MOJ
eISSN: 2374-6939


Research Article Volume 10 Issue 2
1Orthopedic surgeon and microsurgeon of the upper limb, Head of the Pediatric Orthopedics and Traumatology, Service of the University Teaching Hospital Dr. Dari
2Orthopedic surgeons members of the Pediatric Orthopedics and Traumatology, Service of the University Teaching Hospital ''Dr. Dar
Correspondence: Maximo Pericchi Eusebio, Orthopedic surgeon and microsurgeon of the upper limb, Head of the Pediatric Orthopedics and Traumatology, Service of the University Teaching Hospital ''Dr. Dario Contreras, Calle Padre Fantino Falco No.23, Ens. Naco. D.N. Santo Domingo, Dominican Republic, Tel 1 (809) 848 7889
Received: March 03, 2017 | Published: March 28, 2018
Citation: Eusebio MP, Morales EV, Mazzucco EF. Medical treatment for braquial obstetric palsy and “K” index for follow-up. MOJ Orthop Rheumatol. 2018;10(2):130–133. DOI: 10.15406/mojor.2018.10.00400
We present a conservative therapeutic proposal for obstetric brachial palsies and a visual index or marker to determine the state in which treatment was started and the evolution of patients over time. It involves direct infiltration into the brachial plexus affected with methylcobalamin and dexamethasone. We studied 48 patients divided into 4 groups and the short-term results were extraordinary in the group to which the mixture of both drugs was injected. The study was conducted at the Pediatric Orthopedics and Traumatology Service of the University Teaching Hospital "Dr. Darío Contreras "in Santo Domingo Este, Dominican Republic in the year 2013 and since then we are doing this treatment to all the children affected by this pathology that are referred to our consultation. We also developed a visual index for patient follow-up that is very easy to learn. It is the index K.
Keywords: brachial Plexus, brachial plexus palsy, obstetric palsy
From our training as orthopedists, we knew the anti-inflammatory effect of vitamin B12 used locally with lidocaine on enthesitis presented, especially by athletes. Then, we met Methylcobalamin (cobalamin, the active metabolite of B12 potentiated with methylo radicals) that we very effectively use in different enthesitis and tendinitis. We decided to use it on the peripheral nerves themselves such as the median, in compressive syndromes, the ulnar, radial and in lumbar and cervical root infiltrations with great success. This accumulated experience with Methylcobalamin, led us to research its way of acting on damaged nerve fiber and it is in 2011 that we started to use it in repairs and neurolysis in plexus surgeries in adults. Little by little we were using this molecule in obstetric lesions of the plexus under an informed consent protocol and we began to see results that we did not have before and in 2013 we decided to conduct a double-blind study to support this treatment.
We schematized the treatment by cycles of infiltrations and cycles of intramuscular injections as follows: A cycle of infiltrations consists of 5 direct infiltrations to the plexus, one per week, for 5 continuous weeks. They are deposited in each infiltration: 2 ampoules (2 cc) of Methylcobalamin plus an ampoule of 8 mg dexamethasone.
At the end of the 5 infiltrations, a cycle of 30 intramuscular injections of Methylcobalamin is indicated and clinically assessed.
When we started the protocol, we saw how children improved abduction and shoulder flexion and we came up with an index we call "K" that we also present in this article as a rapid follow-up element. 4 groups were established. Denominated Groups A, B, C and D. We chose 12 patients in each group and the same amount according to the type and severity of the lesion.
The inclusion criteria were:
The patients were recruited and evolved in our office at the Pediatric Traumatology and Orthopedic Service of the Dr. Darío Contreras University Teaching Hospital in the city of Santo Domingo Este, Dominican Republic, during the year 2013 and the first quarter of 2014.
Types of PBO chosen:
Index K
When we see a baby with an Erb, Extended Erb and Total type lesion, we will see that his upper extremity is down and straight as if it were a rod. If we start from this rod hangs from a point that is the shoulder, from this point to the upper end and to the lower end, an axis that goes from 0 to 180 degrees is described. The zero will be at the tip of the fingers with the limb hanging and the 180 degrees will be at the maximum abduction point of the shoulder. Then, if the child only abducts the shoulder by describing an axillary angle of 90 degrees and thus a horizontal axis; we will have two quadrants, one upper and one lower with respect to the vertical axis.
If the child only abducts up to 45 degrees, it points to an intermediate point between 0 degrees and 90 degrees. Thus, if the child recovers a lot and abducts to the midpoint of the upper quadrant, it will indicate that this point equals 135 degrees, thus forming a quick visual identification mark: 0, 45, 90, 135, 180 degrees. Take the vertical axis and project from the midpoint (shoulder) a line at each angle and it will be describing a K (Figure 1).
The infiltrations were performed by the anatomic repair technique both supraclavicular and infraclavicular. Supraclavicular technique: The two ends of the clavicle are marked and from the midpoint through a finger on top, a fine needle or a butterfly was introduced, directing its tip caudally at an angle of 80 degrees to contact the clavicle and in At that moment the medicine infiltrated.
Patients with Erb's palsy were infiltrated supraclavicularly. Those who suffered from Erb Extended were infiltrated supra and infraclavicular, equally to those who were totally affected.
The results were measured by:
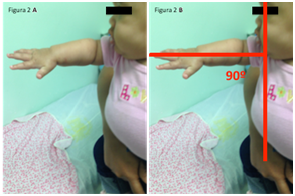
Figure 2 (A & B) 4-month-old girl who arrived with an Erb-type paralysis extended, that is, her shoulder was barely able to take off her body (K1). Figure 4 The elbow was extended and the wrist was flexed just like the legs. fingers, the typical waiter tip deformity. After the first cycle of infiltrations, his shoulder reached a K2 as shown in these photos. A month later, she was subjected to another cycle of a weekly infiltration for five consecutive weeks.
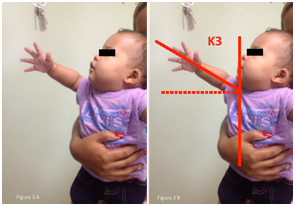
Figure 3 (A & B) The same girl with 6 months and a half and already has a K3, cured elbow wrist and fingers. We consider it cured however, we follow up on the consultations every two months, after completing the first year of life, it will be scheduled every three months and after the second year it will be seen by the consultation every 4 months, or three times a year.

