MOJ
eISSN: 2374-6939


Research Article Volume 12 Issue 5
1Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof, Russian Ilizarov Scientific Centre, Russia
2Professor, Bari-Ilizarov Orthopaedic Centre, Bangladesh
3Medical officer, Bari-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Mofakhkharul Bari, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Professor, Russian Ilizarov Scientific Centre, Kurgan, Bari-Ilizarov Orthopaedic Centre, 1/1, Block#E, Suvastu Shirazi Square, Lalmatia, Dhaka-1207, Bangladesh, Tel +88 01819 211595
Received: September 12, 2020 | Published: October 8, 2020
Citation: Bari MM, Shahidul I, Shayan BAMR. Ilizarov hip reconstruction (hybrid transosseous Osteo-synthesis technique creating femoral support to acetabulum and correcting biomechanical limb axis in proximal femoral defect). MOJ Orthop Rheumatol. 2020;12(5):96-98. DOI: 10.15406/mojor.2020.12.00527
Defects of the proximal femur and technique for femoral reconstruction, support restoration and limb length were used depending on localization of defects and anatomical and functional components of the pathology. Children, adolescents and young adults with late sequelae of neonatal hip sepsis1,2 or hip dislocation from dysplasia present with problems of pain, Trendelenburg gait, limb length discrepancy and hip instability related to absence of part or all of the femoral head and neck and proximal migration of the femur.
Keywords: proximal femoral defects, valgus and varus osteotomy, ilizarov technique
Reconstructive surgeries for the proximal femur were performed in 16 patients with defects of head 8, defects of head and neck 4 and neglected DDH 4 from January 2004 to January 2018.
Pathological symptomatic complex was characterized by the following features which determined severity of anatomical and functional disorders:4,5
Evaluation of gait, leg length and range of motion is very important for surgical intervention. A Trendelenburg sign confirms the weakness of the hip. Range of motion of the hip (flexion, abduction, adduction, external rotation and internal rotation in both supine and prone positions) should be carefully recorded. Flail hip is the best candidate for Ilizarov hip reconstruction.3,6,7 The patient’s ability to adduct the hip combined with weakness of hip abduction strength is a verykey contributing factor to the Trendelenburg gait. With Ilizarov hip reconstruction greater ability of abduction of hip ensues. With Ilizarov hip reconstruction extension at the proximal osteotomy helps the patient lock the hip into extension during gait. LLD and limb deformity should be noted by looking the legs, iliac crest and back exposed.3 Blocks should be placed under the affected leg until the pelvis becomes level and the back looks straight. It will give a good estimate of total LLD. Trendelenburg gait is one of the hallmarks of this disease. Ilizarov hip reconstruction is very effective in eliminating Trendelenburg gait and sign in these patients. No other treatment option except arthrodesis has been able to address this aspect of the problem. Unstable mobile hip is absolutely indicated for Ilizarov hip reconstruction and simultaneously we can correct limb length discrepancy and effective in eliminating Trendelenburg gait.8,9
Hybrid Transosseous osteosynthesis technique involves a proximal femoral osteotomy for valgus and extension and a distal femoral osteotomy for lengthening and limb realignment. The level ofthe proximal femoral osteotomy was determined from the maximum adduction anteroposterior cross-legged radiograph of the pelvis. The affected lower limb and hip are maximally adductedover the normal side. The osteotomy was performed at the level at which the femoral shaft crossed the ischium. The amount of valgus angulation at the proximal osteotomy was determined byadding 15 degree to the femoropelvic adduction measured on the anteroposterior standing radio- graph of the affected side rather than the maximum adduction anteroposterior radiograph of the pelvis. The overcorrection of 15 degree was determined based on experience and was used to compensate for fatigue of the abductor muscles. As the hip is maximally adducted, external rotation of the femur occurs. This amount of external rotation of the hip is corrected with internal rotation at the proximal femoral osteotomy site. Our goal of the distal femoral osteotomy is to lengthen and realign the lower extremity.10
The patient was laid on the operating table with the limb maximally adducted and slightly flexed to 10 degree. Two 5,5mm Schanz were placed at different planes in greater trochanter and fixed to an arch mounted at an angle to 135 to 140 degree to the longitudinal axis of the segment, which was open outwards. Three crossing wires were inserted in the upper third of the femoral shaft and fixed to an arch tilted in reverse direction and placed with hypercorrection of 15 degree to the longitudinal axis of the segment forming an angle open laterally posteriorly. Three to four wires were driven in the distal metaphysis and fixed to a ring. Now subtrochanteric osteotomy of the femur was performed out of the lateral incision of 2 to 3cm using grooved chisel with the convexity turned up. Then the extremity was abducted and maximally extended forming an angle between the fragments ends, the angle was open laterally and posteriorly; support to acetabulum was produced with the end of the distal fragment and partially with the proximal fragment. The arches were connected by threaded rods; and we checked up how good was the support by adducting the limb slowly and pressing along the axis. Then we performed corticotomy in the proximal shaft out of incision of 1cm to 2cm, which was more distally than subtrochanteric osteotomy; the lower third of the femur was corticotomize in concomitant valgus of the knee. The distal arch and the ring were connected by 3 to 4 telescopic rods with uniplane hinges placed at the corticotomy level. Radiographically we checked every 14 days. Gradual distraction was started on 5th post-operative day along the telescopic rods until the leg length discrepancy was eliminated and biomechanical axis normalized.8 Correction was done until the Centre’s of the major bearing joints of the femur were placed in one axis; and the space of the knee was perpendicular to the axis. We dismantled the Ilizarov frame after full consolidation of the proximal and distal corticotomized fragment and exercise therapy was continued for hip and knee joint.
All our treated hips were unstable and during treatment period we found superficial pin and wire infection in 3 cases and that were resolved by oral antibiotics and proper dressing weekly. The clinical evaluation included gait analysis and we used modified Harris hip score. At a mean follow up of 7 years LLD improved from a mean of 5,5cm to 0.8 cm. Modified Harris hip score improved from a mean of 50 points to 75 points. Ilizarov hip reconstruction can correct Trendelenburg gait and at the same time restore knee alignment and correct limb length discrepancy. Remodeling of the proximal osteotomy and development of LLD is expected when Ilizarov hip reconstruction is performed on a young patient.6
Anatomical and functional restoration of the limb were studied in 16 patients with defects of the proximal femur. It demonstrates high efficacy of the technique. Positive results were achieved in 92, 5% of the cases of femoral head and 94,5% of the patients treated for defects of femoral head and neck as well as the proximal femur. Summarizing anatomical and functional results we can say that all patients could walk with full weight bearing and they resumed their occupational activities and 3 persons continued their studies.5 Displaying hip (2 patients) in Figure 1 & Figure 2.
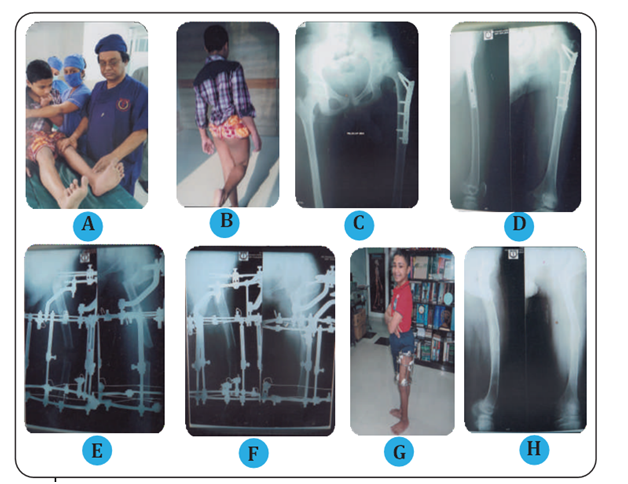
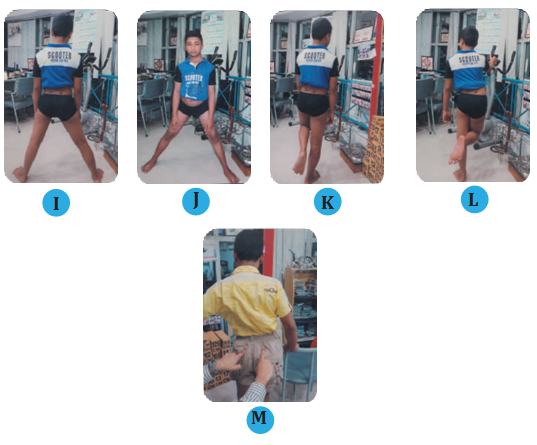
Figure 1
(A) Examining the patient, 14 years old child.
(B) Positive Trendelenburg sign.
(C, D) Radiograph of failed DDH of left hip with implant in situ.
(E) Post-operative radiograph after 3 weeks.
(F) Post-operative radiograph after 12 weeks.
(G) External view of Ilizarov apparatus in the hip and thigh.
(H) Final radiograph, 8 months after frame removal.
(I, J) 10 months after frame removal, showing equal leg length and normal alignment.
(K, L, M) Elimination or negative Trendelenburg sign.

