MOJ
eISSN: 2374-6939


Research Article Volume 10 Issue 1
1Professor, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Prof., Russian Ilizarov Scientific Centre, Russia
2Professor, Bari-Ilizarov Orthopaedic Centre, Bangladesh
3Consultant, Bari-Ilizarov Orthopaedic Centre, Bangladesh
Correspondence: Bari MM, Chief Consultant, Bari-Ilizarov Orthopaedic Centre, Visiting and Honored Professor Russian Ilizarov Scientific Centre, Kurgan, Russia, Tel 8800000000000
Received: February 11, 2018 | Published: February 15, 2018
Citation: Bari MM, Shahidul I, Shetu NH, Mahfuzer RM (2018) Charcot’s Arthopathy in Diabetics: Treatment by Ilizarov Technique. MOJ Orthop Rheumatol 10(1): 00388. DOI: 10.15406/mojor.2018.10.00388
Treatment of Charcot’s joints with diabetic foot is a great challenging situation of soft tissues due to associated neuropathy and vascular compromise. Arthrodesis of the Neuropathic ankle joint is extremely difficult and associated with lot of complications. The use of the Ilizarov fixator in Charcot’s arthropathy is a disabling pathology of the foot and ankle which requires an effective treatment to improve clinical and functional outcomes and prevent foot amputatiaon ankle fusion for patients with neuropathic arthropathy is obscured we aimed to evaluate the results of the Ilizarov method for ankle arthrodesis in diabetic patients with Charcot’s arthropathy.1,2
From 1990 to 2017, 54 patients were performed surgeries (40 males, 14 females) with Ilizarov apparatus in diabetic foot patients with Charcot’s joints (Eichenholtz stage II and III). The mean age of patients was 56 (range 36-65 yrs.) of which all patients were diabetic. Deformity, resorption of bones and instability of the ankle joint that results in a non-plantigrade foot was considered as the operative indication.3 All the patients have been treated with open resection, partial intra surgery reduction, Ilizarov frame application and progressive correction of the residual deformities. The mean follow up time has been 36 months.
We observed that solid fusion was obtained in all 53 patients out of 54, at an average of 18 weeks duration (range, 14-20 weeks), excellent 40 good-10, fair-3, poor-1. No major complications occured.
Case-1 Diabetic foot Charcot joint arthropathy with DM with CKD (Figures 1-5).

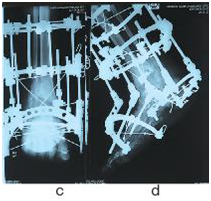
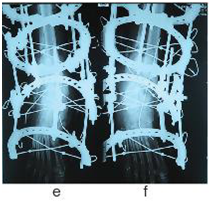
Figure 1 Pre-operative radiographic views (a,b) of a Charcot neuropathy ankle joint after an open reduction and internal fixation repair of an ankle fracture. There was a significant deformity with unstable ankle and deep infection. The patient underwent removal of internal hardware followed by primary ankle compression arthrodesis using Ilizarov fixator (c,d,e,f).
With the Ilizarov technique we achieved the restoration of the foot morphology, with a plantigrade foot in all cases and no deep infection or recurrent skin ulcerations; no amputation was required. This technique is best reserved for patients who are at the highest risk for complication or have failed with standard orthopaedic methods of internal fixation.4
The Ilizarov method provides a successful and effective method by using this biocompatible fine smooth and olive wires for management of diabetic foot with Charcot’s arthropathy associated with preexisting neural and vascular compromise as complications, especially when the use of internal fixation methods have its great limitations. In our series all patients were plantigrade with foot ulcers healed.
None.
None.

©2018 Bari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.