Figure 4 (A & B) Another girl, 3 months old, who in Figure 4A, is on the stretcher in the room to receive anesthesia with naso-buccal mask and to be able to infiltrate her right plexus carrying a PBO type Erb Duchenne extended, canceling shoulder, elbow flexion and extension of wrist and fingers. In the following photographs, the 6-month-old girl, after a cycle of infiltrations, already has elbow, wrist and fingers; plus a K2 + index. The plus (+) is because it passes 90º with a great possibility of gaining greater mobility of the shoulder.
It is proposed, in the universal literature, that 60 to 66% of the high lesions of the plexus present a recovery of some degree, spontaneously. However, the study shows that with a treatment that provides biochemical elements that mediate neuronal deflation, repair and regeneration, the changes in favor of the reactivation of the nerve fiber are accelerated and the patient recovers a greater function than he would recover spontaneously. and with a considerable shortening of time.
In all the literature reviewed, we did not find any type of medical treatment administered before the first year of age, we only found treatments based on physiotherapy and, failing that, the surgical option. So that our treatment offers the possibility of having at hand a medical treatment easy to perform by expert hands and relatively inexpensive when compared to the cost of physiotherapy and not to mention the cost of surgery.
In the Internet, we find an interesting work done as a degree thesis, by Cruz Pedraja Sandra1 who after making a broad literature search, uses botulinum toxin to relax the contracted muscles, especially triceps brachii and biceps, However, it should be noted that this study was carried out on children who were sequenced over 2 years of age and who responded to the orders. In addition, the relaxation of contractures by the action of botulinum toxin does not improve the condition or structure of the nerve fiber.
The pioneers in the West of early microsurgery of the paralytic brachial plexus of birth, such as Narakas, Millesi, Gilbert, Tassin and others, have established a maxim for more than 20 years: "A child with PBO who does not flex at 3 months of age. The elbow should be operated "which, more and more, is modified by surgeons who are not as aggressive. We, for example, do not assess the indication of surgery for the time elapsed, since we began our medical treatment at 3 months of age, which is when the term of this maximum ends. Given that our treatment is applied by cycles of 5 infiltrations, one weekly for 5 weeks run, if the child does not respond with flexion of the elbow to 3 cycles of infiltrations, then we operate.
The index or indicator "K" is an easy tool to use and without complications. Some may point out that it closely resembles Gilbert's functional assessment test, but it is not, Professor Gilbert2 establishes a scale of 6 degrees where 0 corresponds to complete paralysis and 120 to an abduction of 120 degrees or more, with active external rotation. It is a motor scale equal to ours, only that our appreciation becomes visual, with the movements that the child makes with his affected shoulder. In our case (indicator K) 0 corresponds to no degree of abduction but not to complete paralysis, even if it has 0 degrees of abduction. As it turns out, a classic Erb's palsy can have 0 degree of abduction and it is not a total paralysis, it is a K0, but it has movements of its fingers and even the elbow, but not of the shoulder. Then, the same professor Gilbert, proposed another scale of assessment3 called: Gilbert's scale, which assesses the abduction and external rotation of the shoulder where it establishes six degrees where "0" is grade 0 without any type of movements, up to grade 5 where there is an abduction greater than 120 degrees and a complete active external rotation. It is, without a doubt, an excellent scale, but we consider that the one we propose is made almost immediately, visually, simply by observing the child on the lap of his mother or on the examining table.
Nor is it equal to the Movement Scale of the Hospital for Sick Children4 which establishes whether muscular contractions are made for or against gravity and whether it is greater or less than 50 degrees. The K index is ascending and strictly assesses the recovery evolution of the shoulder musculature, especially external rotation, abduction and flexion.
The Mallet Scale,5 although it measures the activity of the shoulder, is more applicable to children who obey orders and to older children, because it needs to make movements that a baby or a child under 3 can not do. However, this is the scale we use for the older patients and adults we operate.
We perform surgery when after two cycles of infiltration and results are not obtained.
Groups A and B were more successful with the treatment with Methylcobalamin, obtaining both, similar results, although group A was slightly better. Infiltration with Methylcobalamin plus dexamethasone turns out to be an adequate drug treatment to restore nerve fiber in infants and children under 3 years of age with Obstetric Brachial Palsy. The index or indicator "K" is easy to visualize and to establish its degree, since it is done to the naked eye without requiring anything else, being able to assess both for shoulder abduction and for flexion.
None.
Authors declare there is no conflict of interests in publising the article.

©2018 Eusebio, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.