Figure 2
(A, B) Images of a 21years old female with 3cm LLD.
(C) Positive Trendelenburg sign.
(D) Pre-operative AP pelvis, x-ray showing an absent of femoral head and proximal migration of the femur with residual sequelae of neonatal hip sepsis.
(E, F) Close up view of the proximal osteotomy and distal osteotomy. Showing the lengthening and the varus correction.
(G) Checking the Ilizarov apparatus.
(H) Patient with Ilizarov apparatus in the hip and thigh.
(I) Final radiograph, 9 months after frame removal.
(J, K, L) Back view, absent Trendelenburg sign.
(M) Increased abduction of right hip (Post-operating).
Hybrid transosseous osteosynthesis technique creating femoral support to acetabulum and correcting biomechanical limb axis and limb length allowed us to obtain positive results of treatment in 92,5% of observations. Functionally sufficient range of motion was preserved at the area of hip joint.Ilizarov hip reconstruction gives improvement in posture, gait and walking abilitywho have hip destroyed by neonatal sepsis through untreated DDH. Efficacy of differentiating application of the variants of femoral reconstruction has been confirmed by complete restoration of limb support in patients who used crutches or stick pre-operatively.11 Limb functioning condition was substantially improved in different groups during various periods of observations.It is evident that Ilizarov external fixator is the best tool for transosseous osteosynthesis which provides condition for controlled bone fixation and a possibility for reconstruction at any level of the involved bone segment.
Ilizarov hip reconstruction in children, adolescent and young adults with sequelae of neonatal hip sepsis or hip dislocation from dysplasia with the clinical problems of pain, Trendelenburg gait, LLD is a good choice which can be done in combination of pelvic support osteotomy and a second distal femoral osteotomy to correct length discrepancy and to realign the lower extremity.
None.
All authors declare no conflicts of interest.
None.

©2020 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.