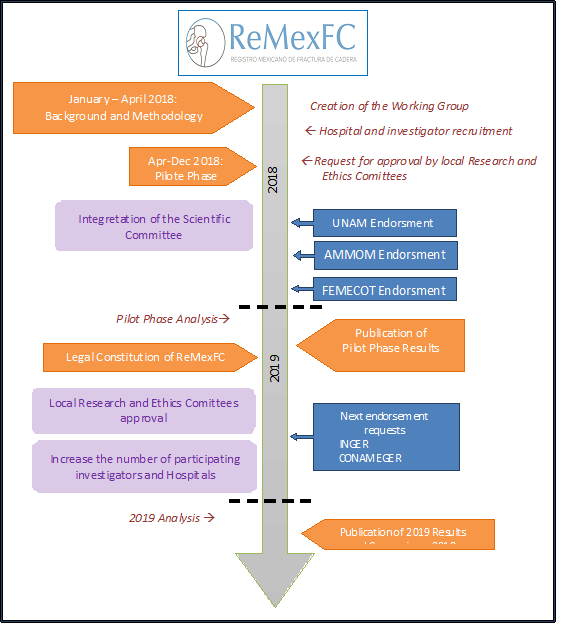
Figure 1 ReMexFC Timeline.
ReMexFC, Registro Mexicano de Fractura de Cadera; UNAM, Universidad Nacional Autónoma de México; FEMECO, Federación Mexicana de Colegios de Ortopedia y Traumatología; INGER, Instituto Nacional de Geriatría; CONAMEGER, Colegio Nacional de Medicina Geriátrica; FFN, Fragility Fracture Network.
|
In-Hospital Acute Phase and 30 days Followup
|
|
|
Patient
-Informed Consent -Gender -Age -City and Provice -Name of The Hospital -Public of Private Care |
Baseline Characteristics
-Residence (Home or Long Term Care) -Gait evaluation -Walking aids -Cognition -Side -Type of fracture -Osteoporosis treament -Functional Status -Sore Ulcers -Delirium |
|
Acute Care
-Date and Time of arrival to ER ¥ -Date and time of arrival to trauma ward -Date and time of surgery -Tipe of Surgery -Surgical delay -Cause of surgical delay -type of Antesthesic technique -Femoral blocking -Sore Ulcer -Delirium -Multidisciplinary team -Sitting after surgery -In hospital weightbearing
|
Discharge
-Discharged to long care or home -Date of discharge -Length of stay -Osteoporosis treatment -In-Hospital Mortality
|
|
30 Days Follow-up
-Mortality -Readmission -Surgical Reoperation -Gait evaluation -Walking aid -Functional status -Osteoporosis treatment
|
|
Table 1 Adaptation for México of the Minimmun Common Dataset
¥ ER, Emergency Room
These variables include sociodemographic characteristics prior to the fracture, cognitive and functional status prior to the fracture, as well as their admission to the emergency department, surgical phase, rehabilitation, patient's condition at discharge, management of osteoporosis and follow-up by telephone or in person at 30 days. In addition, re-admission to the hospital and the requirement for surgical re-intervention will be assessed. Mortality will be measured from the acute phase considering whether it was before, after surgery or within 30 days after discharge.
Each center will collect individually the informed consents, the capture sheets and will be responsible for uploading the data of each patient on a bi-monthly basis to the platform. Once sent, the data will be concentrated in a global database, where the personnel that analyze the data generates a blind for the analysis of information.
Histograms of each variable will be reported with the name of the hospital blinded, marking the national average and, on the other hand, the quality indicator suggested by international standards. These reports will be generated quarterly, exclusively to the participating centers. Subsequently, an annual report will be made, which will be published.
Due to the great extension of the Mexican Republic, regional coordinators will be created with the purpose of continuing adding centers to the registry, as well as to solve doubts in the process of capturing patients, filling in the platform for sending the information.
A scientific committee will be created for the periodic analysis of the variables to be measured, and the resolution of said commission will be communicated to the rest of the subinvestigators. The activities carried out in 2018 and 2019 are shown, including the scientific societies that have so far endorsed the project, as well as those that will be requested in the future in Figure 1. The information will be analyzed with the SPSS package of IBPM version 20.0.
To the coordinators of The Spanish National Hip Fracture Registry for their support and counsling.
The author(s) declares that there is no conflict of interest.

©2019 Viveros-García, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.